Loss of motion is a common sequela of elbow trauma or the natural progression of nontraumatic conditions of the elbow, significantly impairing function of the upper extremity and hindering performance of activities of daily living (ADLs).
A functional arc of 100 degrees (30 to 130 degrees) in flexion and extension, along with 100 degrees in pronation and supination (50 degrees each), is required for most ADLs.19
Neighboring joints offer little compensatory function, making elbow stiffness poorly tolerated.
Stiffness may be due to intrinsic (intra-articular) or extrinsic (extra-articular) causes (Table 1) or a combination of both.6,14
Posttraumatic stiffness is most common, but osteoarthritis, inflammatory conditions, systemic injuries (head trauma), and neurologic disorders may also cause elbow joint contractures.
Loss of extension is most common, although loss of flexion is more poorly tolerated due to an inability to reach the face for eating or grooming.18
The key to treatment is identifying and correcting the functional and occupational impairment; decisions should not be based solely on the absolute loss of motion of the elbow.11
Arthroscopic treatment of elbow stiffness is intended to restore motion, function, and relieve pain when present.23
Table 1 Classification of Elbow Stiffness Based on Location of Structure in Relation to the Elbow Joint
Type
Location
Description
Intrinsic
Within the elbow joint
Articular incongruity after fracture, degenerative changes and loss of cartilage, intra-articular adhesions, loose bodies, synovitis, infection
Extrinsic
Tissues immediately adjacent
Soft tissue and capsular contracture, muscle fibrosis (brachialis especially), collateral ligament stiffness, to the elbow joint heterotopic ossification, skin contractures
Peripheral
Factors anatomically separate from the elbow
Stroke, neurologic problems, peripheral nerve disorder, head injury, cerebral palsy
From Jupiter JB, O’Driscoll SW, Cohen MS. The assessment and management of the stiff elbow. AAOS Instr Course Lect 2003;52:93-111.
Arthroscopic treatments may range from capsular release alone to osteocapsular arthroplasty, including the removal of loose bodies, osteophytes, and capsulectomy.22
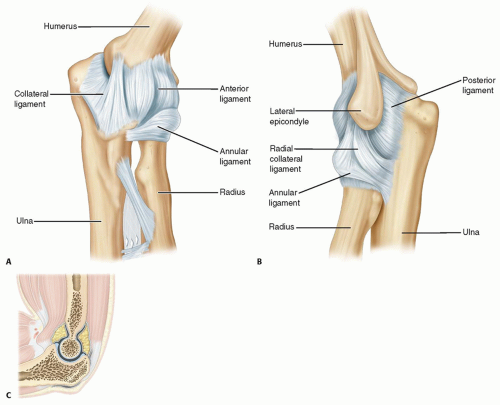
The elbow is anatomically predisposed to stiffness by virtue of the close relationship of the capsule to the surrounding ligaments and muscles, along with the presence of three joints within a synovial-lined joint cavity—(a hinge ginglymus) ulnohumeral articulation and rotatory (trochoid) radiocapitellar and radioulnar joints.11
The anterior elbow capsule attaches proximally above the coronoid fossa and distally extends to the coronoid medially and annular ligament laterally. The posterior capsule starts proximally just above the olecranon fossa and inserts at the articular margin of the sigmoid notch and annular ligament (FIG 1).
The anterior capsule is taut in extension and lax in flexion, with strength derived from the cruciate orientation of its fibers.
The greatest capsular capacity is at 80 degrees flexion.9,24 The normal capacity of 25 mL can be reduced to as little as 6 mL in a contracted state.9,24
The joint capsule is innervated by branches from all the major nerves crossing the joint along with the musculocutaneous nerve.16
The cubital tunnel, which houses the ulnar nerve at the elbow, becomes compressed in flexion (due to stretching of the retinaculum between the olecranon and medial epicondyle) and loosens in extension.
Flexion contractures may adversely compress the ulnar nerve, leading to ulnar neuropathy (FIG 2).
O’Driscoll23 describes four stages of posttraumatic elbow stiffness:
Bleeding: minutes to hours
Edema: hours to days. Both bleeding and edema cause swelling within the joint and surrounding tissues, and the capsule become biomechanically less compliant. Early elbow range of motion through an entire range during stages 1 and 2 can help prevent stiffness.
Granulation tissue: days to weeks. Splints can be used to regain range of motion.
Fibrosis: Maturation of the granulation tissue further decreases compliance. More aggressive splinting is necessary, along with possible surgical management.
The posttraumatic joint capsule is sensitive to contracture, secondary to an increase in disorganized collagen fiber deposition at the cellular level, resulting in thickening that translates into loss of flexibility and joint volume.9,16,23
The reasons for altered capsular properties are multifactorial and not completely known.
Myofibroblasts, cells that enhance collagen production and tissue contraction, increase in number in the posttraumatic anterior capsule.10
Collagen formation, cross-linking, and hypertrophy increase while water and proteoglycan content decrease in the contracted elbow tissue.1
Increased matrix metalloproteinase activity and collagen disorganization have also been described in the contracted capsular tissue.10
Growth factors and other cellular mechanisms may be involved. This is highly variable among individuals.17
Heterotopic ossification may also occur in conjunction with capsular thickening and act as a bony block to motion. Patients most at risk are those with combined head and elbow trauma, burn patients, and those who have undergone surgical approaches to the elbow, all of which are believed to incite a complex inflammatory chain that leads to elbow contracture and heterotopic ossification.7
The onset and progression of elbow stiffness is closely related to its inciting causes (see Table 1); most contractures have mixed elements.14
Posttraumatic contracture is most common and is associated with a failure to regain motion after a direct traumatic injury to the elbow joint rather than progressive elbow motion loss. A posttraumatic contracture will typically remain stable over the long-term unless intra-articular degenerative changes ensue that would worsen motion further.
Contractures associated with degenerative or inflammatory arthritis may slowly progress with time due to capsular contraction and impingement on osteophytes or hypertrophic synovium. Such cases will often have episodic flares of swelling and stiffness in combination with steady baseline progression.
It is critical to determine the degree of functional impairment and duration of symptoms for each patient. Management decisions should be based on subjective
impairment and demands, not necessarily the amount of motion loss.11
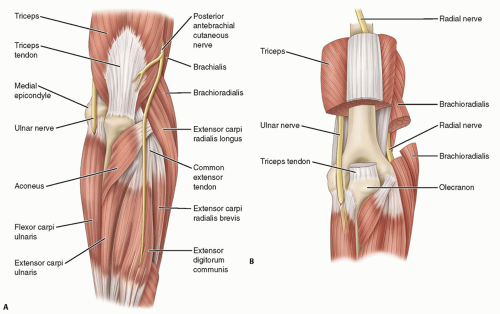
FIG 2 • Anatomic location of the ulnar nerve at the elbow (A), which is contained in the cubital tunnel (B).
Associated disorders should be identified, as peripheral or central neurologic pathology may influence management decisions.
Hand dominance, the patient’s occupation, and the extent of prior therapy should be noted.
The function of the entire ipsilateral and contralateral upper extremities should be tested.
Physical examination
The cranial nerves and cervical spine should be examined to assess for neurologic pathology.
Shoulder motion and strength is assessed.
Careful assessment of the ulnar nerve
The physical examination is critical, as the patients will often not even recognize the presence of ulnar neuropathy in the setting of their adjacent elbow pathology. The elbow flexion and ulnar nerve compression test is the most sensitive for detection of ulnar nerve entrapment at the elbow.21
Table 2 Characterization of Elbow Stiffness by Tissue Involvement
Classification
Relative Occurrence
Location
Description
Static
Most common
Tissues in and around the elbow joint
Capsule, ligaments, heterotopic ossification, articular and cartilaginous components
Dynamic
Less common
Involves muscles around the joint
Poor muscle tone, nerve injuries, and poor excursion of the muscles that cross the elbow joint
From Morrey BF. The stiff elbow with articular involvement. In: Jupiter JB, ed. The Stiff Elbow. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2006:21-30.
Two-point discrimination: Although less than 6 mm is considered normal, careful comparison to the ipsilateral median nerve and contralateral ulnar nerve is necessary to detect subtle signs of nerve damage.
Froment sign and intrinsic hand muscle function: Weakness of the adductor pollicis or interossei may also signify ulnar neuropathy.
The cubital tunnel is palpated to assess for tenderness or a positive Tinel sign.
Elbow range of motion: Flexion and extension are tested with the shoulder flexed to 90 degrees, whereas pronation and supination are evaluated with the elbow held in flexion at the side of the body.
Measure the flat surface of the forearm just proximal to the wrist in comparison to the axis of the humerus. Measurements in supination can be erroneous if tested through the palm because patients can often compensate with significant intercarpal supination.
Measurements can also be erroneous in obese patients who cannot fully adduct the arm to the side, as they will appear to have a deficit in supination if the measurement is compared to the trunk axis and not the abducted humerus, which stresses the importance of using the humerus and not the trunk as the reference point.
Elbow instability: The surgeon should check the ligamentous restraints to varus and valgus stress, as concomitant elbow instability and stiffness may occur after elbow dislocation or subluxation.
Ligaments are assessed with varus and valgus stress at 0 and 30 degrees of flexion as allowed by the patient’s range of motion.
Plain radiographs (anteroposterior [AP] and lateral) are usually adequate.
The AP provides joint line and subchondral bone visualization.
If an elbow is contracted more than 45 degrees, the AP view of the joint line is usually distorted.17
The lateral view may show osteophytes on the olecranon or coronoid processes or within their respective fossae (FIG 3A,B).
Radiographs can be used to follow the maturation process of heterotopic ossification, which usually signifies multiple extrinsic causes of elbow contracture that preclude arthroscopic treatment (FIG 3C).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree