Fig. 6.1
AP and lateral X-ray views of a 12 years old girl with a type IIIA tibial spine avulsion. AP and lateral X-rays after arthroscopic reduction and internal fixation with wire (postoperative and 6 months follow-up)
The Schatzker classification of tibial plateau fractures [6]:
Type I is a split fracture of the lateral condyle usually as a result of valgus and axial force. This pattern usually appears in young patients so there is no compression of the fractured fragment because of the strong cancelous bone.
Type II is a split-compression fracture of the lateral condyle, also a result of combined valgus-axial forces but the more porotic bone of older patients produces a collapse of the cancelous structure under the articular surface.
Type III is a pure compression fracture of the lateral condyle, it can be localized anywhere on the articular surface, the result of an axial force.
Type IV is a fracture of the medial plateau, with a of split or split-compression pattern. It is the result of either a varus or an axial compression force, usually greater than the force that produces a lateral condyle fracture.
Type V is a fracture of both condyles, split and split-compression. An axial force produces it with the knee in full extension.
Type VI is a complex bicondylar fracture with diaphyseal extension. The result of high-energy trauma, usually the fragments are depressed and impacted, separated from the diaphysis.
In the AO/OTA classification, the proximal tibia is denoted as segment 43 and is divided into three main categories. Type A fractures are extraarticular. Type B fractures are partial articular and are subdivided into three main categories: B1 are pure splits, B2 are pure depression and B3 are split-depression. Type C fractures are complete articular fractures and are also subdivided into three subtypes: Type C1 is articular and metaphyseal simple, Type C2 is articular simple, Type C2 is articular simple and metaphyseal multifragmentary and Type C3 is articular multifragmentary. The AO classification separates fractures of the tibial plateau based on their articular involvement in:
These classification systems were all initially based on the radiographic appearance of the fracture and are all subject to intra- and interobserver variability. Traditionally, tibial plateau fractures are classified based on plain anteroposterior (AP) and lateral plain radiographs but it is well known that several fracture patterns exist that are not well represented in existing two-dimensional (2D) fracture classifications. For example, recognition of a posteromedial fragment is important in preoperative planning as it may require an additional surgical approach and/or supplementary fixation methods. It is well recognized that posteromedial shear fractures, as well as fractures in the coronal plane, are easily overlooked on plain AP radiographs.
As CT scanning provides better imaging of bone tissue it should make for a more accurate assessment of the tibial plateau fractures. However, there is conflicting evidence in literature regarding the improvement in the intra- and interobserver variability in classifying tibial plateau fractures using both plain radiographs and CT scanning. Intra- and inter-observer reliability and/or diagnostic accuracy of the most common classification systems for tibial plateau fractures – the AO and Schatzker classifications – are widely studied in orthopedic literature based on plain radiographs [7]. Better, more detailed, imaging form CT scans means that fracture patterns that are not visible on plain X-Rays can be visualized and assessed. This is especially true for fracture patterns that are not very well represented on traditional biplane imaging, such as pure depression patterns and posteromedial shear fractures. Recently, Gardner et al. disagreed that Schatzker III fractures exist, stating that a shear pattern existed in all of the cases that they have investigated [8]. Although Schatzker III fractures are cited to represent up to 30 % of the fracture patterns [5, 9, 10], we found a much lower rate of Schatzker III fractures in our practice of around 7 %. CT and MRI imaging are more accurate than plain radiography for classification of tibial plateau fractures, and the use of cross-sectional imaging can improve surgical planning. MRI is especially useful for determining the association and extent of associated lesions (collateral ligaments, menisci, anterior cruciate ligament, posterior cruciate ligament). While its value cannot be undermined, its costs prohibit the routine use of MRI in fractures of the tibial plateau. Kode et al. compared MR imaging with CT for evaluation of tibial plateau fractures and found that MR imaging was equivalent or better in determining the degree of fracture displacement [11]. In many cases, CT findings mirror those of conventional radiography.
Classically the intraoperative evaluation of the articular surface was be done under direct visualization, something that can be difficult in certain combinations of fracture patterns and approaches (especially a lateral approach for a fracture with a medial component), but some authors favor the use of arthroscopy for its lower rate of infectious complications [12, 13]. Taking all this into the account we agree that the therapeutic indication for arthroscopically assisted fixation of proximal tibia fractures is limited to simple split fractures, split depression and pure depression fractures (Schatzker type I, II, III and simple type IV) as well as avulsion fractures of the ACL insertion and osteochondral fractures this being supported by the opinion of other authors [6, 14],
The use of arthroscopy is according to Musahl et al. better suited for Schatzker III pure depression fractures, one of the uncommon forms of tibial plateau fractures, but while this obviously varies from surgeon to surgeon not all tibial plateau fractures is amenable to arthroscopic aided reduction and fixation techniques. The arthroscopic treatment of proximal tibial fractures is reserved to those fracture patterns where the direct visualization of the fracture can add a definite value to the fracture reduction process. Another factor to be accounted for is the positive liquid pressure that is necessary to perform a knee arthroscopy. It should not hinder the fracture reduction process nor create extensive swelling in an already swollen knee and further increasing the risk for compartment syndrome. Also there is at least one case cited in literature where embolism form arthroscopy fluid occurred in a patient with a tibial plateau fracture that was treated by arthroscopy [15]. Other early complications for ARIF techniques such as DVT and knee effusions maintain the same trend being fewer and less serious than those for standard ORIF techniques but they may have the selection bias of simpler cases fracture patterns that receive the arthroscopic treatment in their favor [16]. Arthroscopy with an articular fracture of the tibial plateau is a technically challenging surgery for the less experienced surgeon but it will also be of great help in identifying and treating associated meniscal injuries or other articular lesions. A fluid pump will control bleeding but low pressure should be maintained to decrease the risks associated with excessive fluid extravasation [17].
Another type of intraarticular injuries that can be addressed arthroscopically is the fractures of the tibial eminence that are synonymous with intercondylar eminence avulsion fractures. Displaced avulsions of the tibial spine are equivalent to ruptures of the anterior cruciate ligament. They present to general orthopedists as well as a wide variety of orthopedic subspecialty surgeons including sports medicine and pediatrics. Restoration of normal knee kinematics is dependent on anatomic reduction and fixation of the avulsed fragment. Because this injury is typically sustained by the skeletally immature patient, epiphyseal fixation is ideal to avoid physeal injury, which can lead to angular limb deformity [18]. Lafrance et al. consider that although most fractures heal successfully, residual laxity usually persists because of prefracture anterior cruciate ligament midsubstance attenuation. This does not typically manifest in subjective instability, and reconstruction of the anterior cruciate ligament is rarely required [19].
Prince et al. found that ACL injuries in skeletally immature patients are seen more often in boys. In addition, tibial avulsion fractures and partial tears are more common in younger, less rigid skeletons that can absorb the forces of trauma. As children mature, complete ACL tears and associated injuries occur in frequencies approaching those patterns seen in adults [20].
Sometimes when close reduction of the fragment is attempted this is obtained incompletely due to soft tissue interposition. Kocher et al. found that 65 % of type III fractures and 26 % of type II fractures had entrapment of the anterior horn of the meniscus, most commonly medial [21]. Other authors have confirmed this as well, particularly in type III fractures. This is why most authors such as Accousti et al. consider the treatment algorithm for tibial eminence fracture management with regard to displaced and irreducible fractures to require arthroscopic or open treatment, based on surgeon preference [22, 23]. Objective sagittal plane laxity does not translate into long-term clinical or subjective instability. However, every effort should be made to obtain the best possible reduction with stable fixation, when needed, to maximize function.
The classification system of Meyers and McKeever (Fig. 6.2) is the current standard used to classify these fractures and to guide treatment [24]. It is based on the degree of displacement, mainly on the lateral x-ray. Zaricznyj modified this classification [25] to include a fourth type – comminuted fractures of the tibial spine, which applies mostly to adults:
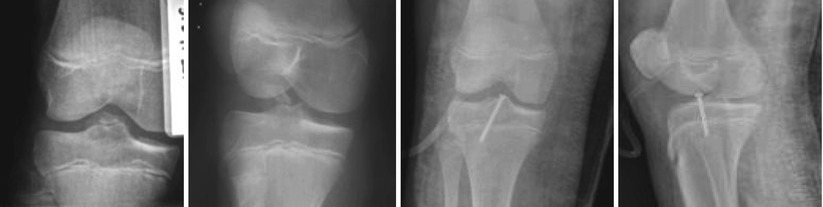
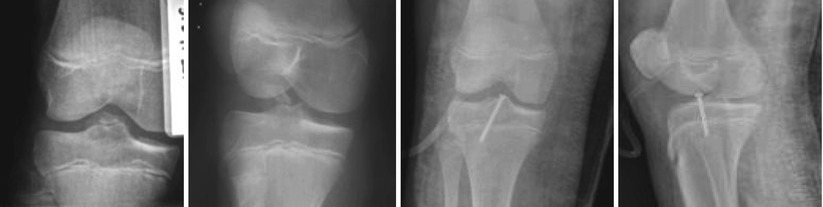
Fig. 6.2
AP and lateral emergency X-ray views of a 11 years old girl with a type IIIA tibial spine avulsion. AP and lateral X-rays after arthroscopic reduction and internal fixation with a cannulated screw
The Mayer and Mc Keevers classification, modified by Zariczynj:
Type I: minimal displacement of the tibial spine fragment
Type II: displacement of the anterior third to half of the avulsed fragment, which is lifted upward but remains hinged on its posterior border
Type III: complete separation of the avulsed fragment from the proximal tibial epiphysis, usually associated with upward displacement and rotation
Type III A involves only ACL insertion
Type III B involves entire intercondylar eminence.
Type IV comminuted fractures of tibial spine.
Song et al. reviewed their cohort of patients with displaced tibial spine avulsions and identified eight cases of type II and ten of type III in children and two cases of type II, 15 of type III, and five of type IV in adults. A higher incidence of type IV fractures was encountered in the adult group. Adults had higher incidences of accompanied meniscal injuries and type IV fractures than children. Significant differences were found in mean Lysholm scores, 99.3 points in children and 89.5 in adults. However, no significant differences were found between adults and children in terms of range of motion, the Lachman test and the Pivot-shift test, and instrumented anterior laxity. Lysholm scores of ACL avulsion fractures were better in children than in adults. Possible causes of these results are higher incidences of accompanying meniscal injury and type IV fracture in adults. However, no intergroup differences were found in terms of stabilities [26].
Arthroscopic treatment is advocated by the majority of authors as the best current option [27–31]. This allows for a complete evaluation and treatment of associated lesions, optimal reduction with removal of any possible soft tissue entrapment, accurate estimate of the size of the fragment (the chondral part is not visualized on x-rays and thus the fragment is usually undersized) and adequate internal fixation using suture, wire or screws. Reynders et al. presented a series of 26 cases of displaced fractures of the intercondylar eminence of the tibia treated with an arthroscopically placed, intrafocal screw with washer. Sixteen patients had a type II tibial eminence fracture according to Meyers and McKeever (mean age, 15 years; male/female ratio, 11:5) and ten patients had a type III tibia eminence fracture (mean age, 17 years; male/female ratio, 1:1). They encountered neither stiffness nor iatrogenic chondral abrasion. All but three patients with type II had some degree of residual laxity, without apparent impact on the clinical result. In four patients with a type III lesion, a residual laxity without functional deficit was noticed. In two cases with a type III lesion, a reconstruction of the anterior cruciate ligament was necessary 3 years after trauma. In four patients with a type III fracture, the fragment remained elevated, with minor impairment of the mobility (extension lag). No mechanical failure or infection was seen in this series. The authors found the intrafocal screw fixation for displaced fracture of the intercondylar eminence to be a reliable and safe technique, although complete restoration of the anteroposterior knee stability was seldom seen [32]. Lubowitz et al. recommend arthroscopic reduction and internal fixation for all displaced (type III) fractures and believe this should also be considered for all cases of displaced type II fractures. Fractures without displacement after closed reduction require careful evaluation to rule out meniscal entrapment. Subjective results are found to be uniformly excellent, despite reports of objective anteroposterior laxity [29].
Kocher et al. reviewed their results in six patients at minimal 2-year follow-up. They found mean postoperative Lysholm and Tegner scores of 99.5 and 8.7, respectively. One patient had a grade A Lachman (normal) test, three had grade B (nearly normal), and two had grade C (abnormal). Instrumented knee laxity showed side-to-side differences of greater than 3 mm in 4 of 6 patients [33].
In contrast, Wilfinger et al. performed a retrospective clinical analysis in a single department and identified 43 patients. Twenty-three were female and 20 male. The mean age at trauma was 11.5 years (6–16 years). Only 1 patient required a change of therapy and needed open reduction. Thirty-eight patients were available for follow-up at an interval of 1–7.5 years after trauma (mean 3.5 years). None of the patients reported pain, swelling, disability or giving-way, or was handicapped in their daily life. Of 26 magnetic resonance imaging examinations, we found a missing anterior cruciate ligament in 1 and a partial rupture in another patient. Based on these results, the authors recommend nonoperative management as the primary treatment for tibial spine fractures in children [34].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








