Balance testing and training
Diane M. Wrisley and Timothy L. Kauffman
Introduction
The medical and sociologic consequences of falls in the older adult are one of the largest worldwide public health issues. It is estimated that 28–35% of persons over 65 years of age fall each year and this increases to 32–42% for persons over 70 years and fatalities are greatest in the over 85 age group (WHO, 2007). Falls in the elderly are multifactorial and have been attributed to medication use, environmental challenges, cardiopulmonary compromise, cognitive changes, frailty and sensory and motor deficits (WHO, 2007; Tom et al., 2013).
Once an older adult falls, changes occur (e.g. fear of falling, decreased mobility, speed, and fluency of movement) that increase their risk of falling. Therefore, it is essential that the geriatric specialist performs a thorough multifactorial balance evaluation and initiates treatment as early as possible. Definitions of key terms concerned with balance are included in Box 59.1.
Physiology of balance
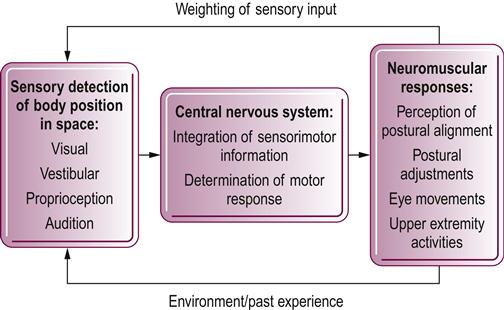
Balance, the ability to maintain the center of gravity over the base of support within a given sensory environment, is composed of several subcomponents and influenced by several systems. Human balance is a complex neuromusculoskeletal process involving the sensory detection of body motions, integration of sensorimotor information within the central nervous system (CNS), and programming and execution of the appropriate neuromuscular responses. Figure 59.1 summarizes the organization of the human balance system. The brain uses visual, vestibular, and somatosensory systems to determine the body position and movement in space. Although there are age-related changes in these systems, older adults do not display increased postural sway compared with younger adults when standing or walking when they have all three senses available (Woollacott et al., 1986). When older adults are first asked to balance on a posture platform under conditions of minimized somatosensory and visual input, half lose their balance (Woollacott et al., 1986). With repeated exposure, however, they are able to learn to maintain their balance on the platform (Woollacott et al., 1986). Interestingly, on further investigation, it was found that the falls correlated positively with subclinical pathologies in either the sensory or the motor systems (Woollacott et al., 1986).
As sensory changes are common in older adults, the reader is referred to additional chapters in this text on peripheral neuropathies (Chapters 32 and 33) and sensory changes in visual (see Chapter 51), somatosensory (see Chapter 49) and vestibular (see Chapters 52 and 58) systems for further evaluation and treatment techniques for these systems that will affect balance.
The information from the various sensory systems is relayed to the CNS and is integrated in several areas including the vestibular nuclei and the cerebellum prior to the generation of appropriate motor responses. Prioritization of use of sensory information for use by the CNS is most likely based on the availability of a particular sensory modality, the task at hand and past experiences (Peterka, 2002). The CNS then generates the appropriate motor responses to maintain upright body posture. Various balance strategies are thought to maintain balance depending on the speed of perturbation and the support surface. Slow, small perturbations on level surfaces result in muscle activity that is sequenced from distal to proximal (ankle strategy), while perturbations that are larger, faster, or on smaller surfaces result in muscle sequences from proximal to distal (hip strategy) (Nashner, 1994). A stepping strategy is used when the perturbations take the center of gravity outside the base of support or limits of stability and is used to recover balance (Nashner, 1994). Older adults frequently switch from an ankle strategy to a hip strategy during different conditions such as walking on slippery surfaces or with smaller, slower perturbations (Horak, 2006). Use of inappropriate balance strategies may contribute to falls in older adults.
There are many other factors that contribute to the ability to maintain an upright posture. First, musculoskeletal constraints must be met. Adequate range of motion (ROM) must be available, especially in crucial joints such as the ankle and hip. Impaired ROM of the neck or painful syndromes in the cervical muscles may lead to an altered representation of trunk and head movement and therefore cause imbalance. The proper generation of neuromuscular force is also essential to developing the appropriate balance strategies. The ability to sequence the muscles appropriately and the timing of the muscle activity are crucial and are sometimes the most difficult to retrain following injury (Horak & Shumway-Cook, 1990). When automatic postural responses are examined, older adults demonstrate slowed onset and reversal in normal distal to proximal sequencing of muscle activation compared with younger adults (Woollacott, 1990). Posture or alignment of bony segments can either assist with the production of the balance responses or make it more difficult to generate balance reactions. Maximizing a patient’s postural alignment can assist in regaining their ability to generate balance responses (Horak & Shumway-Cook, 1990). Although most of our balance reactions occur at a subconscious level, a patient’s cognitive status can influence their ability to generate the balance reactions necessary to maintain an upright posture. If a subject is easily distracted or has slow processing, he or she may not be able to react quickly enough to environmental changes to allow them to stay upright. This may be especially true if there is increased activity in the environment, if the patient is distracted by conversation, or if they are preoccupied (Horak, 2006). Many environmental factors can affect a patient’s ability to maintain balance. Decreased or absent lighting, and soft, pliable surfaces decrease the sensory input available to the patient for spatial orientation. Small children or pets underfoot can cause sudden perturbations and make it difficult for a patient to maintain balance, especially if they already have an increased reaction time. Many classifications of medications, ranging from diuretics to CNS suppressants, can also impair a patient’s ability to balance (WHO, 2007; Kenny et al., 2011) (see Chapter 12).
Balance assessment
The last two decades have seen a proliferation of tools for assessing balance. Some of these tools evaluate only one underlying impairment, and some are multidimensional. The tools range from highly technical and expensive to simple and portable. Table 59.1 provides an overview of various tools and the components of balance that they assess. Box 59.2 illustrates ‘red flags’ or signs and symptoms that indicate that the patient would benefit from further medical workup.
Table 59.1
Evaluation tools for assessing balance
| Self-perception scales | Falls Efficacy Scale (Tinetti et al., 1990, 1994b) |
| Modified Falls Efficacy Scale (Hill et al., 1996) | |
| Activities-specific Balance Confidence Scale (Powell & Myers, 1995) | |
| Assessment of sensory components | Sensory Organization Test of Computerized Dynamic Posturography (Monsell et al., 1997) |
| Clinical Test of Sensory Interaction and Balance (Shumway-Cook & Horak, 1986) | |
| Assessment of motor components | Functional Reach Test (Duncan et al., 1990) |
| Multidirectional Reach Test (Newton, 2001) | |
| Four Square Step Test (Dite & Temple, 2002) | |
| Limits of Stability (El-Kashlan et al., 1998) | |
| Motor Control Test (El-Kashlan et al., 1998) | |
| Five Times Sit to Stand (Csuka & McCarty, 1985) | |
| Multidimensional assessment | Performance Oriented Mobility Assessment (Tinetti, 1986) |
| Physical Performance Scale | |
| Berg Balance Scale (Berg et al., 1992) | |
| Balance Evaluation Systems Test (BESTest) (Horak et al., 2009) | |
| Gait assessment | Timed ‘Up & Go’ (Podsiadlo & Richardson, 1991) |
| Dynamic Gait Index (Shumway-Cook & Woollacott, 1995) | |
| Functional Gait Assessment (Wrisley et al., 2004) | |
| Gait speed |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







