CHAPTER 21 Arthroscopic Wrist Ganglionectomy
Rationale and Basic Science
Dorsal wrist ganglions are the most common type of soft–tissue swellings that present around the wrist. They usually originate from the dorsal portion of the scapholunate ligament, at or just distal to the dorsal folds of the radiocarpal capsule.1 The dorsal wrist ganglion originates from the scapholunate joint. The cyst pedicle lies at the junction of the dorsal capsule and the distal–most part of the dorsal scapholunate interosseous ligament. From here, the ganglion swells into a sac lying along the dorsal capsule—from where it protrudes as a clinically obvious swelling. The intracapsular portion of the ganglion overlies the scapholunate joint, but the large extra–articular fundus of the cyst may vary in location (although it still remains in close vicinity of the joint).
Wrist arthroscopy offers an excellent view of the wrist joint, and with modern mechanized shavers intra–articular pathology can be effectively debrided. In the case of a ganglion, the intra–articular portion is easy to see because it lies against the dorsal capsule. The pedicle of the ganglion at the scapholunate ligament can be visualized in the majority of cases, and can be resected effectively along with the intra–articular portion with minimal surgical incisions. This may reduce the incidence of recurrence after surgery. In addition, arthroscopy allows a thorough visual examination and palpation by probe of the radiocarpal and midcarpal joints to exclude other sources of wrist pain. The use of wrist arthroscopy to effectively treat dorsal wrist ganglia is not new and was first proposed by Osterman in 1995.2
Clinical Features and Indications
Most ganglia present in females in the second, third, or fourth decades of life. Spontaneous resolution is common but can take several years, with 50% of untreated patients “ganglion free” when assessed at six years.3
The most common presenting complaint is the cosmetic concern relating to a lump present on the back of the wrist. The other less common complaints are discomfort localized to the area of the swelling or fear of possible malignancy. Although the diagnosis is usually quite obvious in the majority of cases, other causes of wrist pain must be excluded by a thorough clinical examination and routine radiography. The ganglion is a soft cystic swelling that has no inflammatory signs. Transillumination by a penlight and fluctuation are two key clinical signs that demonstrate the clear fluid nature of the lump and exclude other soft–tissue tumors. If the patient seeks absolute confirmation, ultrasound examination is diagnostic. MR imaging is more expensive, but is indicated if Kienbock’s disease is to be excluded.
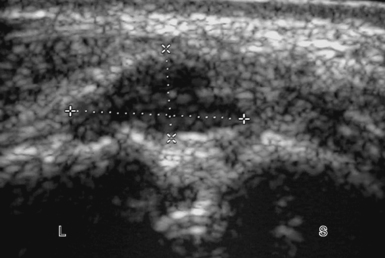
The patient with an occult wrist ganglion will complain of wrist discomfort over the area of the scapholunate joint and may or may not notice intermittent swelling in the area. As the swelling is not visible clinically, confirmation by MR imaging or ultrasound is mandatory. Ultrasound is the most cost effective and will demonstrate the ganglion as a hypoechoic mass overlying the scapholunate joint and deep to the wrist capsule (Figure 21.1).4
Management options include reassurance that the swelling is harmless, and spontaneous resolution is possible if one is prepared to wait for a reasonable length of time. This holds true especially in the pediatric population, where cysts around the wrist are likely to resolve spontaneously in up to 80% of cases.5 A brief period of rest in a splint may help to reduce pain. Needle aspiration does provide immediate symptom relief, with resolution of the swelling, but the reported recurrence rate is about 60%.6,7 The injection of steroid after aspiration does not seem to affect the high recurrence rates, and with risk of subcutaneous atrophy and skin depigmentation is not routinely recommended.8
Surgical Technique
Contrary to traditional wrist arthroscopy that commences on the radial side with initial visualization through the 3–4 portal, for ganglionectomy the author prefers to start from the ulnar side of the wrist from the 6–R portal for the following reasons. Introduction of the scope through the 3–4 portal may actually enter through the ganglion, causing it to rupture and making it less distinct. The intra–articular portion of the ganglion impairs visibility and examination of the joint is not possible. Furthermore, the 3–4 portal will be used for instrumentation to debride the ganglion. The author therefore recommends using the 3–4 portal for diagnostic arthroscopy only after the ganglion has been debrided.
An 18–gauge needle is inserted into the 6–R portal first to localize the level of the ulnocarpal articulation and to ensure that the triangular fibrocartilagenous disc is not violated. A 4–mm transverse incision is made in the skin and a small hemostat is introduced into the joint and spread gently. The blunt trocar and cannula are inserted and then the trocar is exchanged for the scope (Figure 21.2).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree