Fig. 16.1
AP (left) and lateral radiographs (right) of a TKA which has failed through aseptic loosening
CT scans are indicated to evaluate bone stock and osteolysis and are useful prior to most RTKAs. Rotational position of components can also be verified.
Isotope imaging is often non-specific [41]. It is known to have limited value in the first year after joint replacement and thus can show positive results in asymptomatic patients [42, 43]. It fails to discriminate reliably between aseptic and septic pathologies, and as a result, leucocyte scintigraphy is recommended [43, 44]. Positron emission tomography (PET) is not deemed sensitive enough to diagnose aseptic loosening, as yet, and remains a non-essential imaging. The use of isotope imaging is as an adjunct rather than a primary diagnostic tool. Diagnostic arthroscopy is similar unless it is used as a means to biopsy the knee to exclude infection.
Previous and subsequent chapters in this book will discuss causes of failure such as infection, instability, malalignment, extensor mechanism loss and periprosthetic fracture. The topics of polyethylene wear and osteolysis and the use of cement as the principal causes of aseptic failure in TKA will be discussed here.
16.4 Polyethylene Wear
The femorotibial articulation of TKA is dissimilar to that of the highly conforming ball and socket articulation of total hip replacement in that with its sliding and rolling motions, TKA is inherently less conforming and creates shear and contact stresses not seen in the hip. Tensile stress near the edges of the polyethylene insert and subsurface shear stress along the articulating contact area produces pitting and delamination, which is specific to TKA. In addition the cyclic motion of the knee creates residual stresses that contribute to fatigue and failure [45]. Due to the low conformity and small contact area of the femoral component on the tibial polyethylene, peak contact stresses during activities of daily living may exceed the yield strength of polyethylene. These excessive forces may result in plastic deformation and consequently alter surface geometry and negatively affect alignment and stability. Altered load distribution between medial and lateral plateaus may then produce even more polyethylene wear.
The evolution of polyethylene used in TKA is an interesting one and is worth noting. Ultra-high molecular weight polyethylene (UHMPWE) has been successfully used in TKA since the late 1960s [46]. Initial UHMPWE was compression moulded followed by conventional gamma irradiation in air. Compression moulding enhanced wear properties and longevity [45, 47]. Two supposed further advances, the use of carbon fibre reinforcement (Poly II, Zimmer, Warsaw, In, USA) and highly crystalline UHMPWE (Hylamer, DePuy DuPont, Warsaw, IN, USA), were developed, but unfortunately these failed clinically despite preclinical testing demonstrating safety and effectiveness [48–50].
Cross-linked polyethylene (XLPE) is a modified form of UHMPWE that has higher cross-link density achieved by irradiation beyond that necessary for sterilization and thermal treatment [51]. Gamma or electron beam irradiation breaks intermolecular bonds and generates free radicals that promote cross-linking across multiple polymer chains and increases polyethylene density.
However, oxidation after gamma irradiation sterilization in air can reduce the mechanical properties by 20–90 % depending on the severity of the oxidation [52, 53]. The primary mechanism is thought to revolve around the residual free radicals introduced during the sterilization process. Conventional gamma-irradiated polyethylene is thought to contain higher residual levels and thus thought to be more vulnerable to oxidative degradation. In the 1990s, manufacturers began to gas sterilize, gamma sterilize in oxygen-free environments or use thermal treatments in an attempt to reduce residual free radicals [54–56]. Oxygen-free gamma sterilization reportedly increases the oxidative resistance, but some studies have reported that the oxidative process starts as soon as the packaging has been removed [49, 53, 57, 58]. Gas sterilization and thermal treatments have reported to yield undetectable levels of free radicals and have been thought to be oxidatively stable, but two recent studies reported that XLPE may still oxidize despite that these materials may have very low or undetectable levels of free radicals initially [57, 58]. It has been suggested that cyclical loading or lipid adsorption are potential mechanisms that alter the stability of XLPE [59].
Another approach is employing ethylene oxide to sterilize UHMPWE, which then remains non-highly cross-linked as a result but oxidatively stable during in vitro testing [55, 60–62]. The lack of cross-linking may confer worse resistance to wear, but this may be suitable for TKA where fatigue damage is predominant as opposed to total hip arthroplasty, where abrasive/adhesive wear predominates. XLPE with its decreased toughness, ductility and resistance to fatigue makes it more susceptible to failure under these conditions. Macdonald D et al. confirmed that in vivo oxidation was low of ethylene oxide sterilized polyethylene and that the polyethylene remained mechanically stable in the short term (10 years), but longer-term studies are required to ensure durability [58].
Sakellariou et al. conducted a systematic literature review to assess the potential advantages and cost-effectiveness of first-generation XLPE in TKA and concluded that because clinical studies directly comparing XLPE with conventional polyethylene were limited, the benefit of XLPE remains unknown [63]. Biomechanical in vitro testing has shown XLPE to be superior but this is yet to be demonstrated in long-term in vivo studies, and the methodology employed in both types of studies was heterogeneous. Furthermore, the advent of second-generation XLPE (vitamin E infused) has made progress in balancing the effects of abrasive and adhesive wear while maintaining resistance fatigue, but these purported advantages are yet to be seen in vivo and in the long term [64, 65]. The authors concluded that the extra cost of XLPE could not be justified on that basis.
16.5 Osteolysis
Osteolysis around the knee is well recognized [66–76]. The main causative factor is particulate debris which can originate from multiple sources around the TKA such as the tibial bearing surface, the tibial post, the backside of the polyethylene insert in modular TKA designs using tibial trays, the polyethylene patellar component, metallic debris from complete wear-through of polyethylene or cement debris from loosening of the implant [77–80]. It is not exclusive to cemented or cementless implants and the TKA may be stable or unstable [75, 81].
The cellular process of osteolysis is mediated by macrophages and giant cells which release several pro-inflammatory mediators such as interleukins which activate osteoclasts [82–84].
Osteolysis typically occurs in the cancellous bone of the distal femur and proximal tibia. A large amount of cancellous bone may be lost before it is apparent on a plain radiograph. Cortical bone loss is much less frequent but more obvious on X-ray. Furthermore, the bone that is lost may be obscured by the metallic implants and thus osteolysis around a TKA may be difficult to identify from plain radiographs (Fig. 16.2).
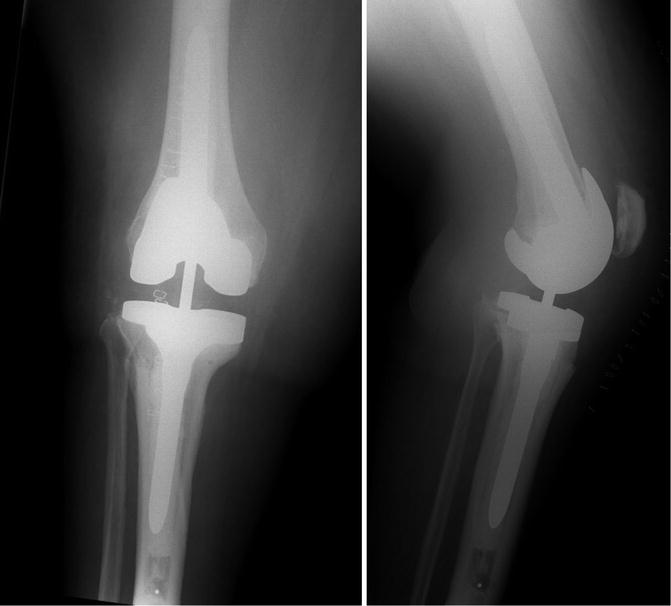
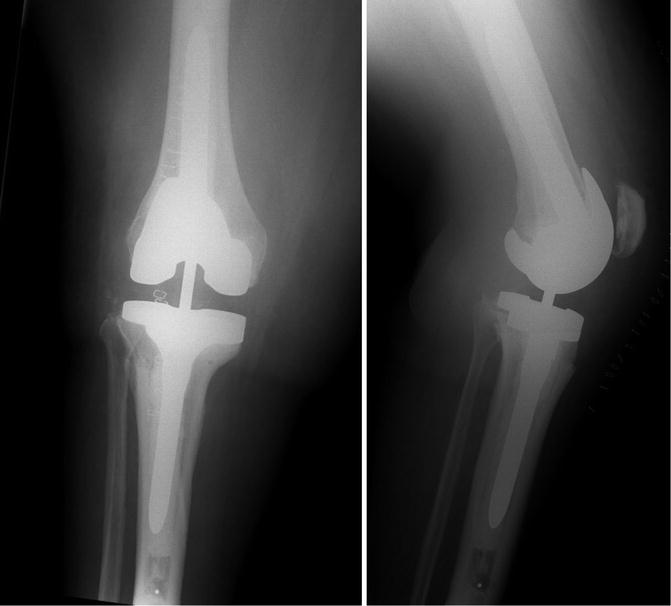
Fig. 16.2
The same knee of Fig. 16.1 following revision: AP (left) and lateral radiographs (right). Medial tibial bone loss has been reconstructed with a medial metallic augment
Serial radiographs help the surgeon spot osteolysis early, as does a high index of suspicion in the persistently painful TKA. Infection must be excluded, as this is also a cause of osteolysis. The development of an effusion some years after TKA may alert the surgeon to an osteolytic process that is aseptic and is caused by synovitis in reaction to particulate debris. Marked instability can cause excessive polyethylene wear, also causing osteolysis.
Certain areas of the TKA are prone to osteolysis such as the posterior condyles of the femoral component and in the region beneath the collateral ligaments. Tibial osteolysis is often peripheral or along access channels to the cancellous bone. Patellar osteolysis occurs around the margin of the implant along the implant-bone or bone-cement interface.
Factors that influence the rate of osteolysis include the conformity and kinematics of the TKA, quality of the locking mechanism between tibial tray and polyethylene insert for modular knees and the degree to which the TKA allows access of particles to the cancellous bone (such as uncemented designs and screw access channels). Young, active patients almost certainly are at higher risk of polyethylene wear and hence osteolysis and should be followed up for longer intervals.
16.5.1 Particle Size
The size of the polyethylene particle has been demonstrated to influence osteolysis; the smaller particles are thought to be more biologically active due to their ease of being phagocytosed [85]. Highly cross-linked polyethylene (XLPE) has been used in total hip arthroplasty for over 10 years and has proved in vivo to show less wear than conventional UHMPWE because it is thought to yield less wear particles [34, 86–90]. In vitro studies for TKA have demonstrated a reduction in wear of XLPE [91]. Iwakiri et al. compared XLPE and conventional polyethylene in small numbers retrospectively and showed a reduction in wear particles for XLPE, but this was not confirmed by Hinarejos et al. who found no significant reduction in wear particle concentration of synovial fluid from TKAs using XLPE when compared to conventional polyethylene [92, 93]. The size of the particle was not significantly different either, but their follow-up was only 1 year, and longer-term studies may demonstrate more significant advantages. Highly cross-linked polyethylene has also shown reduced fracture strength (Huot JC 2011), so coupled with the arguments above, its use is not widespread as yet [94, 95].
16.5.2 Tibial Component Choice
In TKA, surgeons have the choice of an all-polyethylene tibial component or a modular unit using a polyethylene liner (or bearing) mounted on a metal tray. Historically, the total condylar TKA used an all-polyethylene component for which excellent long-term survival rates have been reported [96, 97]. Metal-backed tibial designs originated when biomechanical studies demonstrated that they improved the distribution of forces between the implant and cement [98, 99].
The modularity that metal-backed tibial components allowed, as well as the possibilities for isolated liner exchange in revision procedures, fuelled their popularity. Disadvantages of metal-backed components include backside wear, osteolysis and micromotion [100–102]. Convincing arguments in favour of all-polyethylene components still exist. It is less expensive than its metal-backed counterpart, and studies have shown equal results in terms of function, range of motion, primary stability and long-term implant survival [103–108].
An analysis of over 27,000 TKAs by Gudnason et al. revealed that all-polyethylene tibial components had marginally better 10-year survival compared with metal-backed components, and this was attributed to an increased risk of infection with metal-backed designs [109]. This is a reproducible finding in the literature [110–114]. Some studies have shown a lower migration for all-polyethylene components using radiostereometric analysis, which is accurate for in vivo migration, which in turn is correlated to later aseptic loosening [115, 116]. There are subtle differences in the surgical technique which should not influence choice, but the surgeon of the future will undoubtedly have financial pressures to factor in to the decision-making process when choosing the tibial component for TKA; pleasingly modern polyethylene (oxygen-free gamma irradiated, thermal treated) has ensured that both components enjoy low wear rates and therefore associated osteolysis.
If one is faced with failure of a modular TKA as a result of wear, osteolysis and loosening and components are well fixed and well aligned, then isolated liner exchange is a valid treatment. Although there has been doubt cast on the benefits, studies against isolated exchange may have included diagnoses such as stiffness, instability and synovitis which have different re-revision rates compared to rates for osteolysis and wear, and quality of polyethylene has not been mentioned in the setting of RTKA [117–120]. In conclusion, isolated polyethylene exchange when components are well aligned, well fixed and without backside wear can be successfully used to treat patients undergoing revision for wear or osteolysis as long as the replacement polyethylene quality is good.
16.5.3 Cemented Versus Cementless TKA
Increasing numbers and a progressively younger patient population have stimulated the debate of cemented or cementless fixation in TKA. Young patients expect their activity levels to be higher post-operatively, and because of longer life expectancy, this patient group is more interested in 30-year survival rates of an implant than its 10- or 20-year survival rate. Therefore, preservation of the bone and good function and longevity are the established aims in TKA, and uncemented fixation is well tested and works well in several areas [121]. The bone-implant interface is physiologic and as a living interface it responds to stress in a physiologic way; thus, the attraction of cementless fixation is obvious. Despite success in total hip arthroplasty, uncemented fixation in TKA has not enjoyed similar results because several initial press-fit designs failed and many did not show superiority over cemented fixation [66, 122]. The meta-analysis by Wang et al. excluded the technical failures at an early stage as bias and, using comparative analysis of registers, demonstrated that uncemented TKA performed equally well with cemented TKA [123]. This contraindicated the findings from the study by Gandhi et al., but early technical failures were not excluded and follow-up was only at a mean of 2 years [124]. The other presumed advantage of cementless fixation is reduced operative time and several studies have shown that the absence of antibiotic impregnated cement does not influence the incidence of infection after TKA [125, 126]. The largest obstacle to comparison studies is the low numbers of uncemented cases performed worldwide but also the heterogeneity of the implants used for comparison within the uncemented group, as well as the great variation in surgical technique, ligament balancing and patellofemoral resurfacing options within study populations. On a background of multiple published case series of cemented TKA reporting survivorship for mechanical failure of 90–97 % at 10–15-year [96, 127–129] and between 85 and 98 % at 15–20-year follow-up [1, 2, 26, 130–134], as well as more recent concern that cementless fixation may be more sensitive to malalignment, especially on the tibial side since shear forces caused by varus or valgus tibial base plate positioning will alter the compressive forces distributed across the implant-bone interface, the enthusiasm for cementless TKA has always stuttered.
Cemented fixation in TKA is still the gold standard, evidenced by worldwide registry data that demonstrates more usage than cementless implants; this is despite the hydroxyapatite coating of components and newer developments such as trabecular metal which may infer favourable characteristics of bony ingrowth and maintenance of bone density [135, 136].
16.6 Conclusions
The burden of revision TKA is significant and is set to increase. Understanding why modern TKA fails is imperative if we are to effectively address failure but also to improve outcomes and satisfaction for our patients. Most causes of failure are, to some degree, under the surgeon’s control. Infection remains the first cause of failure to exclude. Aseptic failure of TKA encompasses several mechanisms of failure, some of which are intrinsically linked, namely, loosening, instability and malalignment. Our definitions of mechanisms of failure are becoming more descriptive which will aid in the extraction of meaningful data from large datasets and registries, but as surgeons we have a responsibility to report this data accurately so as to optimize its analysis. The successful development of more resistant biomaterials and evolutions in TKA design has helped reduce rates of polyethylene wear and associated osteolysis, but the work to provide a “lifetime” TKA goes on. Meticulous and accurate surgery to result in a balanced, well-fixed TKA must remain the surgeon’s primary aim in the quest to reduce failure.
References
1.
Ritter MA, Herbst SA, Keating EM, Faris PM, Meding JB (1994) Long-term survival analysis of a posterior cruciate-retaining total condylar total knee arthroplasty. Clin Orthop Relat Res 309:136–145PubMed
2.
Font-Rodriguez DE, Scuderi GR, Insall JN (1997) Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res 345:79–86PubMed
3.
Vessely MB, Whaley AL, Harmsen WS, Schleck CD, Berry DJ (2006) The Chitranjan Ranawat Award: long-term survivorship and failure modes of 1000 cemented condylar total knee arthroplasties. Clin Orthop Relat Res 452:28–34PubMed
4.
Weir DJ, Moran CG, Pinder IM (1996) Kinematic condylar total knee arthroplasty. 14-year survivorship analysis of 208 consecutive cases. J Bone Joint Surg Br 78:907–911PubMed
5.
Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR (2012) Total knee arthroplasty volume, utilization, and outcomes among medicare beneficiaries, 1991–2010. JAMA 308:1227–1236PubMedCentralPubMed
6.
Ravi B, Croxford R, Reichmann WM, Losina E, Katz JN, Hawker GA (2012) The changing demographics of total joint arthroplasty recipients in the United States and Ontario from 2001 to 2007. Best Pract Res Clin Rheumatol 26:637–647PubMed
7.
Falbrede I, Widmer M, Kurtz S, Schneidmuller D, Dudda M, Roder C (2011) Utilization rates of lower extremity prostheses in Germany and Switzerland: a comparison of the years 2005–2008. Orthopade 40:793–801PubMed
8.
Kurtz SM, Ong KL, Lau E, Bozic KJ (2014) Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am 96:624–630PubMed
9.
Abdel MP, Morrey ME, Jensen MR, Morrey BF (2011) Increased long-term survival of posterior cruciate-retaining versus posterior cruciate-stabilizing total knee replacements. J Bone Joint Surg Am 93:2072–2078PubMed
10.
Kurtz SM, Ong KL, Schmier J, Mowat F, Saleh K, Dybvik E et al (2007) Future clinical and economic impact of revision total hip and knee arthroplasty. J Bone Joint Surg Am 89(Suppl 3):144–151PubMed
11.
Robertsson O, Ranstam J, Sundberg M, W-Dahl A, Lidgren L (2014) The Swedish Knee Arthroplasty Register: a review. Bone Joint Res [Internet] 3:217–222
12.
Baker PN, Khaw FM, Kirk LMG, Esler CNA, Gregg PJ (2007) A randomised controlled trial of cemented versus cementless press-fit condylar total knee replacement: 15-year survival analysis. J Bone Joint Surg Br 89:1608–1614PubMed
13.
Robertsson O, Dunbar MJ, Knutson K, Lidgren L (2000) Past incidence and future demand for knee arthroplasty in Sweden: a report from the Swedish Knee Arthroplasty Register regarding the effect of past and future population changes on the number of arthroplasties performed. Acta Orthop Scand 71:376–380PubMed
14.
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63PubMedCentralPubMed
15.
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43PubMed
16.
Saleh KJ, Santos ER, Ghomrawi HM, Parvizi J, Mulhall KJ (2006) Socioeconomic issues and demographics of total knee arthroplasty revision. Clin Orthop Relat Res 446:15–21PubMed
17.
Baker P, Cowling P, Kurtz S, Jameson S, Gregg P, Deehan D (2012) Reason for revision influences early patient outcomes after aseptic knee revision. Clin Orthop Relat Res 470:2244–2252PubMedCentralPubMed
18.
Ong KL, Lau E, Suggs J, Kurtz SM, Manley MT (2010) Risk of subsequent revision after primary and revision total joint arthroplasty. Clin Orthop Relat Res 468:3070–3076PubMedCentralPubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








