CHAPTER 28 Arthroscopic Treatment of Trapeziometacarpal Disease
Introduction
There are myriad techniques for open treatment of trapeziometacarpal (TM) osteoarthritis (OA). These have included partial and complete trapezium excision with or without ligament reconstruction and with or without interposition of tendon, fascia lata, gortex, artelon, or silicone. Instances of reactive synovitis have tempered the enthusiasm for interposition of foreign substances. Recent reports in the North American literature1,2 of good results following complete trapeziectomy with hematoma arthroplasty have rejuvenated interest in this technique, which has been commonplace in Europe for some time.3 Arthroscopic techniques for evaluating and treating trapeziometacarpal disease surfaced in 1994.4,5
The question of whether to interpose tendon is still a matter of debate. Proponents of the hematoma arthroplasty cite data that demonstrates no advantages in terms of pinch strength, thumb motion, and pain relief following an arthroplasty with tendon interposition compared to an isolated trapeziectomy.6 The hematoma arthroplasty relies on the development of a stable pseudarthrosis that develops from the ingrowth of fibrous tissue, which replaces the blood that immediately fills the cavity following an excision of the trapezium. Pinning the thumb metacarpal base to the index for five to six weeks is integral to the procedure, but augmentation or reconstruction of the TM joint capsule is not. The good results that have been obtained with open trapeziectomy have provided the impetus for the development of arthroscopic techniques.
The scaphotrapezotrapezoidal (STT) joint is also commonly affected by OA. The STT fusion popularized by Watson has largely fallen out of favor. As an alternative to this, distal scaphoid resection has been shown to provide good symptomatic relief.7
Indications
Littler and Eaton described a radiographic staging classification of TM OA.8 Stage I comprises normal articular surfaces without joint space narrowing or sclerosis. There is less than 1/3 subluxation of the metacarpal base. Stage II reveals mild joint space narrowing, mild sclerosis, or osteophytes < 2 mm in diameter. Instability is evident on stress views, with > 1/3 subluxation. The STT joint is normal. In stage III there is significant joint space narrowing, subchondral sclerosis, and peripheral osteophytes > 2 mm in diameter (but a normal STT joint).
In stage IV there is pantrapezial OA with narrowing, sclerosis, and osteophytes involving both the TM and STT joints. Burton modified this classification by incorporating the clinical findings.9 Stage I includes ligamentous laxity and pain with forceful and/or repetitive pinching. The joint is hypermobile, which can be seen on stress views (but X-rays are normal). In stage II, crepitus and instability can be demonstrated clinically—whereas X-rays reveal a loss of the joint space. Stages III and IV are similar to Eaton’s classification. Patients in stage I (and possibly early stage II) are appropriate candidates for arthroscopic debridement and capsular shrinkage.10
Badia proposed a more specific classification based on arthroscopic changes.11 Stage I included intact articular cartilage, stage II included eburnation on the ulnar 1/3 of the metacarpal base and central trapezium, stage III comprised widespread full-thickness cartilage loss on both surfaces. Based on intraoperative findings, he recommended debridement for stage I, with thermal capsulorrhaphy in the presence of dorsal subluxation, extension/abduction osteotomy of the metacarpal base ∀ thermal shrinkage for stage II, and an arthroscopic interposition arthroplasty for stage III. He recommended an open arthroplasty in the presence of associated severe STT joint OA.
As a general rule, any patient who is an appropriate candidate for a hemiresection arthroplasty of the TM joint would also be suitable for an arthroscopic hemitrapeziectomy. This would typically include patients in stage II and stage III with unremitting pain despite appropriate conservative measures. This form of treatment does not preclude an open trapeziectomy and/or ligament reconstruction at a later date as a salvage procedure for failed arthroscopic surgery. The presence of Eaton stage IV disease is a relative contraindication to a hemitrapeziectomy, although an arthroscopic hemitrapeziectomy combined with an arthroscopic debridement or limited resection of the distal scaphoid is an option. The rationale for this would be similar to that of the double interposition arthroplasty described by Eaton and Barron, in which the TM and STT joints are resurfaced while the body of the trapezium is left intact in order to prevent a loss of height of the thumb ray.12 Failing this, a complete arthroscopic (or open) trapeziectomy would be necessary.
Precautions
Any significant lateral subluxation of the thumb metacarpal base will not be corrected without some type of ligament reconstruction or capsular shrinkage, and may compromise the long-term result if not corrected. Metacarpophalangeal (MP) joint hyperextension must be treated concomitantly. Otherwise, the reconstruction may ultimately fail. MP hyperextension of 10 to 20 degrees may be treated by percutaneous fixation of the MP joint in flexion for four to six weeks, and/or transfer of the extensor pollicis brevis to the thumb metacarpal base. MP hyperextension of 20 to 40 degrees can be addressed with a volar plate advancement13 or capsulodesis.14 A sesamoidesis MP hyperextension > 40 degrees is typically controlled by an MP fusion.
Contraindications
This would include any general contraindication to thumb arthroscopy, including distortion of the anatomy due to swelling, unstable or friable skin (which would preclude the use of traction), and recent infection. Ehler Danlos syndrome is a relative contraindication for this procedure, although a successful arthroscopic tendon arthroplasty has been reported.15
Surgical Technique
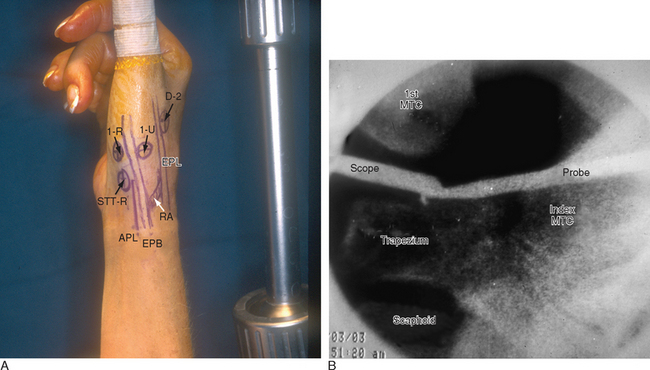
The patient is positioned supine on the operating table, with the arm extended on a hand table. The thumb is suspended by Chinese finger traps with 5 pounds of countertraction, which forces the wrist into ulnar deviation. The relevant landmarks are outlined, including the proximal and dorsal edge of the thumb metacarpal base, the tendons of the abductor pollicis longus (APL), the extensor pollicis longus (EPL), and the radial artery in the snuffbox (Figure 28.1). The procedure is performed with a tourniquet elevated to 250 mmHg. Saline inflow irrigation is provided through the arthroscope and a small- joint pump or pressure bag.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree