8 Associated techniques
Chill-and-stretch (spray-and-stretch) technique
Integrated neuromuscular inhibition technique (INIT)
Ischaemic compression and trigger point release
Muscle energy techniques (MET) – including isolytic stretch
Neuromuscular therapy (soft tissue manipulation)
Percussion technique or spondylotherapy
Proprioceptive adjustment (applied kinesiology)
Pump techniques – lymphatics, liver/spleen, pedal
‘S’ and ‘C’ bends: myofascial release methods for lengthening soft tissues
Stretching fascia – myofascial release
Specific (abdominal) release techniques
Strain–conterstrain and positional release techniques
Soft tissue approaches
In Chapter 6 a detailed description was given of NMT in spinal, cervical, pelvic and intercostal structures, and abdominal techniques were described in Chapter 7.
In this chapter a number of additional soft tissue approaches/modalities/methods that are frequently employed alongside NMT (listed in Box 8.1) will be outlined in alphabetical order, rather than any other sequence.
Box 8.1 Additional soft tissue approaches
• Active release technique (ART)
• Integrated neuromuscular inhibition technique (INIT)
• Ischaemic compression/trigger point release
• Neuromuscular therapy/soft tissue manipulation discussion
• Pump techniques (liver, lymphatics, spleen, pedal)
• Stretching fascia – myofascial release
• Specific (abdominal) release techniques
Active release technique® (ART)
There have been relatively few studies to evaluate efficacy, however one pilot study demonstrated no benefit to quadriceps function in athletes with anterior knee pain where ART was applied (Drover et al 2004). While in different pilot studies:
Elbow (and forearm) technique
Caution – Direct elbow pressure should be avoided, or should be performed with great care:
1. if tissues are inflamed or during the remodelling phase, following trauma, is incomplete
3. close to blood vessels and nerves
Sacrospinalis
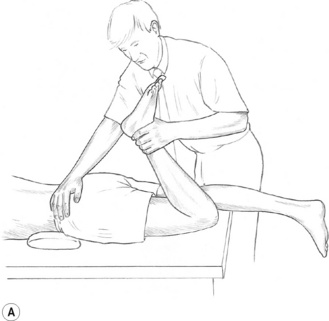
In treating sacrospinalis, for example, the entire spine should be lubricated, and the practitioner should stand on the patient’s left side (patient supine, pillow under thorax) (Fig. 8.1).
• The right elbow tip should be placed just superior to the sacral base, with the forearm at right angles to the patient’s body, as in Fig. 8.1A (and also Figs 10.13B,C)
• By flexing the knees slightly and allowing weight to be transferred via the elbow, the practitioner can apply controlled pressure to the paraspinal muscles with the broad contact of the forearm, or by raising the hand slightly, more precisely by the elbow itself.
• The more the hand is elevated, the sharper the angle of contact of the elbow, and the more precise strokes will be, at the point of contact.
• The elbow/forearm should be allowed to glide slowly cephalad.
• If pain is reported, pressure should be reduced.
• Several glides or strokes along the full length of the spine will greatly relax even marked contractions.
Chronic shoulder restriction
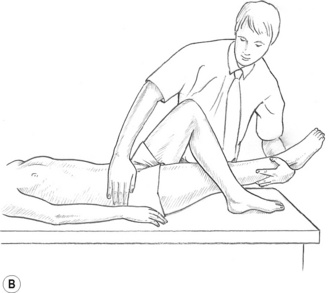
An example of more focused use of elbow technique involves work on the lateral border of the scapula in cases of chronic shoulder restriction (see Fig. 8.1B).
• The patient is side-lying with the side to be treated uppermost, and with the arm abducted, elevated, extended and externally rotated, so that the patient’s hand is close to her head.
• The practitioner should be behind the patient, standing sideways on to the table, facing her head.
• With his non-tableside hand the practitioner grasps the patient’s upper arm, close to the elbow, reinforcing the external rotation, abduction, etc.
• The practitioner’s tableside arm is flexed at the elbow, which should be carefully placed in the patient’s exposed axilla, as close to the lateral border of the scapula as possible.
• Short, slow-moving strokes should be applied along the scapula border, as well as anteriorly and posteriorly, following the curve of the ribs below the axilla.
• If localized contracted tissue is sensed it may be helpful to simply apply sustained, tolerably comfortable, pressure – and wait for a softening to occur.
• The non-treating hand should use any release resulting from the elbow treatment to gradually increase the range of rotation and abduction at the shoulder, to improve humeroglenoid movement.
Treatment of piriformis muscle, and its central trigger points, can usefully be achieved by means of direct elbow pressure, applied to the main trigger point area in the belly of the muscle, while the side-lying patient’s leg is rotated to internally rotate the hip, in order to achieve a lengthening of the muscle. (See illustrated details of the use of the elbow in this way, later in this chapter under the heading Piriformis Technique (see Fig. 8.11)).


 Chill-and-stretch (spray-and-stretch) technique
Chill-and-stretch (spray-and-stretch) technique
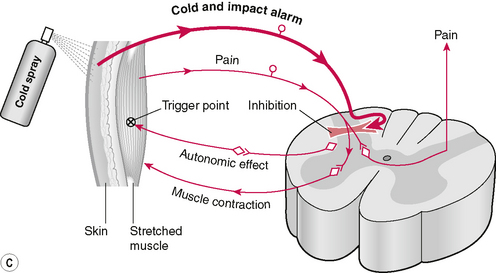
Chilling and stretching a muscle housing a trigger point rapidly assists in deactivation of the abnormal neurological behavior of the site. Travell & Mennell have described these effects in detail (Mennell 1969, 1975, Simons et al 1999, Travell 1952, Travell & Simons 1992).
Travell & Simons (1992) and Simons et al (1999) have discouraged the use of vapocoolants to chill the area, because of environmental considerations relating to ozone depletion, and have instead urged the use of stroking with ice in a similar manner to the spray stream to achieve the same effect. The objective is to chill the surface tissues while the underlying muscle housing the trigger is simultaneously stretched. They also point out that the spray is applied before or during the stretch and not after the muscle has already been elongated.
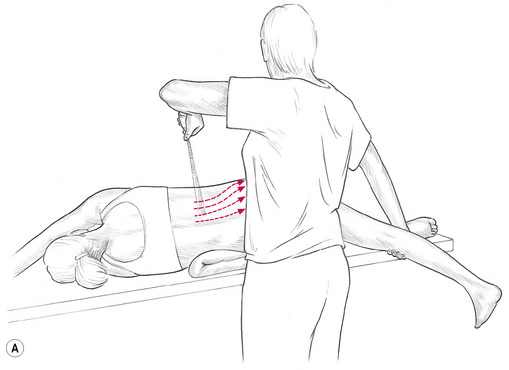
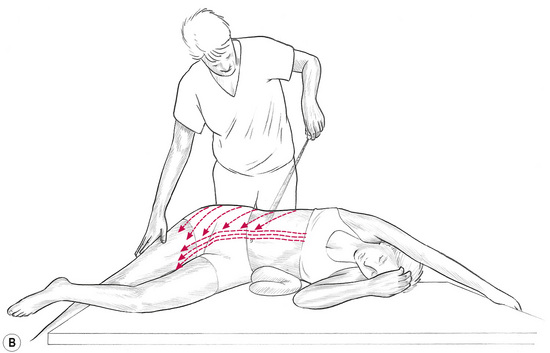
A container of vapocoolant spray with a calibrated nozzle which delivers a moderately fine jet stream, or a source of ice, is needed. The jet stream should have sufficient force to carry in the air for at least 3 feet. Experience suggests that a mist-like spray is less effective. (See Figs 8.2A,B.)
Simons & Mense (2003) report that the vapocoolant spray appears to inhibit pain and reflex motor, and autonomic responses in the central nervous system. When the pain stimuli subside a degree of relaxation takes place allowing stretching and lengthening of the muscle to be more effective and less uncomfortable (Lupandin & Kuz’mina 1985). (See Fig. 8.2C).
Ice as an alternative
The author has found that a cold soft-drink-can, that has been partially filled with water and then frozen, is more suitable, because ice applied directly onto skin melts rapidly and, as Travell & Simons (1992) have pointed out, the skin must remain dry for this method to be successful, because dampness slows the rate of cooling of the skin and may also delay rewarming.
Method
• If a spray is used, the container should be held approximately 2 feet (60 cm) away, in such a manner that the jet stream meets the body surface at an acute angle or at a tangent, not perpendicularly (Figs 8.2A,B).
• This lessens the shock of the impact. For the same reason, the stream is sometimes started in air, or on the practitioner’s hand, and is gradually brought into contact with the skin overlying the trigger point.
• The stream/ice massage/frozen canister should be applied in one direction only, not back and forth.
• Each sweep should commence in the tissues overlying the trigger point and be moved slowly and evenly outward over towards reference zone (where pain is reported as being experienced by the patient). The direction of movement of the spray/ice should follow the fibre direction of the muscle.
• It appears that it is advantageous to spray, or ice-chill, both trigger and reference areas, because secondary trigger points are likely to have developed within reference zones when pain is very strong.
• Clinical experience suggests that the optimum speed of movement of the sweep/roll over the skin, is approximately about 4 inches (10 cm) per second.
• Each sweep should be started slightly proximal to the trigger point, and be moved slowly and evenly through the reference zone, to cover it and extend slightly beyond it.
• These sweeps should be repeated in a rhythm of a few seconds on, and a few seconds off, until all the skin over trigger and reference areas has been covered once or twice.
• If aching or ‘cold pain’ develops, or if the application of the spray/ice/canister sets off a reference of new pain, the interval between applications should be lengthened.
• Care should be taken not to frost or blanch the skin.
• During the application of cold the taut fibres should be placed at light stretch, and after the chilling should be further stretched passively.
• Steady, gentle stretching is usually essential if a satisfactory result is to be achieved.
• As relaxation of the muscle occurs, continued stretch should be maintained for 20–30 seconds, and after each series of cold applications active motion should be tested.
• The patient should be asked to move in the directions that were restricted before spraying/chilling, or that were painful to activate.
• An attempt should be made to restore the full range of motion, but always within the limits of discomfort, as sudden overstretching can increase existing muscle spasm.
• The treatment is continued in this manner until the trigger points (often several are present) and their respective pain reference zones have been treated.
• The entire procedure may occupy 15–20 minutes and should not be rushed.
Deep tissue release
The method recommended is as follows:
• The contact on the tissues involved is made by extending the digits of either hand and making firm contact with the area between the first and second metacarpophalangeal joints, taking out the slack of the tissues and engaging a resistance barrier.
• This contact is rotated clockwise or anticlockwise in order to increase the tension in the underlying tissues, until the tissues with the greatest resistance are noted and combined barrier is engaged – downwards and in a torsional manner.
• The other hand is then placed over the contact hand so that the downward pressure and rotation are reinforced.
• In addition, a further direction of stretch should be introduced by the second hand –directed laterally/medially or superiorly/inferiorly, whichever offers the greatest resistance.
• The tissues would therefore be receiving a direct downward pressure, a rotational stretch, and a further degree of stretch in another direction, all maintained by the two treating hands.
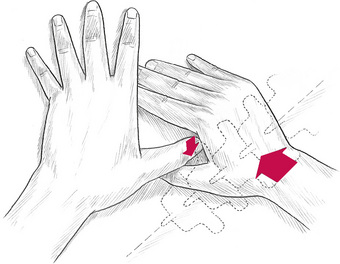
• The overlying hand should have been placed in such a way that the radial border of the metacarpal base of the thumb is directly over the contact point of the first hand’s contact (i.e. over the second metacarpal joint area). (See Fig. 8.3.)
• The fingers of the overlying hand should be tightly in contact with the lateral border of the contact hand.
The last stage of the release technique may be performed in one of two ways:
1. The overlying hand executes a short sharp squeeze by flexing the middle finger against the metacarpals of the contact hand. The resulting pressure in the intermetacarpal area provides the ‘thrust’ or release force. The line of force of this squeeze is towards the practitioner.
2. The second method of release, which is more suitable for deeper contractions of tissue, is applied via short sharp thrust by the overlying hand against the contact hand, with a simultaneous medial rotation of the contact hand. The line of force in this technique is away from the practitioner.
Induration technique
![]() As many patients are too frail, or too ill, to allow the full NMT treatment to be applied, a useful technique exists to aid in normalizing reflex and local areas of the paraspinal musculature. Stoddard (1969) has pointed out that protective spasm in muscle can often indicate underlying pathology (osteoporosis, etc.) and, clearly, deep pressure techniques would be contraindicated in such conditions.
As many patients are too frail, or too ill, to allow the full NMT treatment to be applied, a useful technique exists to aid in normalizing reflex and local areas of the paraspinal musculature. Stoddard (1969) has pointed out that protective spasm in muscle can often indicate underlying pathology (osteoporosis, etc.) and, clearly, deep pressure techniques would be contraindicated in such conditions.
• With the patient sitting or lying, the practitioner, using a very light ‘skin-on-skin’ contact which evaluates ‘drag’ or hills/valleys (see Ch. 5), runs the fingertips longitudinally down the side of the spine (side of spine opposite that on which practitioner is standing) over the transverse processes.
• Any spot or area of ‘hardened’ or indurated tissue, that also palpates as tender to the patient is marked for attention.
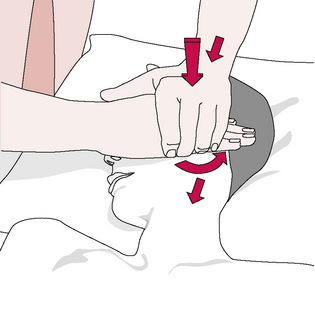
• Treatment is applied by palpating the sensitive area with the tip of the thumb (or a finger), of one hand, while applying light pressure towards the painful spot with the soft thenar or hyperthenar eminence of the other hand, which is resting on the spinous process of the vertebra, adjacent to the indurated tissue (Fig. 8.4).
• Direct pressure (extremely light – ounces/grams only) towards the pain should lessen the degree of tissue contraction, and the sensitivity.
• If it does not do so, the angle of light pressure on the spinous process, towards the painful point, should be varied slightly, so that, somewhere within an arc embracing a half circle, an angle of push towards the pain will be found to abolish the pain totally, and will lessen the palpated feeling of tension.
• This ‘position of ease’ is held for around 20 seconds, before moving on to the next sensitive area.
Integrated neuromuscular inhibition technique (INIT)
![]() INIT, when used to deactivate a trigger point, involves the application of a sequence that includes:
INIT, when used to deactivate a trigger point, involves the application of a sequence that includes:
• Inhibitory (ischaemic) compression (either sustained or intermittent: 5 seconds pressure/2 seconds release/repeated) until a change is reported or noted.
• Place the tissues into a position of ease, to encourage a muscle spindle release of excessive tone (see descriptions of ‘positional release’ below).
• The patient introduces an isometric contraction involving the precise tissues housing the trigger point.
• This is followed by passive stretching of the local tissues.
• Followed by active and passive stretching of the entire muscle (subsequent to another isometric contraction) (see notes on muscle energy technique (MET) below).
• After this activation of antagonists to muscle housing the trigger point may be used to complete the sequence.
Ischaemic compression and trigger point release
Hou et al (2002) report: ‘Ischemic compression therapy provides alternative treatments using either low pressure (pain threshold) and a long duration (90 s) or high pressure (the average of pain threshold and pain tolerance) and short duration (30 s), for immediate pain relief and myofascial trigger point sensitivity suppression.’
Caution – Direct pressure should be avoided, or performed with great care:
1. If tissues are inflamed, or are in the remodelling phase, following trauma
3. Close to blood vessels and nerves
4. Close to attachment sites (to avoid provoking enthesitis)
Travell & Simons (1983, 1992) have suggested that in treatment of trigger points, these should receive ischaemic compression (‘sustained digital pressure’) for a period of between 20 seconds and 1 minute. The pressure should be gradually increased as the trigger point’s sensitivity (referred sensation, as well as the local discomfort) reduces, and the tension of the tissues housing the trigger (‘taut band’) eases. Stretching techniques should be applied following the compression; see integrated neuromuscular inhibition technique (INIT) described later in this chapter.
Fernández-De-Las-Peñas et al (2006) report on a study that verified these suggestions. ‘Ischemic compression technique and transverse friction massage were equally effective in reducing tenderness in myofascial trigger points.’
The mechanisms involved, as seen from a Western perspective, would include ‘neurological overload’, the release of endogenous morphine-like products (endorphins, enkephalins, endocannabinoids) (McPartland & Simons 2007) as well as ‘flushing’ of tissues with fresh oxygenated blood following the compression. Oriental interpretations would include modulation of energy transmission.
See Chapter 3, Box 3.5, for more detail on compression effects.
Massage
Using standard massage protocols, Field (2000) and others have demonstrated, in hundreds of research projects, that significant benefits occur in the following conditions and patient populations: enhanced growth in preterm infants, cocaine and human immunodeficiency virus (HIV)-exposed infants, pain reduction, during labour, pre-debridement for burn patients, juvenile rheumatoid arthritis, fibromyalgia, premenstrual syndrome, migraine, children with autism, adolescents with attention deficit hyperactivity disorder (enhanced attentiveness), anxiety (e.g. exam settings), depression, post-traumatic stress, adolescent psychiatric patients, adolescent mothers, bulaemia and anorexia, chronic fatigue syndrome, autoimmune and immune disorders, diabetes mellitus (reduced glucose levels), asthma, cystic fibrosis, atopic dermatitis, HIV-positive adults, oncology patients.
Some of Field’s explanations for the benefits of massage are summarized later in this section.
Massage methodology
The strokes that make up massage strokes include:
• Petrissage – wringing and stretching movements, across the fibre direction of muscles.
• Kneading – where the hands shape themselves to the contours of the area being treated. The tissues between the hands are lifted and pressed downwards and together.
• Inhibition – which involves application of pressure directly to the belly or origins or insertions of contracted muscles or to local soft tissue dysfunction for a variable amount of time or in a ‘make-and-break’ (pressure applied and then released) manner to reduce hypertonic contraction or for reflexive effects.
• Effleurage – this is a relaxing technique that is used, as appropriate, to initiate or terminate other manipulative methods. Pressure is usually even throughout the strokes, which are applied with the whole hand in contact.
• Vibration and friction – such contacts are used near origins and insertions and near bony attachments for relaxing effects on the muscle as a whole and to reach layers deep to the superficial tissues. It is performed by small circular or vibratory movements, with the tips of fingers or thumb. The heel of the hand may also be used.
• Roulement – this involves skin lifting and rolling, which, as with most massage methods, can be used diagnostically as well as therapeutically (see earlier in this chapter for discussion of skin rolling).
• Transverse or cross-fibre friction – this is performed along or across the belly of muscles using the heel of the hand, thumb or fingers applied slowly and rhythmically or vigorously, depending upon the objectives.
• Tapotement – involves percussive tapping, clapping, drumming and vibrating activities, involving fingertips or the ulnar borders of the hands.
Massage cautions (Wittlinger & Wittlinger 1982)
• In areas that have been recently traumatized (2–3 weeks) and which are in the remodelling phase (including surgery).
• When a person is fatigued the duration and depth of the application should be reduced.
• If a patient has a fragile bone structure, the depth of pressure should be modified.
• When the patient is agitated the rhythm should be modified to create a calming effect.
• Acute infections and acute inflammation (generalized and local)
Physiological effects of massage
The biochemical influences of massage include altered stress hormone (cortisol) production (Field 2000). Perhaps surprisingly, massage fails to increase blood flow through muscle unless it is exceptionally vigorous (Shoemaker et al 1997); however, drainage efficiency is improved when light techniques are employed (Ikimi et al 1996).
• Pain perception is reduced by massage, possibly due to gating of impulses (Clelland et al 1987).
• Massage mechanically modifies soft tissue status (stretching, mobilizing, etc.) depending on the variations in load application (sustained pressure, shearing load, etc.).
• The colloids in fasciae that surround, support and invest all soft tissues respond to appropriately applied pressure and vibration by changing state from a gel-type consistency to a solute, which increases internal hydration and assists in the removal of toxins from the tissue (Oschman 1997).
• Psychological effects include reduced arousal, calmer mood and modified perception of anxiety (Rich 2002).
• Neurological influences include a transient reduction in motor neuron excitability during and following massage (Goldberg 1992).
• Massage also produces a decrease in the sensitivity of the gamma efferent control of the muscle spindles and thereby reduces any shortening tendency of the muscles (Puustjarvi 1990).
Massage effects explained
How are the various effects of massage and soft tissue manipulation explained? Field (2000), discussing her many research findings, states:
Field further suggests that the evidence from her studies points to enhanced homeostatic function, in both infants and adults, following massage therapy, as evidenced by improved sleep patterns (and therefore higher levels of somatostatin), as well as increased serotonin levels. These thoughts are supported by the work of other researchers (Ironson et al 1993).
Apart from the undoubted anxiety and stress-reducing influences of massage, a combination of physical effects also occurs (Sandler 1983):
1. Pressure, as applied in deep kneading or stroking along the length of a muscle, tends to displace its fluid content.
2. Venous, lymphatic and tissue drainage is thereby encouraged.
3. The replacement of this with fresh oxygenated blood aids in normalization via increased capillary filtration and venous capillary pressure.
4. This reduces oedema and the effects of pain-inducing substances that may be present (Hovind & Nielson 1974, Xujian 1990).
5. Massage also produces a decrease in the sensitivity of the g-efferent control of the muscle spindles, and thereby reduces any shortening tendency of the muscles (Puustjarvi et al 1990).
6. Pressure techniques, such as are used in NMT, and the methods employed in MET have a direct effect on the Golgi tendon organs, which detect the load applied to the tendon or muscle.
7. These have an inhibitory capability, which can cause the entire muscle to relax.
8. The Golgi tendon organs are set in series in the muscle, and are affected by both active and passive contraction of the tissues. The effect of any system that applies longitudinal pressure or stretch to the muscle will be to evoke this reflex relaxation. The degree of stretch has, however, to be great, as there is little response from a small degree of stretch.
9. The effects of MET, articulation techniques and various functional balance techniques depend to a large extent on these tendon reflexes (Sandler 1983).
Soft tissues at centre stage
We are in the midst of a change in the concepts of manual therapy that has far-reaching implications. One of the major changes is the restoration of the soft tissue component to centre stage, rather than the peripheral role to which it has been assigned in the past as ever more general health problems are found to involve musculoskeletal dysfunction, for example chronic fatigue conditions (Chaitow 1990).
Lewit (1985) discusses aspects of what he describes as the ‘no man’s land’ that lies between neurology, orthopaedics and rheumatology, which, he says, is the home of the vast majority of patients with pain derived from the locomotor system, and in whom no definite pathomorphological changes are found. He makes the suggestion that these be termed cases of ‘functional pathology of the locomotor system’. These include most of the patients attending osteopathic, chiropractic and physiotherapy practitioners.
Muscle energy techniques (MET) – including isolytic stretch
Muscle energy technique (MET) involves the use of isometric contractions (Mitchell et al 1998) to assist in modification of muscle and joint behavior. Variations on this basic theme involve the use of isotonic concentric, or eccentric, contractions (Schmitt 1999), or a series of rhythmically pulsating contractions (Ruddy 1961) instead of, or as well as, basic isometric variations.
Definition of MET
MET involves a muscle, or group of muscles, being voluntarily contracted, in a specified direction, for a defined length of time (commonly 5 to 7 seconds), involving submaximal effort, with the contraction being matched by the practitioner/therapist’s effort, so that no movement occurs (Mitchell & Mitchell 1995, Mitchell 1976).
• MET has been shown to improve joint range of motion, including spinal joints (Kamani & Walters 2000, Lenehan et al 2003).
• MET has been shown to improve muscle extensibility more effectively than passive, static stretching – both in the short and long term (Mehta & Hatton 2002, Feland et al 2004, Ferber et al 2002).
• In addition studies offer support for the hypoalgesic effects of MET – for example in relation to spinal pain (Brodin 1962, Cassidy et al 1992, Wilson et al 2003).
• Myofascial trigger point deactivation has been shown to be enhanced by use of MET (Chaitow 1994, Fernández-de-las-Peñas 2005, Simons et al 1992, 1999).
MET origins
Much of the research from which conclusions regarding MET efficacy and mechanisms are taken, relates to studies involving proprioceptive neuromuscular facilitation (PNF) stretching. (Fryer 2006, Schmitt et al 1999) PNF (and MET) application may involve one of 3 variations:
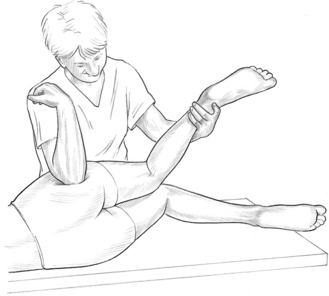
• Contract–relax (CR), in which the muscle being stretched (the agonist) is contracted and then relaxed, before stretching. (See Fig. 8.5A and 8.5B).
• Agonist contract–relax (ACR), in which contraction is of the antagonist, rather than the muscle to be stretched (the agonist). It is suggested that the confusing title of Agonist contract-relax (ACR) should be ignored. The approach relies, it is suggested (see below), on reciprocal inhibition.
• Contract–relax agonist–contract (CRAC), involves a combination of the two methods (CR and ACR) listed above.
Proposed MET mechanisms
Kuchera & Kuchera (1992) as well as Denslow et al (1993) have speculated on the neurological mechanisms that may follow use of MET (contract/relax version).
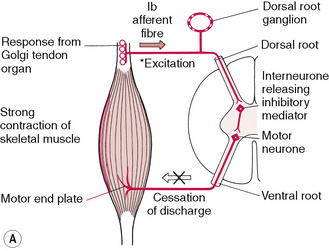
• They hypothesize that the effects may result from the inhibitory Golgi tendon reflex, activated during the isometric contraction that leads to reflex relaxation of the muscle, as a result of post isometric relaxation (PIR) (see Fig. 8.6A).
• An alternative reflex effect has been suggested in which an isometric contraction of the antagonist(s) of affected muscle(s) induce relaxation via reciprocal inhibition (RI) (ACR version) (see Fig. 8.6B).
Some studies support the concept of neurological muscle inhibition, following MET isometric contraction. For example Moore & Kukulka (1991) found that a strong brief depression of the soleus H-reflex occurred, for about 10 seconds, following sub-maximal isometric plantar flexion contractions, probably as a result of pre-synaptic inhibition.
However simultaneous monitoring of the tibialis anterior muscle’s EMG activity revealed minimal activity, so excluding the possibility of reciprocal inhibition operating (Moore & Kukulka 1991).
Since many studies have demonstrated that active motor activity plays a minimal role in producing resistance to stretch (Magnusson et al 1996b) the question remains as to whether low-level motor activity plays a role in limiting the passive stretch of a muscle.
Self-evidently, in order for it to be accepted that MET produces increased muscle length, by means of reflex muscle relaxation, low-level motor activity needs to be shown to play a role in limiting passive stretching of muscle, and this has not been possible (Fryer 2006).
• Ballentyne et al (2003) suggest that the PIR theory is poorly supported by research. Citing EMG evidence they note that ‘various studies have shown that passive stretch does not influence the electrical activity of the hamstring muscle (Klinge et al 1997, McHugh et al 1998) demonstrating that low level muscle contraction does not limit muscle flexibility, disputing the proposal of [such] a neurological mechanism.[i.e. PIR]’
• Lederman (1995) states that the PIR model ignores the complex and dominant influence of the central nervous system.
• Fryer (2000) points to the lack of evidence supporting muscle contraction as a factor in restricted joint ROM, or in spinal dysfunction.
• Magnusson et al (1995) found that low-level EMG activity was unchanged following isometric contractions, or passive stretching.
• Magnusson et al (1996a) have demonstrated that increases in muscle length, following 90 seconds of passive stretching, occurs without any change to the low-level EMG activity of that muscle.
• Fryer (2006) has speculated that although the exact mechanism by which increased muscle extensibility occurs, remains unclear, it probably involves both neurophysiological and mechanical factors, possibly including viscoelastic and plastic changes in the connective tissue elements of the muscle. In fact Fryer maintains that although MET techniques produce greater ROM changes than static stretching, they also produce greater EMG activity in the muscle undergoing the stretch.
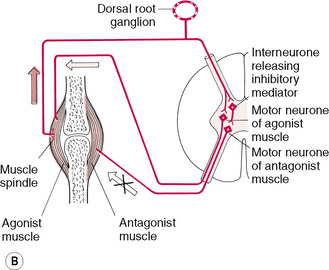
• Fryer & Fossum (2008) have hypothesized a neurological explanation for the analgesic effects of MET. A sequence is suggested in which activation of muscle mechanoreceptors and joint mechanoreceptors occur, during an isometric contraction. This leads to sympatho-excitation evoked by somatic efferents and localized activation of the periaqueductal grey that plays a role in descending modulation of pain. Nociceptive inhibition then occurs at the dorsal horn of the spinal cord, as simultaneous gating takes place of nociceptive impulses in the dorsal horn, due to mechano-receptor stimulation (see Fig. 8.6C).
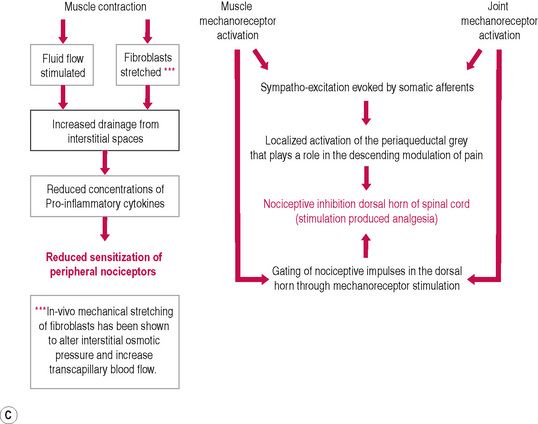
Figure 8.6C Schematic diagram of hypoalgesic effects of MET.
Modified from Fryer G., Fossum C. 2009. Therapeutic Mechanisms Underlying Muscle Energy Approaches. In: Physical Therapy for tension type and cervicogenic headache. Fernández de las Peñas C., Arendt-Nielsen L., Gerwin R. (Eds): Jones & Bartlett, Boston.
Alternative explanations
• At its simplest this explanation observes that if, after an isometric contraction, the same degree of effort is used, as was employed to take the muscle or joint to its end of range, before the contraction, no increase in range or extensibility occurs.
• Magnusson et al (1998, 1996b) measured the degree of applied effort used during passive knee extension, before and after the hamstrings were stretched to the point of pain. They found that both ROM and passive torque were increased following the contraction – because subjects were able to tolerate a stronger stretch.
• Ballantyne et al (2003) confirmed these findings by showing that when the degree of post-test force applied to the muscle remained constant (i.e. the same as used in pre-testing), no change in length took place, suggesting that a single application of MET created a change in tolerance to stretch.
• Fryer (2006) explains: ‘The application of MET would appear to decrease an individual’s perception of muscle pain, and is greater than that which occurs with passive stretching. Stretching and isometric contraction stimulate muscle and joint mechanoreceptors and proprioceptors, and it is possible that this may attenuate the sensation of pain. … MET and stretching appear to produce lasting changes in stretch tolerance, and so the mechanism is likely to be more complex than just gating at the spinal cord, and may also involve changes in the higher centres of the CNS.’
• Hamilton et al (2007) suggest that techniques – such as MET – that stimulate joint proprioceptors, via the production of joint movement, or the stretching of a joint capsule, may be capable of reducing pain by inhibiting the smaller diameter nociceptive neuronal input at the spinal cord level.
What else might produce MET’s analgesic effects?
Brodin (1982), Cassidy et al (1992) and Wilson et al (2003) have all reported that there is a reduction in spinal pain, following application of MET. These reports therefore support the evidence described above, of an increased tolerance to stretch, of muscles treated by MET.
• Degenhardt et al (2007) report that concentrations of several circulatory pain biomarkers (including endocannabinoids and endorphins) were altered following osteopathic manipulative treatment incorporating muscle energy, and other soft tissue techniques. The degree and duration of these changes were greater in subjects with chronic LBP than in control subjects.
• McPartland (2008) and others (Pertwee 2005, Agarwal & Pacher 2007) note that the endocannabinoid (eCB) system, like the better-known endorphin system, consists of cell membrane receptors, endogenous ligands and ligand metabolizing enzymes. Two cannabinoid receptors are known:
Two of the eCB ligands, anandamide (AEA) and 2-AG, are mimicked by cannabis plant compounds. McPartland reports that: ‘AEA and 2-AG are not stored in vesicles like classic neurotransmitters. Rather they are synthesized “on demand” from precursor phospholipids in the neuron cell membrane and immediately released into the neural synapse. (Pertwee 2005). The eCB system dampens nociception and pain, and decreases inflammation in myofascial tissues.’
• Agarwal & Pacher (2007) suggest that cannabinoids mediate analgesia largely via peripheral type 1 cannabinoid receptors (CB1), in pain receptors.
Alternatives to standard isometric contraction versions of MET
• An isotonic eccentric stretch is one in which the practitioner overcomes the effort of the contracting muscle, stretching and simultaneously toning it (Liebenson 2006, Norris 1999, Kolar 1999).
• A rapid isotonic eccentric contraction, the origin and insertion of the muscles involved are taken further apart while the muscle is contracting, due to the greater effort of the practitioner’s counterforce overcoming the muscular effort. When such a manoeuvre is performed rapidly, it is known as an isolytic contraction. Isolytic stretches are useful in cases where a marked degree of fibrotic change is present in the soft tissues. The effect is to create microtrauma during the rapid stretch, subsequently allowing an improvement in elasticity and circulation. To achieve an isolytic contraction (eccentric isotonic), the patient should be instructed to use no more than 20% of possible strength on the first contraction, which is resisted and overcome by the practitioner, in a contraction lasting 2–3 seconds. This is then repeated, but with an increased degree of effort on the part of the patient (assuming the first effort was relatively painless). This continuing increase in the amount of force employed in the contracting musculature may be continued until, hopefully, a fairly strong but painless contraction effort is possible, again to be resisted and overcome by the practitioner. In some muscles, of course, this may require a heroic degree of effort on the part of the practitioner, and alternative methods would need to be found. NMT would seem to offer one such alternative. The isolytic manoeuvre should have as its ultimate aim a fully relaxed muscle, able to reach its normal resting length. This will seldom be possible in one treatment session.
![]() •A slow isotonic eccentric contraction offers various important clinical benefits (Lewit 1999, Liebenson 2001, Norris 1999): To tone postural (type I) muscles that may have lost their endurance potential, a slow isotonic eccentric contraction should be performed, involving increasing degrees of effort. For example, slowly overcome flexion of the wrist forcing it into extension (i.e. the arm flexors, which are postural type I muscles, are stretched while contracting). To relax hypertonic postural (type I) muscles, a slow isotonic eccentric stretch should be performed of their inhibited antagonists (using 40–80% strength). For example, slowly overcome the extended wrist, forcing it into flexion (i.e. the arm extensors, which are phasic type II muscles, are contracting but their effort is overcome).
•A slow isotonic eccentric contraction offers various important clinical benefits (Lewit 1999, Liebenson 2001, Norris 1999): To tone postural (type I) muscles that may have lost their endurance potential, a slow isotonic eccentric contraction should be performed, involving increasing degrees of effort. For example, slowly overcome flexion of the wrist forcing it into extension (i.e. the arm flexors, which are postural type I muscles, are stretched while contracting). To relax hypertonic postural (type I) muscles, a slow isotonic eccentric stretch should be performed of their inhibited antagonists (using 40–80% strength). For example, slowly overcome the extended wrist, forcing it into flexion (i.e. the arm extensors, which are phasic type II muscles, are contracting but their effort is overcome).
• A concentric isotonic contraction tones the muscle that is active.
• Ruddy (1961) suggested that the effects of what he termed rapid resisted duction (i.e. pulsed isometric contractions) include improved local oxygenation, enhanced venous and lymphatic circulation, as well as an improved static and kinetic posture, due to the effects on proprioceptive and interoceptive afferent pathways.
• These variations, along with their particular influences, appear to produce identical benefits in terms of increased ROM and extensibility of soft tissues irrespective of which form of MET methodology is employed. For example, in a study of the use of MET in treatment of piriformis dysfunction, it was found that the same results emerged whether the agonist or the antagonist was used in the contraction phase of ME usage (Wright & Drysdale 2008). (See Figs 8.7A,B.)
Figure 8.7 Fig. 8.7A shows MET treatment of piriformis using an antagonist contraction. Fig. 8.7B shows MET treatment of piriformis using a stretch following an antagonist contraction.
Caution – Stretching of tissues should be avoided: