Practical Aspects of Foot and Ankle Arthroscopy
Keywords
• Arthroscopy • Foot • Ankle
Arthroscopy of the foot and ankle, although sometimes technically challenging, is a useful tool for the foot and ankle surgeon. Burman1 was the first to attempt arthroscopy of the ankle joint in 1931 and surmised that it was not a suitable joint for arthroscopy because of its narrow intra-articular space. With the development of smaller-diameter arthroscopes and improvements in joint distraction techniques, Watanabe2 was the first to present a series of 28 ankle arthroscopes in 1972.
Instrumentation
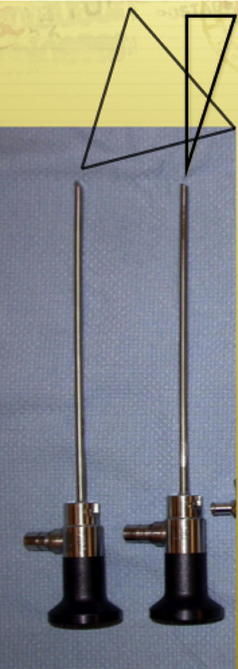
The arthroscope ranges in size from smaller than 1.5 mm in diameter to 7.3 mm; the larger the diameter of the scope, the larger the viewing surface, which increases exponentially (surface area = πr2). A 4-mm-diameter scope is typically used for ankle arthroscopy (Fig. 1). The advent of wide-angled scopes has allowed the development of ankle and small joint arthroscopy. Traditional arthroscopes have the lens angled at 90° to the long axis of the scope. However, the smaller-diameter scopes are cut at 30° and 70° to the long axis of the scope, giving a larger viewing surface and improved visibility in these small spaces. The 30° and 70° scopes have different viewing fields. The 30° scope allows the arthroscopist a field of vision in line with the scope and 30° to the periphery, whereas the 70° scope allows a field of vision 70° to the periphery but not directly ahead (Fig. 2).
Hand Instruments
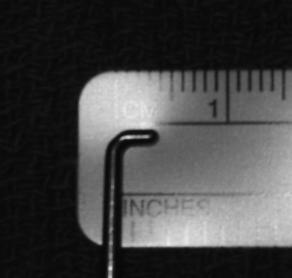
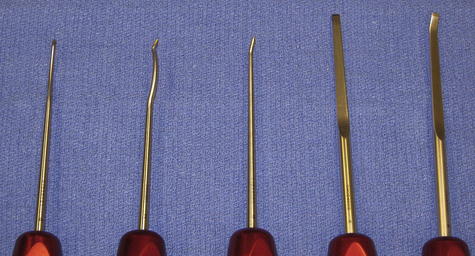
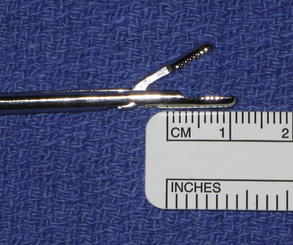
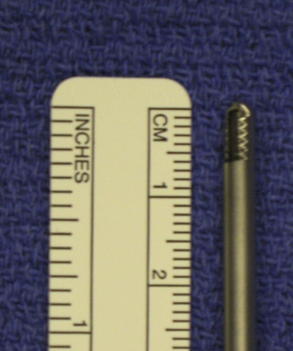
A variety of instruments have been made for arthroscopy. For ankle arthroscopy, instruments with a diameter less than 5 mm are ideal, and for smaller foot joints, a diameter less than 3 mm is ideal. The typical nonmotorized hand instruments available are probes, graspers, curettes, knives, osteotomes, gouges, punches, rongeurs, and magnetized rods (Figs. 3–7). Probes are often marked as a measuring device in 1- to 2-mm increments and also allow the size of lesions to be measured.
Power Instruments
Motorized instruments (cutters, shavers, and burrs/abraders) are often more efficient especially for debriding synovitis and fibrous bands as well as removing osteophytes. They include an aspiration component when attached to suction, which brings the tissue closer to the cutting edge of the instrument. There are various types of shavers including side cutting, open ended, and full radius. The side-cutting shaver has a small window that does not allow exposure to the blade’s distal tip. These are the least aggressive of the power instruments. The open-ended shaver is the most aggressive and has the distal tip of the blade exposed. Probably the most commonly used is a combination of the 2 types, which is called a full-radius shaver. It has only partial exposure of the tip of the blade and the side-cutting window (Figs. 8 and 9). The full-radius shavers are either smooth (traditional type) or with incisors. The incisor types are either single or double incisor, meaning that both the barrel and the blade have teeth for a double incisor and only the blade has incisors on a single incisor. Typically, the power setting used is between 1500 and 3000 rpm. If the rotation of the blade is too fast, it will not allow the instrument to pull adequate tissue into the device.
Thermoablative Tools
Other tools available to the arthroscopic surgeon include arthroscopic radiofrequency wands and, to a lesser extent, holmium-YAG laser systems that can vaporize, shrink, coagulate, and even weld tissue. Although arthroscopic laser technology has been available for more than 15 years, it remains controversial because it is expensive, requires special training, and remains unproven regarding its benefits.3 In recent years, radiofrequency wand technology has advanced significantly to effectively manage soft tissue abnormalities, especially in a cleanup role after the bulk of the soft tissue has been removed using a shaver or an ablator. The tips of the instruments vary in size to adapt to small-sized and medium-sized joints. Proper fluid management is important to regulate intra-articular temperature with these devices; this is combined with surgeon-controlled power adjustments to match tissue density and response to thermoablation. Some radiofrequency wands are aspirated to allow for suction application, which assists with fluid flow management, and to draw tissue into the wand tip. These suction types can also help to control intra-articular temperature because of the evacuation of heated fluid.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree