Abstract
Exercise training, associated with therapeutic education, is the main axis of cardiac rehabilitation (CR) programs. The aim of this study was to review the literature for descriptions of the various assessments of exercise tolerance used to prescribe exercise intensity during CR. A secondary objective was to attempt to formulate a rational practice with these assessments in CR programs.
1
Introduction
Exercise training, associated with therapeutic education, is the main axis of cardiac rehabilitation (CR) programs. By improving physical abilities of patients, exercise training aims to facilitate activities of daily living as well as social and occupational integration . Furthermore, through its systemic physiological effects (reduced hyperadrenergy, endothelial dysfunction, insulin resistance, inflammation, hypercoagulability) and its contribution to the control of risk factors, exercise training plays a major role in decreasing CR-related morbidity and mortality .
Rehabilitated patients are extremely heterogeneous, so exercise training must be individualized to have optimal efficacy with the lowest risk. This individualization is based on the frequency, intensity, time and type (FITT) principles . Some of these 4 factors are rather simple to personalize, depending on the patient and the fixed objectives. The training involves first the type of exercise to perform: global training involves a large number of muscles (e.g., exercises on an ergometric bicycle or treadmill) and resistance training restricted to some muscle groups. Concerning more exactly the mode of muscle contraction, concentric exercises are principally recommended (the exact place of the eccentric or the isometric exercise has yet to be specified). The organization of CR sessions in terms of frequency (3 to 5 sessions a week) and duration (30 min to 2 h) is rather easy to modulate, depending on the situation encountered, for programs that take place over periods fluctuating from 2 to 3 months .
Paradoxically, the personalization of exercise intensity–an apparently essential aspect–is the least standardized. Exercise intensity concerns the targeted objectives as much as the ways to achieve them. The objectives can be an improvement in strictly aerobic capacities based on moderate intensity training to facilitate activities of daily living or conversely, the search for maximal performance by high-intensity exercises. The exercise intensity to propose can range from 40 to 80% and even 90 or 95% of maximal capacity.
The most appropriate factors for individualizing this training intensity remain questionable. This customization is based on, in addition to disability status and comorbidities, a preliminary evaluation of the tolerance to effort, for which cardiopulmonary exercise test (CPET)–besides its role in risk stratification–is still the gold standard . Indeed, the test can be used to define a target heart rate (HR) to reach during exercise training. However, alternative methods are available, some dealing with physiological parameters different from HR. Sometimes these procedures are more practical and less expensive and require less expertise and fewer technological resources.
The aim of this study was to review the literature for descriptions of the various assessments of exercise tolerance that can be used to prescribe exercise intensity during CR. A secondary objective was to attempt to formulate a rational practice with these assessments in CR programs.
2
Methods
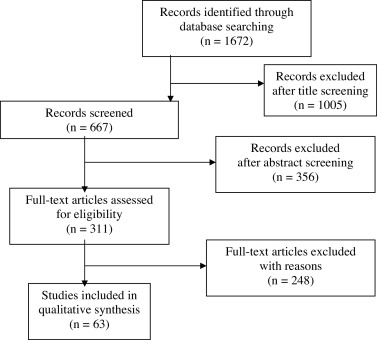
We searched MEDLINE via PubMed for articles in English or French that were published from 1970 through January 2015 by using the keywords “Cardiovascular Diseases/rehabilitation”[Mesh] AND (“aerobic test” OR “endurance test” OR “exercise intensity” OR “exercise prescription” OR “muscle testing” OR “heart rate monitoring” OR “walk test” OR “perceived exertion”). We had no restriction on study methods but we selected articles describing the evaluation of exercise tolerance only during CR and identifying physiological signals tested for the personalization of the exercise. The flow of selecting articles was according to the PRISMA statement . Articles were identified first on the basis of the title, then the abstract, and then the full text of identified articles was assessed.
2
Methods
We searched MEDLINE via PubMed for articles in English or French that were published from 1970 through January 2015 by using the keywords “Cardiovascular Diseases/rehabilitation”[Mesh] AND (“aerobic test” OR “endurance test” OR “exercise intensity” OR “exercise prescription” OR “muscle testing” OR “heart rate monitoring” OR “walk test” OR “perceived exertion”). We had no restriction on study methods but we selected articles describing the evaluation of exercise tolerance only during CR and identifying physiological signals tested for the personalization of the exercise. The flow of selecting articles was according to the PRISMA statement . Articles were identified first on the basis of the title, then the abstract, and then the full text of identified articles was assessed.
3
Results
The selection of articles is in Fig. 1 . The analysis of the 63 articles allowed for retaining 4 main physiological markers that can be used to assess exercise tolerance and to tailor training intensity for patients during CR: HR, perceived exertion, muscle capacity (work rate, muscle strength), and walking speed.
3.1
HR analysis
HR is the most easily assessable parameter of exercise tolerance in routine clinical practice, particularly by using an HR monitor, an inexpensive device to personalize exercise training by determining a target HR. Understandably, the strategies based on the use of the HR are the most frequent.
3.1.1
HR assessed by symptom-limited exercise testing
Although electrocardiography (ECG) stress testing is not essential, it is generally performed at the beginning of a CR program to determine 2 essential parameters: maximal heart rate (HR max ) and maximal workload. Furthermore, it improves the safety of exercise training by eliminating myocardial ischemia, cardiac arrhythmia or effort hypertension, which can require an adaptation of the drug therapy or can contraindicate CR . ECG stress testing contributes to cardiac risk stratification, but during CR it is not designed for diagnosis of the cardiovascular disease and thus it is performed without preliminary modification of drugs.
The use of a percentage of the HR max assessed by a stress test has been proposed for several years to individualize exercise training intensity . The current recommended training HR is between 70 and 85% of the HR max . However, this procedure, though often used in many experimental studies, is criticized because it does not account for chronotropic specificity , which varies considerably in patients with cardiovascular disease. Indeed, the chronotropic competence of these patients is often altered by multiple factors: cardiac alterations, dysfunction of the autonomic nervous system, drug interactions (e.g., beta-blockers, calcium-channel blockers, ivabradine, amiodarone), and metabolic comorbidities such as diabetes. Accordingly, the recommendation is to account for the HR reserve, the difference between HR max and resting HR, by the Karvonen formula : training HR = rest HR + % (HR max – rest HR). The percentage to apply depends on the target intensity of exercise training: from 50% for low intensity to 90% for high intensity. To avoid underestimating the training HR in patients receiving beta-blockers, a modified Karvonen formula based on the HR at the anaerobic threshold was proposed: training HR = rest HR + 0.8 (HR max – rest HR) .
Gas exchange can be continuously assessed during CPET to confirm that the test was ended at exhaustion (a final respiratory exchange ratio > 1.10 being necessary) and as a result, that the maximal aerobic capacity (peak oxygen uptake: VO 2peak ) is measured accurately, thus defining more rigorously the corresponding HR max . Another additional gas exchange measures is the first ventilatory threshold, a metabolic marker of adaptation to effort, by specifying the intensity of the exercise from which an additional anaerobic power production is associated with the aerobic energy supply. Using the HR corresponding to this threshold seems to ensure safe and effective aerobic endurance training in patients with coronary disease and chronic heart failure . However, in determining the first ventilatory threshold, the method becomes cumbersome and expensive; we lack clear evidence that in current practice the procedure is superior to HR assessed by conventional stress testing . When the targeted intensity of training is greater than the first ventilatory threshold, another limitation in the use of the VO 2 to personalize a constant-work-rate exercise is the “slow component” of the VO 2 kinetics, appearing between 2 and 3 min of exercise and corresponding to a loss of muscle efficiency. Consequently, the VO 2 and HR steady state are delayed and higher that expected by the CPET, thereby reducing the duration of the exercise . However, the measurement of VO 2peak would be most useful for patients with chronic heart failure, because it quantifies metabolic deconditioning according to the 4 stages of the Weber classification and can be used to evaluate progress during training .
Such maximal exercise tests are reserved for specialized structures and require expensive resources (trained staff and specific equipment). They cannot be repeated regularly during CR to tailor intensity of exercise training according to the progress of patients. In addition, they could be deleterious for patients with debilitating disease, particularly the oldest patients, who often have musculoskeletal damage and experience various cardiac events. Moreover, the maximal tests are not really representative of functional capacities in real life . Some submaximal field tests have been suggested as surrogates to a maximal stress test dedicated to the analysis of HR adaptation to effort, most of them walking tests. Indeed, walking is a physiological activity and is a better example of human motion than constrained effort such as walking on a treadmill or use of a cycloergometer .
3.1.2
HR assessed during functional tests
The 6-min walk test is a fixed-duration walking test that was the first to be validated as a functional test dedicated to assessing exercise tolerance in patients with cardiovascular disease, particularly chronic heart failure . The patient is told to cover the greatest possible distance on a flat indoor walking track in 6 min. It is an easy-to-perform and safe submaximal test widely used to evaluate the impact of exercise training on endurance . HR measured during the test has been used to personalize training, to improve aerobic capacity , with even greater efficacy to achieve HR training than a conventional protocol based on a percentage of the maximal capacity . The main limitation of this test to tailor the CR is probably the persistent ambiguity concerning the instruction of targeted walking speed, which determines the measured HR: sometimes brisk walking at intensity close to maximal capacity , and more often, free walking velocity (“comfortable”) staying strictly within aerobic conditions .
The 200 m fast walk test is a fixed-distance walking test corresponding to an intense but submaximal effort. It is well tolerated in patients with stable coronary disease . The subject must walk as quickly possible, without running, on a flat 50 m indoor walking track, encouragement being given at mid-distance. In one study the corresponding HR was used to personalize high-intensity interval training in patients with coronary disease. It had the same tolerance and impact on walking performance as conventional aerobic training but with a greater increase in VO 2peak .
3.1.3
Predicted HR
Using a percentage of a predicted HR max could be an interesting alternative to a ECG stress test to prescribe training. On the basis of the inverse relationship between age and HR max , numerous predictive equations of HR max that account for only age have been proposed, the first being the Fox formula (HR max = 220 – age) . However, the prediction error of these equations is too great to be applicable in current practice, particularly in patients with coronary disease . The main reason for this limitation is probably that these equations do not incorporate the great diversity of chronotropic competence in these patients. For the same reason, and logically, the unsuitability of these predictive formulas to prescribe exercise intensity was confirmed .
Parameters of walking tests could improve the predictive value of these formulas because they incorporate chronotropic features . Indeed, a model that combines HR measured during the 200-m fast test and age seems to be more efficient than a conventional formula that includes only age (e.g., the Fox or Tanaka equation) to predict HR max . As well, the target training HR defined from the HR reserve calculated by use of this new predictive model was statistically correlated with that established with measured HR max by a stress test. If confirmed in a large number of patients, this new approach could become an alternative to a stress test.
3.2
Perceived exertion: an alternative to HR
Although the HR is an effective approach to personalize exercise training, it is not applicable for some types of patients often referred for CR: those with atrial fibrillation, pacemakers, and chronotropic incompetence (a small alteration in HR can reflect a large change in workload). In addition, CPET is still not possible and the HR max is seldom known. The rate of perceived exertion (RPE) could be a surrogate because it is associated with the level of cardiorespiratory demand, despite its subjective component . RPE is a valid way to regulate training intensity , independent of exercise duration . The Borg scale was the first to be used in this indication .
3.2.1
Borg scale
The 6- to 20-point Borg scale has been found reliable for assessing subjective RPE in a healthy population . This score, used for prescribing exercise intensity in patients with coronary disease included in a home CR program, was found as effective as a conventional program (tailored by a percentage of HR reserve), by improving physical capacities at the same level . An RPE of 12–13 (“somewhat hard”), corresponding to the ventilatory threshold in healthy subjects , seems an effective means to individualize aerobic training in patients with coronary artery disease and chronic heart failure . However, there is a risk of overtraining for patients with heart failure at such levels of intensity . The choice of a lower intensity is possible (RPE 9–11 on the Borg scale), particularly for eccentric training, which is associated with lower demand on the cardiorespiratory system than concentric training . In contrast, in high-intensity interval training, the use of RPE 17 (“very hard”) results in exercise intensity below the target HR . Another limit to the applicability of the Borg scale is its readability for patients with impaired vision . Also, the observed variability in the scale seems to be an obstacle to its use in routine practice .
3.2.2
Talk test
This test is based on the swift increase in breathing rate above the first ventilatory threshold that causes difficulty in talking . It consists of an incremental submaximal test on a treadmill or a cycloergometer with 1-, 2- or 3-min stages. During the last part of each stage (10–30 s), the patient is asked to read a standard paragraph (about 30–50 words), then answer the question “Were you able to speak comfortably?” If the subject gives a response other than a positive “yes” (e.g., “yes but” or “I’m not sure”), the intensity is coded as equivocal and approximates the first ventilatory threshold . This test is well tolerated in patients with coronary disease and has good relative reliability .
Use of the HR or workload corresponding to an equivocal stage of the talk test to prescribe exercise intensity results in intensities of 60 to 90% of HR reserve . Training prescribed at the intensity associated with the last positive stage (unequivocal response “yes”), and even more at the preceding stage, is the best tolerated .
The 2 main limits of the talk test are the need to have the corresponding HR to personalize the training and the observed excessive variability of results of this subjective test in rehabilitated patients . When HR is unavailable (e.g., atrial fibrillation), a surrogate to the talk test is to perform exercise training at an intensity compatible with a comfortable conversation. Finally, the talk test is not a practical tool for customizing high-intensity exercise such as interval training : it must be reserved for predominantly aerobic training.
3.3
Assessment of muscle capacity
3.3.1
A percentage of maximal workload to customize global training
The work rate (as a percentage of maximal work load) is rarely implemented as the only quantitative tool to prescribe the intensity of global training in patients with coronary disease because it represents only an approximation of exercise capacity in that it does not account for cardiorespiratory adaptation. It is not a practical simplification because it requires a stress test to assess the maximal tolerated workload, without cardiovascular intolerance, and a percentage of this achieved measure has to be determined as a threshold for training on an ergometer or treadmill . The work rate can be used to tailor fitness training in healthy subjects, but in CR, it is disconnected from cardiovascular parameters.
3.3.2
Muscle strength to personalize resistance training
The health-related effects of resistance training are well documented in patients with cardiovascular disease . Dynamic exercises (concentric and eccentric) are preferred to isometric exercises because of the deleterious impact of the latter .
The HR response is generally lower to resistance training than global training. To avoid cardiac events and musculoskeletal complications, low to moderate initial resistance training, corresponding to 30 to 50% of the maximum voluntary contraction, is recommended. With CR progression, muscle load can be increased to 50 to 80% of the maximum muscle strength . Consequently, for optimal training prescription of the muscle groups involved (e.g., biceps curl, triceps extension, knee extension, bench press, latissimus dorsi pull-down), entry muscle strength testing is justified: usually 1-repetition maximum testing is performed, with if possible, a periodic evaluation, to accurately adjust the resistance training program, without generating significant muscle injury or soreness .
When a preliminary muscle strength test is not available, as for global training, the patient can adapt the resistance training intensity according to the RPE: the intensity can be between RPE of 11 (“fairly light”) and 13 (“somewhat hard”) on the Borg scale . However, eccentric training has a specific characteristic. Indeed, with the slightest cardiorespiratory demand during eccentric exercise, the usual criteria for the personalization of conventional (concentric) resistance training, namely the HR and the perception of fatigue at these intermediate levels, is inappropriate. Therefore, a low RPE (9–11 on the Borg scale) is more appropriate to avoid muscle damage .
3.4
Walking speed
Walking speed can be used for training customization in a way that is separate from the corresponding HR.
3.4.1
Self-selected walking velocity
The “comfortable” walking speed corresponds to the best bioenergetic efficiency of walking in a steady state of aerobic metabolism . It is associated with functional capacities and global health status and is related to age and gender . Free walking is well tolerated and thus practiced with pleasure; it facilitates compliance with a prolonged modification of the lifestyle and is an effective strategy for outdoor training for patients with coronary disease .
3.4.2
The shuttle-walking test
The shuttle-walking test is an incremental exercise test that is well tolerated in patients. The subject walks between 2 ground markers set 9 m apart and has to pass each marker in time with a sound pulse from an audiotape; the speed increases every minute until exhaustion . The test seems appropriate as an alternative to a conventional maximal exercise test for patients with chronic respiratory diseases and it can be used to assess the effects of exercise training in the context of a CR program (increase in distance walked) . To our knowledge, the test has been used only to personalize exercise training during a respiratory rehabilitation program: intensity was fixed at 70% of the peak speed for a continuous walking exercise, aided by a metronome, with frequency set according to a prior 12 m walk test at the usual pace, which allowed for calculating the step length . The likely explanation for the low use is the complexity of this procedure for application in current practice. In addition, the speed values of a shuttle walk test are not transferable to a treadmill because of the fundamentally different energy demands of these 2 types of effort .
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





