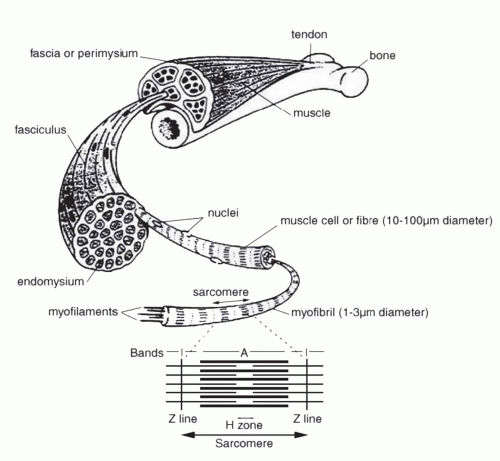
The basic units of skeletal muscle include sarcomeres, myofilaments, myofibrils (basic units of contraction), muscle fibers (cells), fascicles (bundles of about 150 muscle fibers each), and a muscle (Fig. 5.1). Sarcomeres, areas from Z line to Z line and functional contraction units of myofibrils, contain two types of myofilaments: thick (myosin) and thin (actin) myofilaments, which are repeated throughout muscle myofibrils.
Other structures within sarcomeres are I bands, A bands, Hzones (absence of actin), and M bands (sarcomere’s center). Transverse tubules (T tubules; see Excitation-Contraction Coupling), found at the A-I junction of sarcomeres, and the sarcoplasmic reticulum (SR) are the primary regulators of calcium influx into muscle units. The sarcolemma is the muscle cell membrane.
Satellite cells are muscle “stem” cells. They are activated to a full cell cycle from the quiescent state in response to heavy resistance training and cell damage. Activation of satellite cells is necessary for normal growth and regeneration of tissue damage. Insulin growth factor-1 (IGF-1) is a primary regulator of satellite cells (27,28).
Key muscle proteins include actin, myosin, troponin, and tropomyosin. Actin and myosin constitute myofilaments within myofibrils; myosin is the site of adenosine triphosphate (ATP) binding. Troponin complexes on actin molecules are the calcium binding sites for initiating contraction. Tropomyosin, found in thin filaments of muscle fibers, inhibits contraction until modified by troponin.
Alpha and gamma motor neurons initiate and regulate muscle contraction. Alpha motor neurons initiate contractions in contractile (extrafusal) fibers, whereas gamma neurons innervate muscle spindle (intrafusal) fibers of muscle.
Motor units (basic functional unit of movement) consist of alpha motor neurons, synaptic junctions (motor endplate), and the muscle fibers they innervate.
One motor neuron can innervate 10 to several thousand muscle fibers. Release of acetylcholine by neurons initiates contraction, and degradation of acetylcholine by cholinesterase terminates action potentials.
Muscle contraction is triggered by an electrical impulse involving acetylcholine release, arrival of the impulse at the sarcolemma (after crossing the synaptic junction), and subsequent entry of calcium into myofibrils. Electrical impulses travel quickly into the interior of muscle cells, down the T tubules with release of calcium from the SR to myofibrils.
Once calcium stores are released from the SR, a nonstoppable contraction is initiated: Calcium entry activates crossbridge linkages and contraction of sarcomeres.
Sliding-Filament Theory: This theory states that muscle contraction occurs when two major myofilaments (actin and myosin) slide past one another through a series of crossbridge linkages. Myosin crossbridge linkages combine, detach, and recombine in an oscillatory pattern such that at any point in time about 50% of myosin heads are attached to actin binding sites. No myofilament actually changes length.
All or None Law: A motor neuron initiating an action potential will contract all muscle fibers innervated by that motor neuron simultaneously. Muscle fibers achieve gradation of contraction strength by recruiting fewer or more motor neurons to initiate contraction and/or by changing the frequency of action potentials to sustain contractions.
Muscle Spindles: These specialized intrafusal muscle fibers are located between and among extrafusal fibers deep within the interior of muscles. These proprioceptors sense and relay the length or velocity of muscle movement (e.g., patellar reflex).
Skeletal muscle fiber types are characterized by differences in morphology, histochemistry, enzyme activity, surface characteristics, and functional capacity (17,18,19,23,24,27) (Table 5.1).
Table 5.1 Characteristics of Major Skeletal Muscle Fiber Types*
Fiber Characteristics
Slow Twitch
Fast Twitch
Type I
Type IIa
Type IIx
Other Terminology
Slow Oxidative (SO)
Fast Oxidative Glycolytic (FOG)
Fast Glycolytic (FG)
Aerobic Capacity
High
Med/High
Low
Glycolytic Capacity
Low
High
High
Myoglobin Content
High
Med
Low
Color
Red
Red
Pink/White
Fatigue Resistance
High
Med
Low
Glycogen Content
Low
Med
High
Triglyceride Content
High
Med
Low
Time to Peak Tension
Slow
Med
High
Myosin ATPase Activity
Low
Med
Med
Myosin Heavy Chain (MHC)
MHCIβ
MHCIIa
MHCIIx
Tension Cost*
Low
Med
Med
ATP/ADP
Low
Med
Med
ADP, adenosine diphosphate; ATP, adenosine triphosphate; Med, medium.
This chart represents current nomenclature for human skeletal muscle fiber types. Type IIb human muscle fibers are currently referred to as Type IIx because of the MHCIIx isoform found in human muscle. Type IIb muscle fibers are found in rodents and other species, with MHCIIb (19,21,22,23).
*Tension cost = ATPase activity to isometric tension ratio.
Human muscle fiber types include Type I, IIa, and IIx, due to the expression of different myosin heavy chain (MHC) forms (18,21,22,24).
Distribution of Type I (slow twitch) and Type II (fast twitch) fibers within normal populations depends on many factors
and shows extraordinary adaptive potential in response to innervation/neuronal activity, hormones, neural signaling, training, functional demands, and aging (19).
Minute ventilation ([V with dot above]E) is the total volume of air moved into and out of the lungs each minute; it is a function of tidal volume (VT) and respiratory rate (fB).
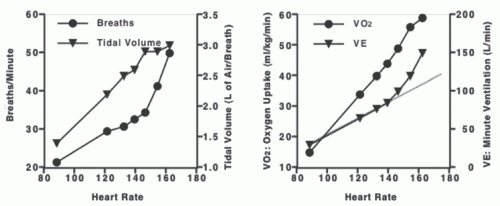
At rest, [V with dot above]E is between 5 and 7 L · min−1, whereas during exercise it increases to between 60 and 180 L · min−1, depending on the health of the person (Fig. 5.2). VT increases by expanding both inspiratory and expiratory volumes; these “extra” volumes are called inspiratory and expiratory reserve volumes (IRV and ERV), respectively. The increase in VT allows [V with dot above]E to increase 5- to 10-fold during exercise. An increase in fB further augments [V with dot above]E (1,2,26).
MVV is the volume of air exchanged during repeated maximal respirations in a specified time (10-15 seconds). It is expressed as L · min−1 and represents a measure of maximum breathing capacity for comparing to maximal [V with dot above]E during exercise ([V with dot above]Emax).
BR is the difference between MVV and [V with dot above]Emax and is sometimes expressed as [V with dot above]Emax/MVV; it is the additional ventilation available during maximal exercise. If a person achieves maximal work capacity prior to attaining MVV, the person has a normal BR, whereas if MVV = [V with dot above]E, the person may have compromised pulmonary function. A typical BR is 11 L · min−1, with normal [V with dot above]Emax/MVV ranging between 60% and 75%.
Oxygen uptake ([V with dot above]O2), based on the Fick equation, can be expressed as: [V with dot above]O2 = CO × (a − vO2) = HR × SV × (a – vO2), where CO is cardiac output, a – vO2 is arteriovenous O2 content difference, SV is stroke volume, and HR is heart rate. For an average 70-kg adult, CO is about 5 L · min−1 at rest and can increase to 20 to 30 L · min−1 during strenuous exercise.
[V with dot above]O2, determined during exercise by measuring respiratory gases, is related to the fractional percent of O2 in inspired and expired air and [V with dot above]E. Inspired air contains 20.93% O2 and expired air around 17.0%.
[V with dot above]O2 is usually expressed in absolute units (L · min−1) or relative to body weight (mL · kg−1 · min−1). Resting [V with dot above]O2 ranges from 0.25 to 0.4 L · min−1, and maximal exercise [V with dot above]O2 values can exceed 5.0 L · min−1 (15-70 mL · kg−1 · min−1) (Fig. 5.2). Higher relative values indicate higher aerobic fitness.
Carbon dioxide (CO2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree