Bone, Connective Tissue, Joint and Vascular Biology, and Pathology
Linda A. Russell
Edward F. DiCarlo
Bone is composed primarily of an inanimate, calcified extracellular matrix with a small proportion of cells acting in a custodial role.
Diseases of the bones are the result of disturbed cellular function that interferes with the maintenance of mechanical function.
There are more than 14 types of collagen that comprise molecules in the extracellular matrix.
Joints are organ systems whose functions depend on the competence of all of the component parts—bone, cartilage, ligaments/tendons, and synovium.
Diarthrodial joints are composed of two articular surfaces that are bathed in synovial fluid and provide for stable and fluid motion.
Osteoarthritis is a manifestation of the mechanical failure of a joint resulting from failure of at least one of the joint components.
Rheumatoid arthritis (RA) is an example of the inflammatory destruction of a joint leading to stiffness and subsequent loss of function.
Skeletal muscle permits motion by generating force and the diseases are either intrinsic to the muscle, such as in inflammation and the dystrophies, or secondary due to vascular or neurologic conditions.
Several mechanisms are active in the development of vasculitis—but classification schemes are heavily dependent on clinical circumstances, the type and size of the involved vessels, and the type and degree of inflammation present.
The musculoskeletal system comprises the organs that permit the human body to move in a coordinated and stable manner. Bones, tendons, ligaments, and muscles comprise the primary organs of the system, and ancillary structures such as blood vessels, fascias,
and aponeuroses are included in the term “connective tissues”; all these structures have a connective tissue matrix that includes some form of collagen.
and aponeuroses are included in the term “connective tissues”; all these structures have a connective tissue matrix that includes some form of collagen.
The collagens comprise a set of molecules that provide the extracellular supporting framework for various tissues. More than 14 different collagens have been identified. Each collagen has a specific function. The structure of the collagen molecule is a triple helix.
Each collagen type has a specific amino acid sequence.
Type I collagen comprises 90% of collagen in the body and is the major constituent of skin, tendon, bone, synovium, cornea, conjunctiva, and sclera.
Type II collagen is found in cartilage.
Type III collagen is often found with type I collagen in skin, synovium, and vascular wall tissues.
Type IV collagen is found in basement membranes.
Type V collagen is found surrounding fibroblasts, smooth muscle cells, and other mesenchymal cells.
Type IX and XI collagens are found in cartilaginous tissues.
Bone is primarily composed of an inanimate extracellular matrix, with a lesser component of living cells present in a custodial role. Bone, cartilage, and teeth have the unique ability to calcify. Bones are produced as a result of two processes:
Endochondral ossification. Most bones are modeled in cartilage and develop by the orderly replacement of that cartilage with bone tissue. The processes of elongation and complex modeling of the ends of bones progress through endochondral ossification.
Membranous ossification. Bones, or regions of bones that do not develop through endochondral ossification, are produced by the intramembranous (periosteal) deposition of bone. The midregions of flat bones (e.g., calvarium, mandible, ribs, and ilium) and the cortical shafts of long bones are produced through this process.
Bone shape depends on anatomic location and the forces applied to the bone. All bones change their shape (grow) through some combination of endochondral ossification and membranous ossification—through processes that take place in the epiphyses, in the apophyses (e.g., the greater and lesser trochanters), and at the periosteal surfaces.
The ends of long bones and the complex edges of flat bones are composed of epiphyses and apophyses, which are modeled in cartilage, are capable of maintaining the complex shapes of the bone ends throughout development and growth, and are eventually replaced mostly by bone.
Adjacent to the epiphyses and apophyses, the growth plate provides for growth of the bone through endochondral ossification. Most growth plates fuse in the late teenage years when normal human growth ceases.
The midshaft of the long bones is the diaphysis and the transitional zone between the growth plate and the diaphysis is the metaphysis.
The outer portion of a bone is composed of a cortex or compact bone and the inner portion is the medullary cavity that contains variable amounts of cancellous or trabecular bone. The bone marrow is in the medullary cavity.
Within the diaphyseal shaft, the outer surface is referred to as the periosteum and the inner surface is called the endostium.
The ends of long bones that form a joint are covered in a layer of articular cartilage that does not calcify and persists throughout life.
The bone cells are of three types. Osteoblasts are responsible for bone formation. Osteoclasts are responsible for bone resorption. Osteocytes play a role in mineral and bone homeostasis. Appropriate clinical markers for these cell types and their associated activity are presented in Table 6-1.
Table 6-1 Bone Cell Types with Appropriate Clinical Markers and Associated Activity
Bone cell type
Function
Marker of bone remodeling
Osteoclast
Bone resorption
Urinary N-telopeptide, urinary C-telopeptide, deoxypyridinoline
Osteoblast
Bone formation
Bone alkaline phosphatase, osteocalcin
Osteocyte
Cell-to-cell communication
Unknown—none?
Bone remodeling is a process that occurs throughout life and permits repair of injured bone and maintenance of serum calcium-phosphorus homeostasis.
The bone matrix is composed of collagen fibers (primarily type I) and noncollagenous proteins that in normal bone are arranged in orderly layers resulting in “lamellar bone.” Crystals of hydroxyapatite are found on the collagen fibers and in the ground substance, which is composed of glycoproteins and proteoglycans.
Bone pathology can be seen in several conditions including fracture, osteoporosis, osteomalacia, and Paget’s disease.
Fractures occur in the setting of high-impact trauma or in pathologic states such as the metabolic bone diseases, osteogenesis imperfecta, and both primary and metastatic neoplasms.
Osteoporosis (see Chapter 53) is a systemic skeletal condition characterized by a reduction in the amount of bone to an extent that is sufficient to permit fracture during normal activity or after sustaining minimal trauma (i.e., fragility fracture). It leads to a condition where the rate of bone formation cannot keep pace with the rate of bone resorption, although both the rates may be reduced. This results in delicate, fragile trabeculae that are not well connected.
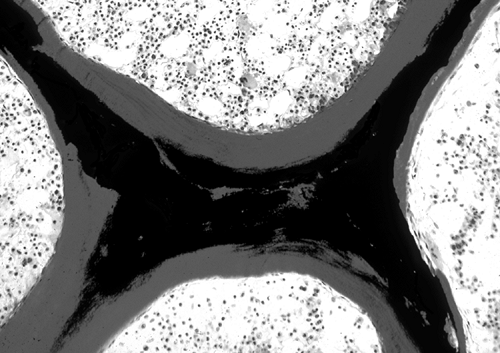
Osteomalacia (Fig. 6-1) refers to any systemic skeletal condition that is characterized by an excessive amount of unmineralized bone tissue called “osteoid.”
Osteomalacia appears with increased osteoid thickness and osteoid surface, coupled with a reduced or otherwise insufficient mineral apposition rate. Osteomalacia most commonly results from insufficient levels of calcium, phosphate, or vitamin D.
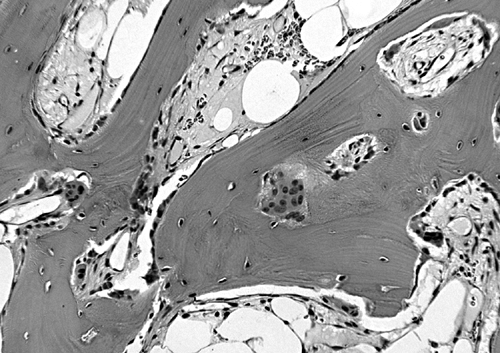
Figure 6-2. This photomicrograph of a decalcified section of bone in Paget’s disease shows numerous, variably sized osteoclasts and uniform small osteoblasts aligned along the surfaces of irregular bony trabeculae. The result is derangement of the trabecular and matrix architecture with loss of mechanical integrity (hematoxylin–eosin, H&E ×25).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access