Chapter 3 Assessment
Introduction
Competency in clinical assessment (in varying degrees) is an essential requirement of any practising healthcare professional, including practitioners of CAM. This is because assessment data directly inform clinical decision making, determining for instance when a clinician should initiate, continue or cease treatment, or when to refer or involve others in the multidisciplinary team. Even though the acquisition of pertinent knowledge and skills in clinical assessment is a vital first step to developing competence in this area, it is important to note that assessment is not just a step-by-step data collection exercise, but a process that requires a high level of critical thinking. Put simply, assessment should not be about ticking all the boxes, but about analysing and evaluating the data to determine what additional techniques and tests would support or refute suspected or possible diagnoses. This ongoing evaluation of the data is known as critical analysis, which is vital given that many client health problems can be complex and fraught with uncertainty. Integrating critical analysis into a comprehensive and systematic clinical assessment framework also promotes the efficient use of practitioner and client time, and healthcare resources. Before discussing such a framework, it is important to understand the types of data that can contribute to the clinical assessment.
Types of assessment data
There are several types of data that can be acquired during a clinical assessment. Each form can be distinguished by the means in which it is collected, interpreted and utilised. Recognising the merits and limitations of these different types of data is critical to understanding the assessment process. The first of these types is subjective data. This category of data is defined as that which is informed by personal opinion, feelings and perceptions. Subjective data are typically obtained during client and family interviews, and are the predominant form of data collected during a health history. While subjective data provide valuable information about a client’s lived experience, such as the duration and severity of a symptom, this form of data is easily confounded by personal bias, which raises concern about the accuracy and consistency of such information.1,2
The other major form of data that can be collected during the assessment process is objective data, which is defined as that which is observable, verifiable, measurable and not distorted by subjective impressions. Objective data are often acquired using recognised measures such as pathology tests, radiological imaging and physical examination techniques; as a result it is less likely to be tainted by personal bias. As such, the validity and reliability of objective data are greater than that obtained by subjective data. What this means is that clinicians should give higher priority to the collection of objective data over subjective information during the clinical assessment.3,4
CAM assessment process
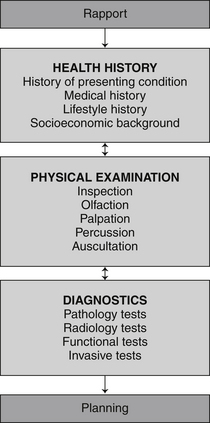
Clinical assessment is a pivotal component of DeFCAM in that it directly informs every succeeding stage of the process. For this reason it is necessary that client assessments are comprehensive and complete, and that they follow the principles of rigorous clinical assessment (see Table 3.1). One way practitioners can minimise the risk of omitting important data is to adopt a systematic approach to clinical assessment. The head to toe and body systems approaches are two such processes used in clinical practice. The problem with these methods is that neither presents a comprehensive approach to clinical assessment. The CAM assessment process is a more complete assessment process, not only because it integrates additional elements of the health history (such as socioeconomic background) and physical examination (such as olfaction), but also because it encompasses an essential diagnostics phase. These interrelated stages of the process and the non-linear nature of the approach are illustrated in Figure 3.1.
Table 3.1 Principles of rigorous clinical assessment
| Data should be | accurate |
| complete | |
| comprehensive | |
| interpreted appropriately | |
| corroborated by supporting evidence | |
| objective | |
| systematic | |
| Methods should be | ethically sound |
| reliable | |
| safe | |
| sensitive | |
| specific | |
| valid |
Health history
Implementing measures that build client rapport before and during the clinical consultation are critical to developing client trust, improving communication and enhancing the accuracy of acquired information.5 This is particularly important when completing a health history because subjective data often dominate this stage of assessment. It is probable that the quality of clinical assessments will be improved if clinicians become more consciously aware of the many factors that improve client rapport (see Table 2.1) and, more importantly, attempt to address these elements throughout the consultation.
Asking a clinician to speculate on the aetiology of a disease when the history of a presenting complaint is described as mild (severity), dull ache (quality) to the left lower abdominal quadrant (location) would be difficult and inappropriate. On the other hand, if the history added that the discomfort had been present for the past 3 months (onset), occurred intermittently every day (frequency) for approximately 1–2 hours at a time (duration), was non-radiating (radiation), improved by defecation (ameliorating factors), worsened by stress (aggravating factors) and was accompanied by bloating and flatus (concomitant symptoms), then a clinician may be able to consider possible hypotheses, such as irritable bowel syndrome. This description of the presenting complaint is summarised in Table 3.2.
Table 3.2 Core components of the presenting complaint description (ReLOAD FACQS)
| Re | Radiation |
| L | Location |
| O | Onset |
| A | Aggravating factors |
| D | Duration |
| F | Frequency |
| A | Ameliorating factors |
| C | Concomitant symptoms |
| Q | Quality |
| S | Severity |
Once the presenting condition has been adequately described the clinician can start to explore other factors that may contribute to the chief complaint, the client’s state of health and wellbeing, and the overall plan of care. These determinants can be separated into medical, lifestyle and socioeconomic factors. With reference to the medical determinants, these include family history of illness, allergies and sensitivities to foods, medications and environmental agents, over-the-counter and prescribed medications, complementary medicines and supplements, current and previous medical conditions or illnesses, and history of surgical or investigational procedures (see Table 3.3). For paediatric clients, it is important to also consider immunisation, birth, breastfeeding, growth and development history.
Table 3.3 Medical components of the health history (FAMMS)
| F | Family history |
| A | Allergies and sensitivities |
| M | Medications |
| M | Medical conditions |
| S | Surgical and investigational procedures |
Another important component of the health history is the client’s lifestyle history. A lifestyle history includes details about diet and fluid intake (including quality and quantity of consumed goods), illicit drug use (including type, route and frequency of use), smoking status (including strength and quantity), frequency and duration of exercise, alcohol use (including type, quantity and frequency), quality and duration of sleep, and entertainment and recreation choices (see Table 3.4).
Table 3.4 Lifestyle components of the health history (DISEASE)
| D | Diet and fluid intake |
| I | Illicit drug use |
| S | Smoking status |
| E | Exercise frequency and duration |
| A | Alcohol use |
| S | Sleep quality and duration |
| E | Entertainment or recreation choices |
The final part of the health history, socioeconomic background, is a particularly important component as many of the factors within this category are likely to affect a client’s capacity to understand and/or comply with treatment. This category includes information about the client’s family environment (including living arrangements, proximity of family, family dynamics), occupation and employment status, religion and cultural background, level of social support from family, friends and/or external agencies, level of educational attainment (including primary, secondary and tertiary level education), and residential and/or work environment (see Table 3.5). For paediatric clients, information also should be obtained about childcare arrangements and school performance.
Table 3.5 Socioeconomic components of the health history (FORSEE)
| F | Family environment |
| O | Occupation and employment status |
| R | Religion and cultural background |
| S | Social support |
| E | Education |
| E | Environment (work and residential) |
In an attempt to quantify the severity and/or impact of the presenting condition, some practitioners choose to use one of a number of clinical assessment tools, such as pain, depression, anxiety, stress and irritable bowel syndrome scales. Although such tools may be useful in providing clear, concise and measurable data about the presenting problem, which may help in the evaluation of client care, the validity and reliability of many evaluation tools are not well established. If the accuracy of a tool can be determined and the data are found to be reasonably consistent, then that assessment instrument may have a place in the CAM assessment process. Examples of tools that can be used in the assessment of conditions pertinent to each body system are outlined in the second half of this chapter.
Physical examination
A complete and comprehensive health history should provide the clinician with a detailed description of the client’s presenting condition and enable the practitioner to formulate a number of assumptions about the aetiology of the complaint. To determine which, if any, of these hypotheses are likely to become probable diagnoses, the clinician will need to test the assumptions by acquiring additional data. The source of such data can be derived from the physical examination (for a more detailed discussion of assumption or hypothesis processing, see chapter 4).
The physical examination generally involves some degree of physical contact between the practitioner and client, so it is critical that the clinician establishes some level of rapport and trust with the client (see chapter 2) and has at least obtained verbal consent from the client prior to commencing the examination. Appropriate hand washing, infection control measures, privacy, client conversation, instrument use, draping, level of client contact and exposure are also important measures for reducing a client’s risk of physical or psychological harm. Because inappropriate physical contact and professional misconduct are major causes of complaint against CAM practitioners,6–8 these strategies may also serve to protect clinicians from unnecessary professional and legal action. To further protect the client and practitioner from immediate and enduring harm, it is important that clinicians also recognise their professional boundaries and the limits to their scope of practice, and, where appropriate, refer clients to relevant health professionals for further assessment. For paediatric clients, it is important that a parent or guardian is present whenever possible.
Once these factors have been taken into consideration, a practitioner can commence the physical examination. The first part of this assessment, which begins from the time the practitioner makes visual contact with the client, is inspection. This visual assessment of the client incorporates a general and a specific component. The general inspection examines the client’s broad state of health by observing features such as posture, gait, affect, body language, physical guarding and functional capacity, which can alert the clinician to possible causes of the presenting condition as well as related comorbidities. Specific inspection focuses on the presenting complaint and associated body systems, and requires the clinician to make observations about pertinent structural and functional manifestations (including normal and atypical signs), such as a flat or distended abdomen and pink or pale skin colour.
The tactile component of the physical examination, known as palpation, uses deep and light touch, where relevant, to acquire information about the size, depth, texture, temperature, mobility, firmness and tenderness of the presenting condition.9 Apart from corroborating observed data, palpation adds necessary detail about the condition of the underlying structures, including muscles, bones, organs and blood vessels. The tactile examination of pulses, masses, lesions and areas of localised pain are some examples of where this technique maybe applied. Palpation also provides supporting evidence for pathological processes, such as inflammation, infection and carcinogenesis. A good case in point is erythema. The presence of localised erythema to the lower limb, for instance, says very little about the aetiology of the condition, but when combined with palpable heat and tenderness, suspicions of inflammation and/or infection may be confirmed.
Complementing palpation is percussion, an examination technique that uses touch (i.e. tapping the area of interest) and sound, specifically, vibration, to define the density of the underlying structure, in particular, whether the structure is gas, fluid or solid.10 This information can help a clinician distinguish between certain pathologies without relying on invasive or costly diagnostic tests in the early stages of assessment. A particularly important place for percussion is in the early detection of pneumonia, pneumothorax, internal bleeding and organomegaly. With reference to respiratory disease, percussion can be especially helpful in differentiating between generally less fatal conditions such as lobar pneumonia (manifested by percussive dullness), and life-threatening emergencies such as pneumothorax (manifested by hyper-resonance).
The data collected from a comprehensive health history and physical examination can be particularly helpful in informing the CAM practitioner about possible diagnoses, as well as the need for referral. The following example illustrates this point further. A brief clinical assessment that identifies the presence of cough and chest discomfort may mislead a practitioner into believing that a client has asthma or respiratory tract infection. A more detailed assessment that identifies the additional presence of haemoptysis, hoarseness, weight loss, dyspnoea, digital clubbing and supraclavicular lymphadenopathy, may direct a practitioner to a more probable diagnosis of lung cancer, resulting in prompt referral to an allopathic medical practitioner and the avoidance of unnecessary delays in treatment. Other clinical manifestations that should alert a clinician to the possibility of more serious pathology, and the need for prompt referral to an appropriate practitioner, are bleeding (such as haemoptysis, melaena and haematuria), escalating pain (including central chest pain, cephalgia and abdominal pain), altered levels of consciousness, seizures, unresolving masses, rapid weight loss and petechiae.
Diagnostics
Investigations not typically performed by CAM practitioners, but for which clinicians may need to interpret findings or refer clients on, are invasive procedures. These investigations, often used in conjunction with pathology tests, provide important information about the structure, function and/or pathology of the presenting complaint, although when compared with other diagnostic methods, most invasive tests pose a greater risk of harm to the client, including an increased risk of pain, infection and haemorrhage.
The other category of diagnostic investigation, which is commonly used by CAM practitioners, is the miscellaneous tests. Despite the long history of use of these tests within CAM, particularly methods such as iridology, kinesiology, Vega testing and pulse diagnosis, there is insufficient clinical evidence to support their use. This is not to say that these methods are ineffective or should be dismissed in clinical practice, only that further research is needed to evaluate the validity and reliability of these procedures. Miscellaneous tests are not confined to CAM diagnostics: this category also captures investigations that do not nest within the other four diagnostic categories, including electrodiagnostics and sleep studies. Examples of tests that fall into the five diagnostic categories are listed in Table 3.6.
Table 3.6 Examples of diagnostic tests that may be requested, performed or interpreted in CAM practice
| Pathology tests | Carbohydrate breath test |
| Complete blood examination (CBE) | |
| Culture and sensitivity testing (C&S) | |
| Glycated haemoglobin (HbA1c) | |
| Lipid studies | |
| Liver function test (LFT) | |
| Nutrient levels (iron studies, hair mineral analysis) | |
| Oral glucose tolerance test (OGTT) | |
| Semen analysis | |
| Thyroid function test (TFT) | |
| Urinalysis (UA) | |
| Functional tests | Adrenal hormone profile |
| Bone metabolism assessment | |
| Comprehensive detoxification profile (CDP) | |
| Comprehensive digestive stool analysis (CDSA) | |
| Intestinal permeability (IP) test | |
| Pulmonary function test (PFT) | |
| Urodynamic studies | |
| Radiological tests | Computed tomography scan (CT) |
| Contrast studies | |
| Magnetic resonance imaging (MRI) | |
| Mammography | |
| Positron emission tomography (PET) | |
| Radiograph/X-ray | |
| Ultrasound (US) | |
| Invasive tests | Allergy skin testing (prick-puncture test) |
| Arthroscopy | |
| Biopsy | |
| Colonoscopy | |
| Endoscopy | |
| Laparoscopy | |
| Lumbar puncture (LP) | |
| Miscellaneous tests | Electrodiagnostics (electrocardiograph) |
| Iridology | |
| Plethysmography | |
| Pulse diagnosis | |
| Quantitative sensory testing (QST) | |
| Sleep studies |
Cardiovascular system assessment
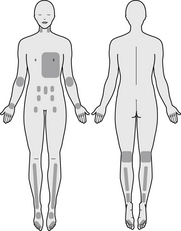
These points should be taken into account when conducting a comprehensive assessment of the cardiovascular system. An outline of the regions pertinent to cardiovascular system assessment is illustrated in Figure 3.2.
Health history
History of presenting condition
Identify the client’s primary problem and establish the location, onset, duration, frequency, quality and severity of the sign or symptom, the presence of radiating symptoms (e.g. chest pain radiating down the left arm or up the neck may indicate myocardial ischaemia), any aggravating or ameliorating factors (such as walking, stress, rest or leg elevation) and any concomitant symptoms (including shortness of breath, fatigue, chest pain, palpitations, claudication, paresthesias and syncope).
Lifestyle history
Identify any factors that may increase the client’s risk of CVD, such as obesity, tobacco use (including number and strength of cigarettes inhaled in a day), alcohol consumption (including number of standard drinks and type of alcoholic beverage consumed in a day), illicit drug use (including type, route and quantity of drug used per day), diet and fluid intake (such as sodium, omega 3 fatty acids, saturated fat, fibre, fruit and vegetable consumption), quality and duration of sleep (e.g. broken sleep, sleep apnoea) and frequency and duration of exercise.11
Physical examination
Inspection
Observe for any signs of impaired cardiovascular function, such as xanthomata (hard, yellow masses that are pathognomonic of familial hypercholesterolaemia),10 digital clubbing (an abnormal enlargement of the terminal phalanges that may be a sign of chronic hypoxia), splinter haemorrhages of the nail bed (present in infective endocarditis12), dyspnoea, pallor or cyanosis (may be observed in hypoxia, anaemia, vasoconstriction or vascular occlusion), Lichstein’s sign (oblique, bilateral earlobe crease observed in people over 50 years of age with significant coronary heart disease),12 dependent oedema (may be indicative of chronic venous insufficiency or right-sided heart failure), leg ulceration (may be indicative of peripheral vascular disease) and lower leg varicose veins and ochre pigmentation (both signs suggest the presence of chronic venous insufficiency). The presence of chest scars (from sternotomy or pacemaker insertion) and/or deformities (such as pectus excavatum or pectus carinatum) may also draw attention to the possibility of cardiovascular defects.
Palpation
Examine major pulses of the neck (carotid), chest (cardiac apex), upper limbs (brachial, radial, ulnar) and lower extremities (femoral, popliteal, posterior tibial, dorsalis pedis) and note the rate, rhythm and amplitude of each pulse, as well as the presence of any thrills or palpable vibratory sensations (thrills are indicative of turbulent blood flow). Assess the peripheries for temperature (cool hands and feet may be indicative of cardiac failure or peripheral vascular disease) and pitting oedema (may indicate the presence of chronic venous insufficiency or right-sided heart failure). In terms of cardiac function, identify the position and diameter of the point of maximum impulse (PMI) (a laterally displaced or enlarged PMI is suggestive of cardiomegaly)10 and the presence of thrills or increased pulse intensity over the aortic area (may suggest the presence of aortic dilatation), pulmonic area (may be indicative of pulmonary artery dilatation), mitral area (may be indicative of mitral stenosis or regurgitation) and tricuspid area (may be a sign of tricuspid stenosis or regurgitation).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree