CHAPTER 16 Basic science on somatovisceral interactions
peripheral and central evidence base and implications for research
Introduction
The basic philosophy of osteopathic medicine is a ‘whole-person’ approach to care and to the understanding of the integrative functioning of the body. This approach is also the basis of so-called ‘holistic’ or ‘integrative’ medicine (see Chapter 1). It is included both implicitly and explicitly in all manual therapy or other physical interventions directed at the body in the treatment of dysfunctional states (as practiced by chiropractors, physical therapists, massage therapists, and others). This approach uses the biological mechanisms of the body and brain to correct the pathophysiological regulations of the body tissues (see Chapter 1). Beal (1985) described this focus in a more practical and direct way: ‘The concept of viscerosomatic reflexes reflects the strong interest of the osteopathic profession in the relationship of the musculoskeletal system in health and disease. It was apparent to early practitioners in the profession that somatic dysfunction was the result of multiple factors – somatic, visceral, and psychologic…. [Thus] The osteopathic profession has held certain basic tenets to be true – that altered or impaired function frequently occurs in the somatic system, that these somatic components may be manifest as presymptomatic signs of disease, and that they may be expressed as local or remote effects of dysfunction as somatovisceral or viscerosomatic reflexes. … [Therefore] osteopathic manipulative treatment of viscerosomatic reflexes has been advocated on the basis that it is designed to reduce somatic dysfunction, to interrupt the viscerosomatic reflex arcs, to influence the viscus through stimulation of somatovisceral effects, and to reduce the potential preconditioning effect of somatic dysfunctions to body stressors’.
The physiological and hence also the pathophysiological regulation of body tissues involves the brain and its reciprocal communications with the body. The efferent pathways from the brain are the somatomotor, autonomic, and neuroendocrine systems. The afferent pathways from the body tissues to the brain are the large groups of small-diameter (Aδ- and C-) afferents, which monitor the mechanical, thermal, metabolic, and inflammatory states of the tissues (see Chapter 2 and Fig. 2.1).
Manual and other physical interventions at the somatic body tissues do affect the target tissues locally, independent of their innervation on one side (see Chapter 6) and the somatic afferent innervation of these tissues on the other. The consequences of these therapeutic interventions are complex, as stimulation of the afferent neurons activates (1) reflex circuits in the spinal cord, brain stem, and hypothalamus involved in regulation of somatomotor, autonomic, and endocrine systems; (2) neural pathways and centers related to interoceptive body sensations, which include pain, heat, and other sensations from the skin, and pain and other sensations from deep somatic tissues and viscera; and (3) neural circuits related to affective (emotional) feelings.
How do we bring these levels of neural integration together to understand the mechanisms underlying the potentially curative effects of manual interventions on functional disorders in the deep somatic and visceral body domains? Some mechanisms underlying the neural processes potentially operating during manual therapy are discussed in the chapters of this book. Here I will critically discuss the experimental measurements and clinical observations on which the concepts of somatic dysfunction and the dysfunctional spinal segment are based. This includes the concept of somatovisceral interactions. I will concentrate particularly on the spinal autonomic (largely sympathetic) systems. Then I will summarize some aspects of the integrative functions of the spinal cord and potential mechanisms underlying chronic deep somatic and visceral pain. Finally, I will discuss the role of positive feedback mechanisms involving the somatomotor and spinal autonomic systems. I will not address the philosophical superstructure of osteopathic medicine that is related to ‘spirit, mind, brain and body’ (but see Introduction and Figure 2.1 in Chapter 2).
Systems and mechanisms involved in manual therapy
Various systems believed to be important in understanding the effectiveness of manual therapy in osteopathic medicine (but also in other medical fields independent of osteopathic medicine) and various underlying mechanisms have been discussed in this book. The common theme in all chapters (with the exception of Chapter 6) is that the integrative action of the central nervous system (which includes the spinal cord!) stands in the center to provide the mechanisms operating in manual therapy. Here I highlight the main topics that have been discussed:
Somatic dysfunction and the spinal segmental dysfunction
The scientific basis of osteopathic medicine is related to pathobiological1 processes in deep somatic tissues, in particular of the spine, and in the viscera; to the role of the afferent and efferent (somatomotor and autonomic) innervation of the diseased tissues; to the integrative neural processes in the spinal cord; and to supraspinal control. This is reflected in the osteopathic practice that consists – to put it simply – of the diagnosis and treatment of (1) structural changes in deep somatic tissues of the spine; (2) restricted mobility of skeletal muscle, joints, and fascia; and (3) changes in soft tissue consisting of alterations of local circulation, muscle tone, deep tissue sensitivity (discomfort and pain); and texture of deep tissues (‘trophic changes’) (Johnston 1992, Patriquin 2003; see Chapter 12). Interactions occur between the neural and non-neural components, between different deep somatic compartments, between deep somatic and visceral tissues, and between spinal and supraspinal neural circuits. Improvements in the diagnosis and treatment of functional diseases depend greatly on our understanding of the mechanisms of these interactions. In the center of both stands the concept of somatic dysfunction (previously called osteopathic lesion) and the concept of spinal segmental dysfunction (also called lesioned segment, or dysfunctional segment or facilitated segment).
The scientific basis of the ‘philosophy of osteopathy’ as it is propagated today (Chila 2010; Chapter 1 in this book) was first formulated in its full extent by Korr in 1947 and 1948, and has remained practically unchanged up to the present (Korr 1947, 1948, 1955a,b, 1978, 1979). For example, his keynote article published in 1948 in the Journal of the American Osteopathic Association was reprinted in the same journal in 2000 without further comments or interpretations in the light of modern research.2 Korr himself has directed and conducted research in this field, in particular related to spinal sympathetic outflow, in order to give support to his concept (Korr et al. 1958, 1962, 1964, Wright et al. 1960). Korr’s scientific ideas and research are mainly rooted in the experimental work of Denslow on the somatomotor system (Denslow 1944; Denslow & Clough 1941; Denslow & Hassett 1942; Denslow et al. 1947) and in the experimental work of Kellgren and Lewis on referred pain and hyperalgesia in the deep somatic tissues and viscera (Kellgren 1938, 1939, 1940, Lewis & Kellgren 1939, Lewis 1942).
The neural concept underlying osteopathic medicine
In the paper ‘The neural basis of the osteopathic lesion’, Korr (1947) states (I quote this because it makes clear what Korr foreshadowed in his future research and in his overall concept [bold and explanations in squared brackets are from me]):
Four of the main principles in osteopathy appear to be:
After an extensive discussion Korr concludes:
Under the heading Manipulative Therapy at the end of the paper, Korr states:
…Since the excessive tendinous and muscular tension produced around a joint, let us say, by some bony displacement tends reflexly to produce more tension, the manipulative easing of tension breaks a vicious cycle [involving skeletal muscle, its afferent and efferent innervation, and the spinal cord; see pages 289–291].
What is stated here in one of the first papers by Korr was repeatedly formulated by him in the subsequent 30 years (see, for example, Korr 1978). Korr and co-workers developed their own methods to record the electrical skin response (dependent on the activity in sudomotor neurons [Thomas & Korr 1951, 1957, Thomas et al. 1958]), and the blood flow through skin (dependent on activity in cutaneous vasomotor neurons [Wright et al. 1960, Wright & Korr 1965]). Korr (1951) endeavored to develop methods to measure:
Korr hoped to work out why manual therapeutic interventions can be successful and how these interventions can be optimized to generate better and mechanism-based manual treatments. This was a modern research concept. Korr was fully aware that the main problems to be solved are (1) to work out the mechanism of the lesion process (preferentially in the skeletomotor system of the spine); (2) to learn about as to how this lesion process develops over time, i.e. to study its development under chronic conditions; and (3) how this lesion process is modulated (enhanced or attenuated) by supraspinal centers, in particular the telencephalon (Korr 1951).
Korr’s conclusions
Korr’s concept in the light of modern neurobiological research
Is Korr’s concept, which is at the heart of teaching, diagnosis, and treatment in osteopathic medicine (Lederman 2000), supported by modern neurobiological research? Here I will raise some critical questions in the light of such research conducted in the fields of pain and the autonomic nervous system. These critical remarks do not belittle what Korr has tried to achieve: Korr was modern in his time, as he tried to formulate testable scientific questions.
The spinal cord as integrative organ
Organization of the spinal cord and its output systems
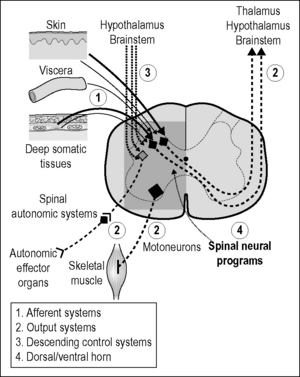
In Chapters 2 and 7 it was emphasized that the spinal cord is an integrative organ in its own right in the regulation of activity in spinal preganglionic neurons, and hence in the neural regulation of autonomic effector organs by spinal autonomic systems. The same principle applies to the regulation of activity in somatomotor neurons and hence of skeletal muscles. Thus the spinal cord contains a wealth of excitatory and inhibitory interneurons (segmental, propriospinal) which are involved in the following functions (Fig. 16.1):
The number of spinal interneurons (segmental and propriospinal) outnumber the number of spinal output neurons (motor neurons, preganglionic neurons, neurons projecting to supraspinal centers in brain stem, hypothalamus, and thalamus [ascending tract neurons]) by one order of magnitude (Polgar et al. 2004, Spike et al. 2003), indicating how important these interneurons are in the integrative activity of the spinal cord. Furthermore, in primates (and probably other mammalian species as well) the number of supraspinal neurons projecting to the spinal cord is probably much higher than the number of ascending tract neurons projecting to supraspinal centers, indicating how powerful the supraspinal control of spinal circuits is. This is also reflected in the fact that the volume of the spinal cord is about 2% of the volume of the brain in primates, but 35% in the rat (Swanson 1995). This argues that top-down control by the telencephalon is becoming quantitatively more important with the encephalization in evolution. It does not argue that the results we obtained in research on rodents do not apply to humans.
The dorsal horn of the spinal cord (and the trigeminal nucleus) can be divided functionally into three parts (Craig 2003a, 2008a, Dostrovsky & Craig 2006). This subdivision is somewhat speculative and not generally accepted. However, it helps to distinguish integrative aspects of interoception3 (pain in the three body domains, thermal sensations, other sensations of the skin [e.g., itch, sensual touch], sensations of the deep somatic tissues, visceral sensations, etc.), of exteroception (pressure, touch, vibration), and of regulation of somatomotor neurons and spinal preganglionic neurons:
These data and neurophysiological studies of spinal autonomic systems (see Chapter 2 in this book and Chapters 4 and 9 in Jänig 2006) strongly argue that the spinal cord contains the neural machineries that could explain the reciprocal relations between the three body domains (skin, deep somatic tissues, viscera). Thus they could explain:
Functional plastic changes of dorsal horn neurons in the spinal cord
Inflammation of peripheral tissues leads to sensitization of nociceptive primary afferent neurons (Fig. 16.2). This is reflected in the following changes of the nociceptive afferent neurons: development of ongoing (spontaneous) activity; decreased activation threshold and larger responses upon mechanical or thermal stimulation; and recruitment of mechanoinsensitive (silent) afferent neurons with unmyelinated axons. The cellular and subcellular (molecular) mechanisms of this sensitization are partially known, at least for the acute phase of sensitization (Hucho & Levine 2007, Julius & McCleskey 2006, Meyer et al. 2006, Ringkamp & Meyer 2009, Woolf & Ma 2007). However, it is debated whether the mechanisms of sensitization are the same in the chronic stage.
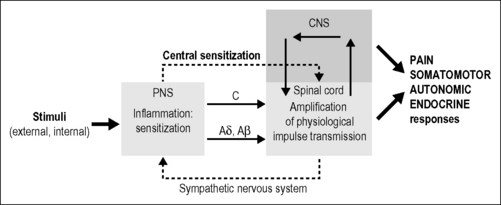
The pain is always associated with motor, autonomic, and endocrine responses. The upper interrupted arrow indicates that the central changes are generated (and possibly maintained) by persistent activity of nociceptors with unmyelinated (C-) fibers (e.g., during chronic inflammation) called here ‘central sensitization’. The lower interrupted arrow indicates the potential efferent feedback via the sympathetic nervous system (including the sympathoadrenal system) (see Fig. 16.4). The transmission of nociceptive impulses is under multiple control of the brain (arrows upper right). The sensitization of nociceptors entails sensitization of central neurons (e.g., in the dorsal horn) and changes of the central representations (of the somatosensory system) which may become irreversible. The central changes, induced by persistent activity in afferent nociceptive neurons, are also reflected in the activity of sympathetic systems and somatomotor systems that may establish positive feedback loops to the primary afferent neurons. CNS, central nervous system; PNS, peripheral nervous system.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree