Arthroscopy-Assisted Management or Open Reduction and Internal Fixation of Tibial Spine Fractures
Itai Gans
Theodore J. Ganley
DEFINITION
Tibial spine fractures are bony avulsions of the anterior cruciate ligament (ACL) from its attachment on the anteromedial portion of the intercondylar tibial eminence.26 Some authors consider them to be equivalent to the midsubstance ACL injuries seen in the adult population.
This injury most commonly occurs in the younger age group, particularly children aged 8 to 14 years with open growth plates, but can also occur in adults.
Tibial spine fractures have an incidence of 3 per 100,000 children each year.21
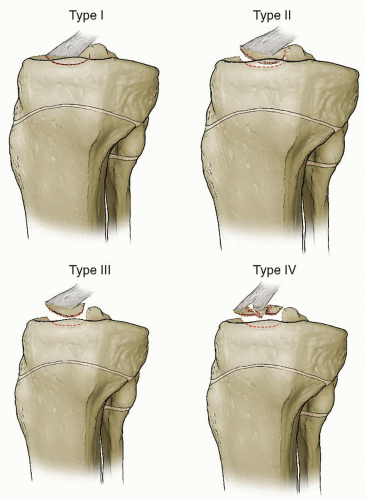
Meyers and McKeever16 classified tibial spine fractures into three types based on the degree of displacement. This classification was later modified by Zaricznyj27 to include a fourth type, signifying a comminuted fracture fragment (FIG 1):
Type I: nondisplaced fracture with minimal anterior margin elevation
Type II: posterior hinged fracture with partial displacement of the anterior margin (one-third to one-half of the tibial spine lifting from the epiphyseal bed)
Type III: completely displaced fracture fragment
Type IIIA: no rotational malalignment
Type IIIB: Fracture fragment has rotated such that the cartilaginous surface of the fracture fragment faces the raw bone of the epiphyseal bone bed.
Type IV: completely displaced and comminuted fracture fragment(s)
ANATOMY
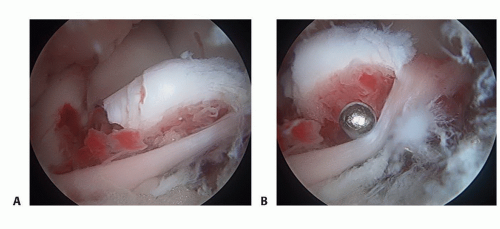
The tibial eminence is found lying in the intercondylar area of the tibia (FIG 2).
It is anatomically divided into four distinct regions: a medial and lateral triangular elevation (or medial and lateral tibial spines) and an anterior and posterior recess.
The ligamentous ends of the medial and lateral menisci insert into the intercondylar eminence.
The medial elevation provides the attachment for the fibers of the ACL with the anterior attachment of the medial meniscus just anterior to the ACL insertion and the anterior attachment of the lateral meniscus just posterior to the ACL insertion.
There are no structures that attach to the lateral portion of the eminence.
The tibial eminence also serves as an insertion for the posterior cruciate ligament (PCL); the fibers of the PCL typically arise from the posterior portion of the intercondylar eminence.16
In the younger child, the majority of the anterior portion of the tibial eminence is cartilaginous.16
PATHOGENESIS
Avulsions of the tibial spine are usually traumatic in nature. This injury is more common in children, particularly those with incomplete ossification and open growth plates.
The usual mechanism of injury is a hyperextension injury, with or without a forced valgus or external rotational force about the knee.17 These fractures may also occur following a direct blow to the distal femur when the knee is flexed.
FIG 2 • Axial view of the tibial plateau. A. The intercondylar eminence lies between the medial and lateral condyles. B. The medial portion serves as the attachment of the ACL.
The injury occurs because of a tensile load placed on the ACL. The ligamentous ACL is much stronger in resisting tensile forces than the immature, incompletely ossified and primarily cartilaginous, osteochondral surface; this often results in failure and avulsion of the osteochondral attachment of the ACL.
Before bone failure, in situ stretch injury of the ACL may occur18 and may result in clinical laxity despite adequate reduction of the fracture fragment.10,22
Different loading mechanisms are likewise implicated in the development of the injury. Experimental models have shown that rapid loading rates result in midsubstance ACL tears, whereas gradual loading results in tibial spine avulsion fractures.18,26
The inherent anatomy of the knee has likewise been implicated. Kocher and colleagues11 compared 25 skeletally immature knees with tibial spine fractures against 25 age-matched skeletally immature knees with midsubstance ACL tears and found a narrower notch width (intercondylar notch) in individuals who had sustained the midsubstance ACL tears.
PATIENT HISTORY AND PHYSICAL FINDINGS
Fractures of the tibial spine are usually precipitated by an acute traumatic event. The clinical presentation usually coincides with the severity of injury.
Usually, a patient with a tibial spine injury will have a history of trauma or sports-related injury; the most common mechanism is historically a fall from a bicycle. With increasing numbers of children playing in competitive athletics, sports-related tibial spine fractures have been reported with increasing frequency. High-velocity trauma may also cause tibial spine injuries.
The patient will usually present with a painful swollen knee. Swelling is secondary to hemarthrosis from the intraarticular knee injury.
Gentle palpation and examination of the knee are undertaken. Most patients have some degree of swelling due to hemarthrosis secondary to the intra-articular fracture. Other superficial injuries are related to the degree and nature of the traumatic event.
Knee joint laxity is often present, and patients typically have an inability to bear weight on the affected extremity.
It is important to note that patients will typically only have positive anterior drawer tests or Lachman tests with complete fractures (ie, type III and type IV) of the tibial spine. However, due to stretch of the ACL complex during injury, subclinical laxity may be noticed in incomplete fractures.
A positive anterior drawer test indicates knee joint laxity. However, this is not as sensitive as the Lachman test in assessing for ACL deficiency.
A positive result on the Lachman test indicates deficiency of the ACL complex. The test has greater sensitivity and specificity for ACL tears.
In the presence of a deficient ACL complex, during the pivot shift test (usually done intraoperatively when the patient is anesthetized), the femur falls posteriorly in relation to the tibia as the leg is raised and rotated internally. The valgus force applied to the leg along with slight flexion of the knee results in the pivot shift phenomenon. The intact iliotibial band reduces the femur when the knee is brought into 20 to 30 degrees of flexion.
The knee should also be carefully examined for any concomitant injury including meniscal and collateral ligament injury.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Good imaging is crucial in the assessment and management of tibial spine fractures as appropriate classification of the fracture pattern dictates treatment (see section on Nonoperative Management).
Standard anteroposterior (AP) and lateral views of the knee are usually adequate in making the diagnosis. These views help to define and identify the extent of bony injury.
A precise lateral radiograph is necessary as this is the best view to accurately assess fracture classification and fracture fragment position.
In lesions that are predominantly cartilaginous, radiographs may sometimes detect a small piece or a fleck of avulsed bone, which may be indicative of the avulsed osteochondral fragment, and underestimate the true size of the fracture fragment (FIG 4).
Magnetic resonance imaging (MRI) is a good imaging modality for suspected tibial spine injuries, especially in the immature knee, where the tibial spine is predominantly cartilaginous and radiation exposure is of concern. MRI can help differentiate between a midsubstance ACL injury and a true avulsion fracture of the tibial spine and allow for classification of the fracture pattern. MRI can also allow assessment for fracture displacement and help to detect concomitant injuries around the knee joint.9
Computed tomography is helpful in the older age group and in cases of severe trauma, where the fracture configuration may be severely comminuted and there is no suspicion of concomitant meniscal or collateral ligament injury.
DIFFERENTIAL DIAGNOSIS
ACL tear
Osteochondral lesion or osteochondral fracture
Tibial plateau fracture
Other ligamentous or meniscal injuries about the knee
NONOPERATIVE MANAGEMENT
Nonoperative management is reserved for nondisplaced type I fractures and reducible type II fractures.
Type II fractures may be reduced by first aspirating the hematoma and injecting a local anesthetic agent into the joint space.
The knee is extended in an attempt to reduce the fracture fragment. The mechanism of reduction is through direct pressure exerted by the lateral femoral condyle.
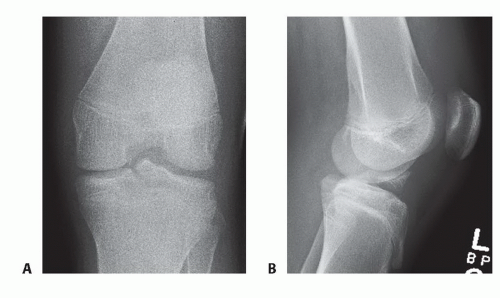
FIG 4 • AP (A) and lateral (B) radiographs of the knee showing a displaced tibial spine fracture (type III).
This maneuver may be effective for lesions that are large enough to include part of the tibial plateau.
In small lesions, or in lesions where the intermeniscal ligament is interposed between fracture fragments, the maneuver may not afford adequate reduction.
The reduction is assessed with radiographs, and the knee is immobilized.
A hinged knee brace or long-leg cast is placed to immobilize the leg and maintain reduction.
There has been controversy about the optimal position for cast placement.
Previous authors have recommended varying knee positions, ranging from 0 to 40 degrees of flexion.3,5,17 The arguments in favor of flexing the knee relate to the relative relaxation of the ACL in flexion.15
Immobilization in hyperextension is not recommended due to patient discomfort and the risk of putting the popliteal artery under tension, potentially causing the development of a compartment syndrome.
The authors recommend immobilization in a hinged knee brace in full extension for 4 to 6 weeks.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree