Arthroscopically Assisted Treatment of Ankle Injuries
Keywords
• Ankle injuries • Arthroscopy • Ankle fractures • Intra-articular fractures
Ankle fractures that are displaced and unstable have traditionally required surgical intervention to obtain an anatomic reduction and stabilization with internal fixation (open reduction and internal fixation [ORIF]).1,2 This necessitates a surgical exposure of adequate size to visualize and reduce the fracture fragments as well as allow the delivery of appropriate fixation. The repair also requires inspection of the ankle articular surfaces for any damage. Chondral and osteochondral fragments, if identified, should be addressed with excision or repair. There is a biologic price for this strategy. Open techniques usually require extensive soft tissue dissection that can potentially compromise the blood supply to the osseous structures and affect healing. Arthroscopy is an expedient tool in the management of intra-articular fractures of the ankle. It can provide the surgeon with the ability to help anatomically reduce a fracture under direct visualization and sometimes be combined with a minimally invasive ORIF. It also affords the surgeon the ability to address any articular injury with minimal biologic risk.3,4
Contraindications: to using arthroscopic assistance
Surgical assessment
The patient initially requires a thorough physical examination coupled with appropriate radiographic evaluation of the ankle along with the leg or foot as indicated. With the patient hemodynamically stable, immobilization of the fracture is performed along with a closed reduction if necessary to relocate a subluxation or dislocation. A compressive dressing and splint/fracture brace is applied. Initial surgery performed within 6 hours of injury is ideal. If the surgery is delayed, then the timing of the procedure will depend on the recovery of the soft tissue to decrease the likelihood of postoperative wound problems.5 This principle of allowing the soft tissue to “settle” must be respected. For unusual adult fracture patterns and more routinely in specific pediatric ankle fractures, a computed tomography (CT) scan is required to fully observe the fracture configuration and aid with developing an approach to deliver fixation. The question then becomes which fractures may benefit from arthroscopic assistance, and also, which fractures can be successfully managed from a minimally invasive approach.
Pearls in arthroscopic technique
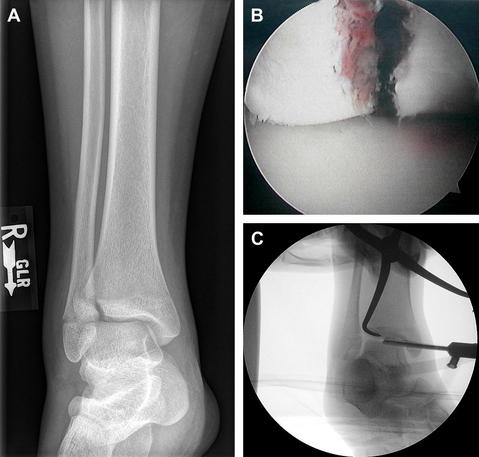
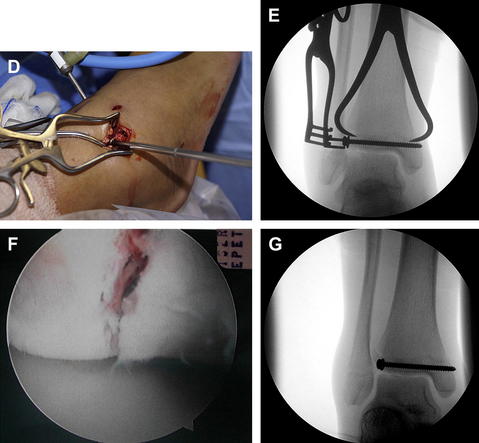
Large (4.0 mm) and small joint (2.7 mm) arthroscopes can be used depending on the size of the patient. Most fracture patterns can be visualized with the standard anteromedial and anterolateral portals. Occasionally, an accessory portal is necessary to aid in reduction or for an alternate view of the fracture. Gravity inflow is preferred, avoiding arthroscopic pumps that can increase inflow pressure resulting in fluid extravasation. Extravasation of the ingress fluid from the arthroscopic procedure can increase the risk of wound problems or compartment syndrome. It can also cause the soft tissue envelope to swell, making it difficult to palpate osseous structures for a minimally invasive ORIF. Two bags with 3 L of lactated Ringers solution is suspended 3 to 4 feet above the operating table. Inflow through the cannula and a separate portal for outflow aids with distention and visualization. Another problem can be the disruption of the capsule and ligaments that prevents distention by allowing fluid escape, limiting the ability to see. Generally with most injury patterns, the joint can be entered without any distraction, as an unstable mortise allows for easier passage of instruments. Distraction is occasionally needed to help gain access to the ankle joint (Fig. 1).6 It can be helpful in visualizing the posterior aspect of the ankle joint or examining the inferior tibial plafond. Upon entering the joint, one encounters varying degrees of hemarthrosis, synovium, and joint debris. This requires evacuation by joint lavage and the introduction of a synovial shaver. With joint debridement, the fracture will be visible. The fracture site can be debrided of hematoma and any entrapped periosteum with a dental pick. Certain fractures can now be reduced percutaneously with a pointed reduction forceps. The reduction is checked with arthroscopic and fluoroscopic control. If anatomically reduced, then internal fixation can be delivered.
Treatment of specific fractures
Pediatric Ankle Fractures
Nearly 40% of physeal injuries in children are ankle fractures and more than half of these occur in sports.7 With pediatric ankle fractures, the transitional fractures of Tillaux and the triplane fracture are amenable to athroscopically assisted percutaneous techniques. The Tillaux fracture is a Salter-Harris Type III fracture (Fig. 2).8 It is seen in the older adolescent, as it is the last part of the distal tibia epiphyseal plate to fuse. It usually occurs within a year of complete closure of the distal tibial physis. The injury mechanism is external rotation that produces a quadrilateral-shaped fracture fragment on the anterolateral aspect of the tibia. This fragment is displaced and rotated laterally with a gap separating the fragments but normally without step-off. A CT scan best demonstrates this fracture. An arthroscopic approach can easily visualize the fracture along the anterior aspect of the tibia and allow for debridement of the hematoma. A percutaneously placed pointed reduction forceps can reduce the fracture under arthroscopic and fluoroscopic visualization. A cannulated lag screw can then be delivered percutaneously under fluoroscopic control. The screw can be perpendicular to the ankle joint or angled slightly superiorly. Crossing the epiphyseal plate with a screw is not an issue, as this is the last portion of the physis to close.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree