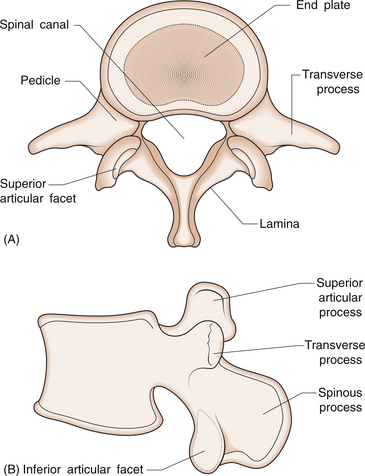
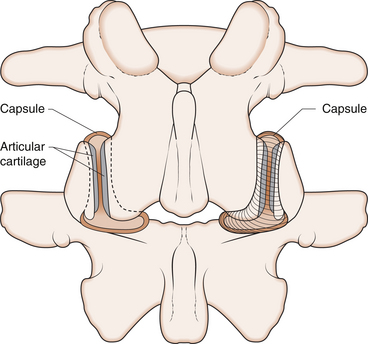
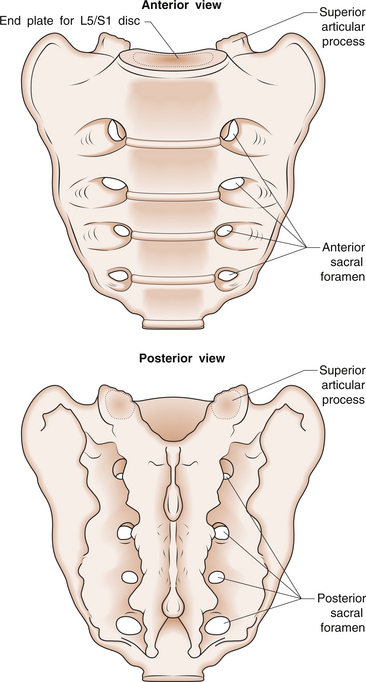
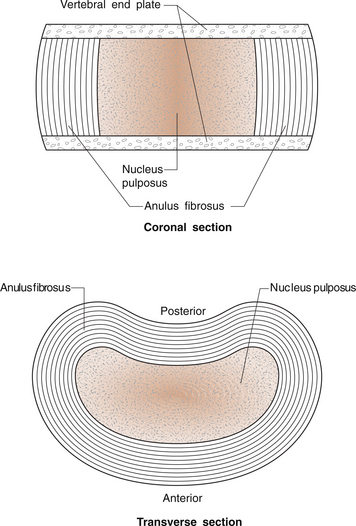
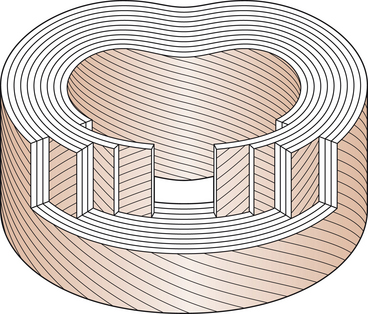
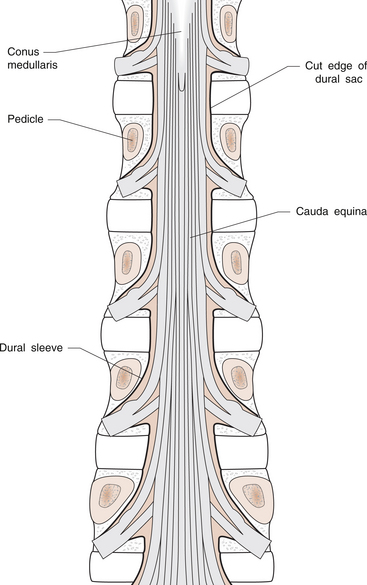
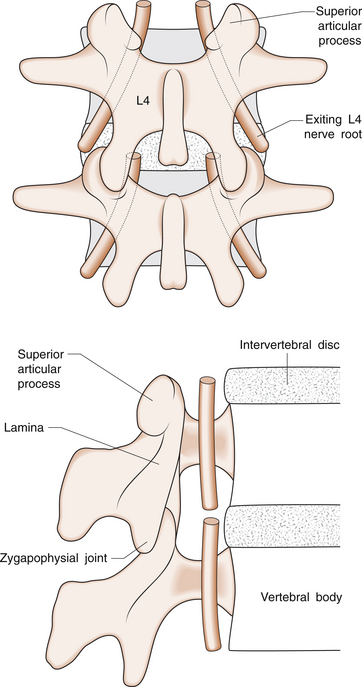
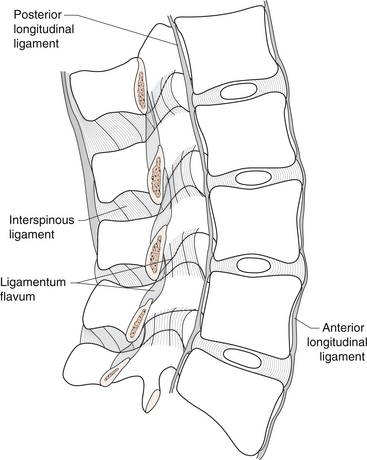
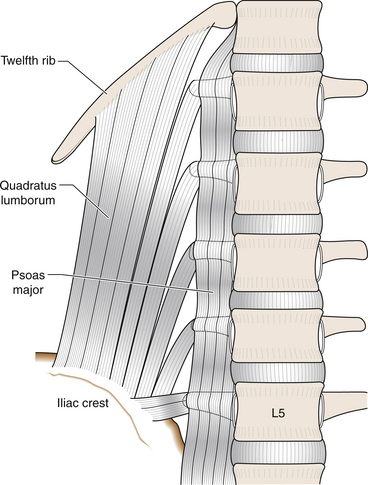
4 Les Barnsley There are five lumbar vertebrae, numbered from the top down. Traditionally, each vertebra is divided into its anterior and posterior elements, which are joined by thick pillars of bone called pedicles. The anterior element, or body, of the vertebra is a kidney-shaped prism of bone, with the concavity directed posteriorly and flat superior and inferior surfaces called endplates (Fig. 4.1). A small rim of bone makes up the outer margin of these surfaces. This is where the outer part of the intervertebral disc attaches, and is a secondary ossification centre of the vertebra. The pedicles are thick projections that originate nearer the superior part of the vertebral body at the postero-lateral corners. The posterior elements are those structures that lie behind the pedicles. Viewed from above, posterior elements, pedicles and posterior parts of the vertebral body elements are seen to form a protective ring that encloses the vertebral foramen. The part of this ring not containing the vertebral body is called the neural arch. The vertebral foramen is occupied by the spinal cord above L1/2 level and the spinal nerve roots below this. Two sheets of bone, or laminae, arise from the pedicles and join in the midline to complete the ring. A bony plate oriented in the sagittal plane develops from the fusion of the laminae and is known as the spinous process. Arising superiorly from the junction of each pedicle and its lamina, are two projections known as the superior articular processes. These present a relatively smooth curved surface posteriorly. From the lower corner of each lamina, there are matching projections known as the inferior articular processes, whose smooth curved surface is presented anteriorly. Together, these processes make up the posterior intervertebral joint between adjacent vertebrae. These joints are correctly termed zygapophysial joints, but are commonly and erroneously named facet joints. These joints are identified by side and level, indicating the vertebrae that they link, e.g. the right L4/5 zygapophysial joint (Fig. 4.2). Arising from the side of the lateral aspects of the pedicles are laterally oriented projections of bone known as the transverse processes (Fig. 4.1). The sacrum is a triangular bone at the base of the spine. It provides a base for the lumbar spine above, and yet is part of the pelvic ring. Its superior components are a flat kidney-shaped surface to match the L5 vertebral body and a superior articular process on each side to form the L5/S1 zygapophysial joints. The vertebral foramen continues into the sacrum, allowing passage of the sacral nerve roots through the bone before they exit through perforations on the anterior and posterior surfaces of the sacrum, known as the sacral foramina (Fig. 4.3). Between each pair of lumbar vertebrae, and between L5 and S1 lie the lumbar intervertebral discs. These have two components, an outer ring or annulus fibrosus and a central core, the nucleus pulposus (Fig. 4.4). The latter comprises a turgid gel made up of water (70–90%), proteoglycans and some collagen fibres. The proteoglycans are large molecules made up of glycosaminoglycans (GAGs) linked to proteins. The glycosaminoglycans are complex polysaccharides consisting of long chains of repeating units usually made up of a sugar molecule, then a sugar molecule with an amino group attached and so on. These are then linked to proteins. The importance of GAGs both in the disc and elsewhere (such as in articular cartilage) is that they are very hydrophilic, effectively sucking in and holding water. The collagen fibres in the nucleus pulposus are ‘protein ropes’ that provide some viscosity and tensile strength to the nucleus. There is no blood supply to the nucleus pulposus in the adult, and the nucleus is not innervated and so cannot hurt. The annulus fibrosus comprises alternating layers of obliquely oriented collagen fibres (Fig. 4.5). Collagens are a group of rope-like proteins. Macroscopic collagen fibres are made of many microfibrils that in turn comprise three polypeptide chains wound helically around each other. Collagen has significant tensile strength (the ability to withstand being pulled apart), which is exploited in numerous musculoskeletal structures, including bone, cartilage, tendons and ligaments. The outer one-third of the annulus fibrosus has nerve fibres and endings, so that this part of the disc may be a source of pain production. These joints are formed by the superior articular process of the lower vertebra and the inferior articular process of the upper vertebra. They are synovial joints (see Ch. 1), having a cartilage covering over the bony surface and a capsule lined by synovium (Fig. 4.2). In addition, they have intra-articular structures known as menisci, which help to cover the exposed articular cartilage when the joint moves. It is thought that entrapment of these menisci in the loose ends of the joint capsule may be a cause of an acute ‘locked back’. Irritation of the lumbar nerve roots can cause local somatic pain, but more characteristically causes neuropathic pain and neurological symptoms and signs in the legs. Knowledge of the relationship of the neural structures of the spine to the vertebral bodies and intervertebral discs is important in understanding nerve root compression due to herniated intervertebral discs, as well as other causes of nerve compression within the spinal column. The spinal cord itself terminates at the level of L1 or L2. The end of the cord is known as the conus medullaris, and the exiting nerve roots form the cauda equina ‘horse’s tail’, which descends within the dural sac (Fig. 4.6). The nerve roots lie at the back of the sac in the vertebral foramen, before running forward to exit the spinal canal under the pedicle of the vertebra after which they are named, i.e. the L4 nerve root enters underneath the L4 pedicle. They pass through the intervertebral foramen, bounded anteriorly by the vertebral body and the intervertebral disc, and posteriorly by the zygapophysial joint and lamina of the upper vertebral body (Fig. 4.7). A posterolateral prolapsed disc can compress the exiting nerve root against the bony structures behind it. Such a prolapse at L4/5 would compress the L4 nerve root. A more central disc prolapse may compress the next nerve root travelling to exit below. This would particularly be the case where there is some narrowing of the vertebral foramen, such as may occur with hypertrophied lumbar zygapophysial joints. The role of the ligaments of the lumbar spine in the production of back pain remains controversial. It has been suggested, by analogy with ligamentous injuries elsewhere, that sprains of these ligaments might cause pain. Knowledge of their basic anatomy is useful, particularly in interpreting imaging. Other than the intervertebral discs, whose annulus fibrosus may be considered a ligament, there are four main ligaments that link adjacent vertebrae (Fig. 4.8). The anterior longitudinal ligament is a thin, flat ligament that covers the front of the spine on the anterior surface of the vertebral bodies and intervertebral discs. The fibres of the anterior longitudinal ligament are oriented vertically, resisting separation of the anterior parts of adjacent vertebral bodies. The posterior longitudinal ligament runs along the posterior surface of the vertebral body, inside the vertebral foramen. Its fibres are also vertically oriented, and it resists separation of the posterior margins of adjacent vertebral bodies. The ligamentum flavum is a series of small ligaments joining the laminae of adjacent vertebrae. They have a very high elastin content, which means that the ligament is more like a rubber band than a rope. Its role seems to be to preserve the shape and smoothness of the vertebral foramen during spinal movements, and prevent compression of the neural structures. In some patients, particularly with zygapophysial joint arthrosis, the ligamentum flavum can become thickened and contribute to a narrowing of the vertebral foramen. The interspinous ligament spans adjacent spinous pro-cesses, and restricts separation of the spinous processes, as might occur in forward flexion of the spine. Several muscles act to move the lumbar spine. Flexion and rotation is achieved through contraction of the abdominal muscles. The psoas major muscle arises from the transverse processes of the lumbar vertebrae and the lateral margins of the vertebral bodies. It attaches into the lesser trochanter of the hip, and can either flex the hip or, if the hip is fixed, flex the lumbar spine. Quadratus lumborum is a broad, flat muscle that attaches to the iliac crest, the inferior margins of the 12th rib and the transverse processes of the lumbar spine. This muscle appears to both fix the 12th rib during respiration and facilitate lateral flexion of the lumbar spine (Fig. 4.9). There are several small muscles linking the transverse processes of adjacent vertebral bodies (the intertransversarii). Their function may be to produce proprioceptive information about the position of the lumbar spine, rather than to exert any significant force.
BACK PAIN
Normal lumbar spine anatomy
Vertebrae and sacrum
Intervertebral discs
Lumbar zygapophysial joints
The lumbar nerve roots and spinal cord
Ligaments
Muscles
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


BACK PAIN
Only gold members can continue reading. Log In or Register to continue