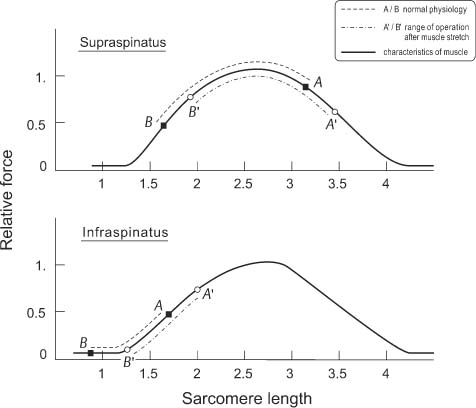
1 Biomechanics of Pathophysiology and Repair of Rotator Cuff Tears Rotator cuff (RC) muscles are an integral part of the shoulder. The RC provides the torque needed to move the joint as well as the force to stabilize the joint. RC ruptures are frequently associated with loss of strength and stability of the shoulder. Biomechanical studies have been performed to explore the potential etiology of the injury and to assess various treatment modalities. In this chapter, I will discuss the basic concepts that relate to the RC muscle function and injury, along with the biomechanical considerations for the treatment of shoulders with RC deficiency. The function of muscle as a joint mover depends on the muscle’s physiology and its mechanical efficiency. The physiological cross-sectional area represents the effective size of the muscle, which determines the ability of the muscle to generate force. The physiological cross-sectional area is not simply the area of a given muscle cross-section, but the cross-section of the muscle fibers as calculated by dividing the muscle volume with the fiber length. The physiological cross-sectional area of the RC muscles has been studied and reported in the literature.1,2 The physiological cross-sectional areas for the subscapularis, supraspinatus, infraspinatus and teres minor muscles combined are 16.30, 5.72, and 13.75 cm2, respectively. The combined RC muscles contribute almost 35% of the physiological cross-sectional area of all the muscles crossing the shoulder joint.1 Within the RC, the contributions of each muscle are 53, 10, 22, and 14% for the subscapularis, teres minor, infraspinatus, and supraspinatus muscles, respectively.2 In addition to the physiological cross-sectional area, the potential muscle contractile force further depends on muscle length at contraction. As illustrated in the muscle length-tension relationship, the peak muscle force is generated when the sarcomere is near optimal length (Fig. 1–1). Excessive shortening of the sarcomere reduces the force generation as indicated by the ascending limb of the length-tension curve on the left. On the contrary, excessive sarcomere lengthening reduces force generation, as shown by the descending limb on the right. Such length-tension relationship needs to be considered in RC tear repair. The supraspinatus muscle normally operates in the range near the plateau of the length-tension curve, where A represents the muscle at elongated length when the arm is in the dependent position, and B represents the shortened muscle length when the arm is in full abduction. In the cuff repair, stretching of the tendon and muscle is usually required to reattach the muscle to the tuberosity. Such stretching will shift the physiological range of operation to the right on the length-tension curve between A′ B′. With such a shift, the force generation potential with the arm at the dependent position is, therefore, compromised. Such reduction in force generation could be clinically critical because the RC muscles are instrumental in initiating abduction motion. To avoid such a stretching effect, a patch graft could be utilized to maintain the proper length-tension relationship. On the other hand, the infraspinatus muscle normally operates in the ascending limb of the length-tension curve. Therefore, any stretch of the tendon and muscle of infra-spinatus in the repair of defect will shift the range of function from AB to A′ B′, which will not compromise the force generation of the muscle. Figure 1–1 Potential muscle contractile force depends on muscle length. The supraspinatus muscle normally operates in the range near the plateau of the length-tension curve, where A represents the muscle at elongated length when the arm is in the dependent position, and B represents the shortened muscle length when the arm is in full abduction. Stretch of the tendon will shift the physiological range of operation to the right on the length-tension curve between A´ B´. On the other hand, the infraspinatus muscle normally operates in the ascending limb of the length-tension curve. The moment arm (MA) further determines the mechanical efficiency of the muscle force in generating torque around a joint. In general, the MA about different axes of rotation for a given joint varies with joint posture. Geometrically, the MA is measured as the shortest distance between the line of action of the muscle and the axis or center of rotation of the joint. Experimentally, it is difficult to have an accurate assessment of the MA in such measurement due to the errors in defining the line of action as well as the joint center of rotation. Alternatively, the MA could be determined based on an intimate relationship among these three parameters.3 The instantaneous MA (r) or mechanical advantage of a tendon can be related to the tendon excursion (E) and the joint rotation (φ) as: This concept has been used extensively in the past for accurately assessing the muscle and tendon MAs in physiological and pathological conditions. Based on the above principle, the MAs of infraspinatus and subscapularis muscles were noted to contribute not only to external rotation (ER) and internal rotation (IR), respectively, but also to the elevation of the arm in the plane of the scapula, a role for which these muscles has been given little or no consideration.4 The contribution of the infraspinatus muscle to abduction is enhanced with IR, whereas that of the subscapularis muscle is enhanced with ER. Thus elevation of the arm in the dysfunction of the supraspinatus muscle could potentially be compensated by the remaining RC muscle through proper rehabilitation and strengthening.4 The subscapularis muscle is a more important elevator in the scapular plane than either the supraspinatus or infraspinatus muscle, especially in the latter phases of motion.5 Axial humeral rotation is an important movement commonly performed during activities of daily living and is a targeted motion of shoulder rehabilitation, particularly in those protocols emphasizing RC strengthening.6 With the humerus in neutral or elevated positions, the infraspinatus is the most powerful external rotator, followed by teres minor. The subscapularis muscle is the most effective internal rotator in this position. RC tears are frequently associated with loss of shoulder strength. The tendon detachments, tendon defects, and muscle retractions of supraspinatus and infraspinatus disturb the force transmission to the humerus and torque generation by the RC. In two studies, these effects on force transmission and joint torque were measured in various types of simulated defects using cadaver specimens. Detachment or creation of a defect involving up to two thirds of the supraspinatus tendon resulted in a minor reduction in the force transmitted by the RC. Creation of a defect involving the whole supraspinatus tendon resulted in a moderate reduction. However, a simulated muscle retraction involving one-third and two-thirds of supraspinatus tendon, as well as the whole supraspinatus tendon resulted in losses of torque of 19, 36, and 58%, respectively. These findings support the rotator cable concept that corresponds to the clinical observation that patients with a small rupture of the RC might present without a loss of shoulder strength. Muscle retraction is potentially an important factor responsible for the loss of shoulder strength following large RC ruptures.7 RC ruptures that extend into the infraspinatus tendon may cause dysfunction. One study was performed to determine whether a threshold size of infraspinatus defect exists, beyond which abduction torque generation decreases substantially.8 It was found that the glenohumeral abduction torque progressively decreased with greater infraspinatus detachment. When detachment extended to three-fifths of the infraspinatus, abduction torque reduced 52% of the intact condition, which was a significantly larger reduction compared to supraspinatus release alone. The inferior portion of infraspinatus, which includes the rotator cable insertion, plays a role in transmitting the compression forces across the glenohumeral joint.8 In the repair of rotator cuff tears, the torn tendon cannot always be freed adequately to permit reattachment at its original anatomical insertion site. An option is to advance the site of insertion medially and reattach the tendon to a trough in the sulcus or to the humeral head. The biomechanical effects of such medial advancement on the MA of the supraspinatus muscle during glenohumeral elevation were studied using fresh-frozen shoulders from cadavera.9 Medial advancement of the site of insertion of the supraspinatus tendon was simulated by the placement of suture anchors in the sulcus of the proximal part of the humerus at points 3, 10, and 17 mm medial to the junction of the supraspinatus tendon and the bone. Three and 10 mm of medial advancement of the tendon had a minimum effect on the MA during elevation compared with the value determined for the intact condition. However, 17 mm of medial advancement was found to reduce the MA significantly. Superior transposition of the subscapularis tendon has been recommended for surgical repair of massive tears of the RC. Superior transposition of the subscapularis tendon significantly increased its abduction MA.10 The effect was optimal when the simulated insertion site was lateral rather than medial and, to a lesser extent, anterior versus posterior. The results provided a biomechanical rationale for subscapularis tendon transposition in restoring the loss of abduction strength of the shoulder in a massive cuff tear. Repair of large defects for RC tears associated with muscle retraction is sometimes impossible. Biological or synthetic patch graft has been proposed for the coverage and restoration of the anatomy for load transfer. In one study, a simulated supraspinatus tendon defect and retraction, and patch repair was performed.11 A patch graft was inserted into the defect and the effects of reattachment to the greater tuberosity, narrowing of the defect by using a smaller graft, and anterior graft attachment (rotator interval tissue versus subscapularis) were investigated (Fig. 1–2
The Rotator Cuff as Joint Mover

Effects of Injury and Repair of Rotator Cuff Tears on Joint Torque
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree