The long head of the biceps tendon has long been recognized as a potential source of pain and cause of shoulder impairment.1,20,21,35
Although biceps tendon pathology can occur in isolation, more frequently, it occurs concomitantly with rotator cuff disease, and its neglect may account for a subset of patients with persistent pain following rotator cuff repair.
Pathology of the long head of the biceps tendon presents in a spectrum, ranging from subtle tendinopathy detected by diagnostic imaging studies, to frank tearing or subluxation visualized intraoperatively.
Because the functional significance of the biceps tendon long head has been the subject of considerable debate, treatment has often been tailored more to patient symptoms, activity levels, and expectations, rather than strict operative criteria.
The ideal indications and optimal operative approach for the treatment of biceps tendinopathy, tears, or instability remain controversial but continue to evolve with advances in arthroscopic technology.
The long head of the biceps brachii (LHB) originates from the supraglenoid tubercle and the superior aspect of the glenoid labrum.
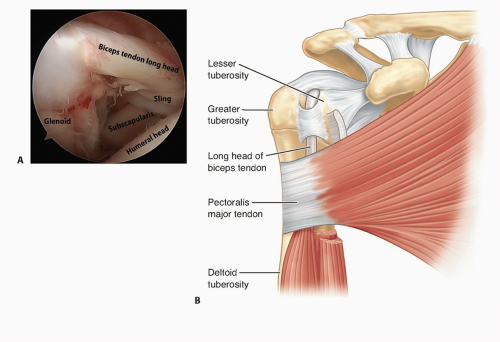
FIG 1 • A. Arthroscopic view of biceps tendon long head and proximal aspect of bicipital groove. B. Anatomy pertinent to surgery involving the LHB tendon.
Multiple anatomic variants of the LHB tendon origin have been described, the most common of which involves an equal contribution from the anterior and posterior labrum.33
The tendon travels intra-articularly (but extrasynovially) an average of 35 ± 5 mm toward the intertubercular (bicipital) groove between the greater and lesser tuberosities.27
Mean LHB tendon length is 9.2 cm, with greatest width at its origin (about 8.5 × 7.8 mm).23
At the site of intra-articular exit lies the annular reflection, or biceps pulley, whose fibers are derived from the superior glenohumeral, the coracohumeral ligament, and the superficial or anterior aspect of the subscapularis tendon (FIG 1). Externally, this structure’s counterpart is the transverse humeral ligament.
The bicipital groove has been a topic of significant study in the literature for its relevance to arthroplasty, and it has been implicated as a contributing factor to tendinopathy involving the LHB.5,25
The dimensions of the bicipital groove vary along its mean 5-cm length. At its entrance, the width ranges from 9 to 12 mm, and the depth is about 2.2 mm. In its midportion, the groove narrows to a mean width of 6.2 mm, whereas its depth remains comparable at approximately 2.4 mm. This considerable groove narrowing may contribute to entrapment of a hypertrophic intra-articular component, referred to as an hourglass biceps.5,15,25
The bicipital groove internally rotates from proximal to distal, with a mean change in rotation of the lateral lip estimated at about 16 degrees.15
The biomechanical significance of the biceps tendon long head is controversial. Some authors have suggested it plays a contributory role in shoulder stability, particularly in overhead athletes.13,24 Based on electromyographic studies, other authors have concluded that the LHB tendon does not contribute to shoulder stability.18,37
The extent of functional loss of forearm supination and elbow flexion strength following biceps tenotomy has not been clearly established and is a source of controversy in the literature but may be estimated at 10%.34
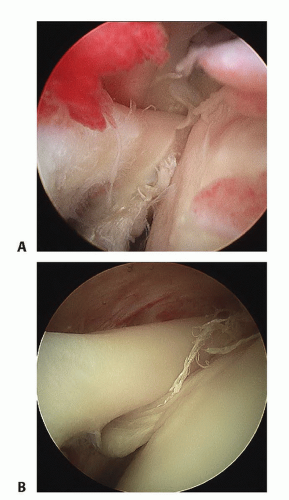
LHB tendinopathy encompasses a spectrum of pathology, including intratendinous signal change, synovitis of the sheath, partial tearing, frank tendon rupture, and instability (FIG 2).
The etiology of LHB tendinopathy is thought to be multifactorial.
Identifiable causes include degenerative changes (usually in association with rotator cuff disease),20,34,35 degenerative osteophyte spurring and stenosis within the bicipital groove,5,25 inflammatory disease, traumatic injury, lesions of the biceps pulley complex or subscapularis tendon, and subtle forms of glenohumeral instability or superior labral anterior posterior (SLAP) tears.
Lesions of the pulley complex or tears of the upper subscapularis tendon or anterior leading edge of the supraspinatus, may permit intra-articular subluxation, LHB instability, and mechanical symptoms.
“Hidden” cuff tears within the rotator interval, or compromise of the annular reflection pulley may permit LHB subluxation, which can lead to pathologic changes to the LHB tendon.
Tears of the superior labrum such as type II SLAP tears, and more subtle patterns of instability such as the peel-back mechanism in throwing athletes, can also cause biceps pain and/or bicipital tendinopathy.
Little is known about the natural history of biceps tendinopathy, so prediction of an individual patient’s clinical course is difficult.
Patients with high-grade tendinopathy, either in isolation or in association with cuff tears, seem to be at risk of subsequent rupture.
Spontaneous LHB tendon rupture often alleviates the chronic pain preceding the event.34
Patients with bicipital tendinopathy may complain of anterior shoulder pain exacerbated by resisted elbow flexion and/or supination.
Diagnosis of biceps pathology is established by the history and character of shoulder pain, as well as appropriate physical examination and diagnostic imaging.
Biceps tendon disorders can present either in isolation or in association with other pathology, typically tears of the rotator cuff.
Pain due to biceps pathology is often referred to the bicipital groove area.
Physical examination findings are variable but typically include focal tenderness to palpation over the course of the biceps long head within the bicipital groove.
In addition, physical examination for biceps pathology should include the following:
Speed test: Considered positive if pain is elicited on resistance against shoulder flexion with the forearm in a supinated and extended position. However, this test has been found to have low sensitivity and specificity (estimated 32% to 68% and 56% to 75%).11
Yergason test: Historically perceived to indicate LHB instability, it is performed by having the patient actively supinate his or her forearm with the elbow flexed 90 degrees and in adduction. Pain or subjective reproduction of symptoms suggests biceps tendinopathy, although sensitivity and specificity for this test is also low.
Active compression test: Primarily assists in differentiating between symptomatic superior labral pathology and acromioclavicular joint pathology. A positive result may suggest biceps tendinopathy in the appropriate clinical context.
Despite the fact that clinical tests are well established, few studies have corroborated their sensitivity, reliability, or accuracy.
Magnetic resonance imaging (MRI) and ultrasound are the primary methods by which biceps tendinopathy is evaluated.
For the diagnosis of subluxation or dislocation of the LHB, ultrasound has a reported sensitivity of 96% to 100% and specificity of 100%.2 For the assessment of complete rupture, or
confirmation of a normal tendon, ultrasound has a sensitivity of 50% to 75% and specificity of 100%. Ultrasound is most useful to demonstrate pathology in the intertubercular groove and perform a dynamic examination of LHB instability. Notwith-standing its established value, a limiting factor of ultrasound is that it has been shown to be highly operator-dependent.
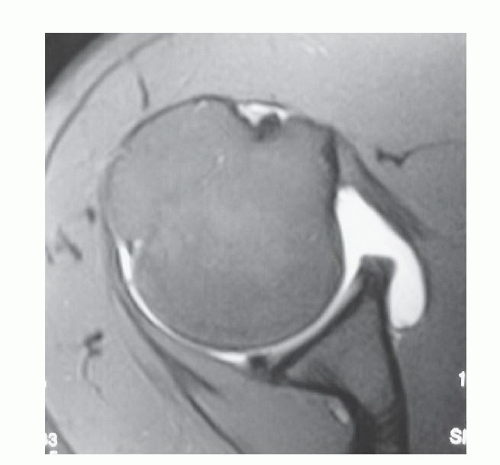
FIG 3 • Coronal MR image showing a normal-appearing biceps tendon in the bicipital groove adjacent to a normal subscapularis tendon and overlying annular reflection pulley.
MRI can identify intratendinous tendon abnormality, bicipital sheath hypertrophy, concomitant superior labral and rotator cuff pathology, the intra-articular course of the tendon, and the relationship of the biceps to the structures of the annular reflection pulley that stabilize it (FIG 3).
LHB tendinopathy or tenosynovitis
LHB partial tear
LHB rupture
LHB instability (subluxation or dislocation)
SLAP tear
Acromioclavicular joint pathology
Anterosuperior rotator cuff tear
Subcoracoid impingement
Subscapularis pathology
Treatment of biceps tendon pathology depends in part on whether it presents in isolation as a primary problem or is associated with other pathology.
Alternative nonoperative management of suspected biceps pathology includes activity modification, a course of nonsteroidal anti-inflammatory medication, and corticosteroid injections targeted directly into the biceps sheath within the intertubercular groove. Such an injection can be both therapeutic and diagnostic.4
Table 1 Indications for Tenodesis and Tenotomy
Procedure
Advantages
Disadvantages
Tenodesis
Better cosmesis Maintenance of length-tension relationship of biceps Decreased risk of fatigue-related cramping Maintenance of forearm supination and elbow flexion strength
Potential pain at tenodesis site Potential failure of tenodesis to heal Potential persistent tenosynovitis Requires postoperative protection until healed
Tenotomy
Typically minimal discomfort No need for placement of implants into proximal humerus or bone-tendon healing High rate of success for pain relief Minimal risk of persistent tenosynovitis Does not require significant postoperative protection
Potential fatigue-related cramping Significant potential for Popeye sign and undesirable cosmetic result Potential for slight to mild forearm supination and elbow flexion deficit
Some clinicians have advocated injection under ultrasound guidance.14 As portable ultrasound units become increasingly available and integrated into clinical practice, it may become the standard by which biceps tendon sheaths are injected.
LHB ruptures traditionally have been treated with nonoperative management based on the perception that this problem rarely results in any significant impairment.
Patients may object, however, to the “Popeye” deformity (bulge in the volar aspect of the midportion of the brachium) (FIG 4) and possible fatigue-related cramping.
Surgical decision making includes patient factors, biceps tendon structural compromise, and concomitant shoulder pathology.
Partial-thickness tearing or fraying exceeding 25% to 50% of the LHB tendon’s diameter, or tendon subluxation or dislocation from its normal position within the bicipital groove, constitute indications for definitive operative treatment. However, these estimates are somewhat empiric rather than scientifically established.
Patient factors influencing treatment include the patient’s age and activity level, occupation, desired recreational activities, and expectations.
Because the biceps tendon is a known “pain generator,” its evaluation and inclusion in the treatment of cuff disorders is particularly important.
Preoperative consideration must be given to anticipate operative strategies if LHB pathology is encountered at the time of surgery.
Operative alternatives in treating biceps tendon disorders include débridement, tenotomy (release of the biceps tendon long head), and tenodesis, in which the biceps is reattached to either bone or soft tissue of the proximal humerus. Each has advantages and disadvantages (Table 1).
The selected surgical approach should take into consideration patient factors, intraoperative findings, and surgeon preference.
Patient factors include age, arm dominance, work, recreational and activity demands, expectations, and perspective on influence of cosmesis.
Intraoperative findings influence decision making in a number of ways, including bone quality; soft tissue quality; the presence of injury to the biceps sling, subscapularis, or anterior supraspinatus; and the presence of instability.
Surgeon factors include arthroscopic proficiency and experience as well as the performance of concomitant surgical procedures that may influence treatment approach.
Few studies have compared surgical alternatives within the same population of patients. Most comparative studies have design flaws due to patient and pathology heterogeneity, in addition to variable surgical procedures due to concomitant pathology.
The ideal indications for débridement versus tenotomy versus tenodesis (soft tissue or bone) remain unclear at this time.
Arthroscopic débridement may be an initial component of many biceps tendon surgical procedures.
In cases of fraying or partial tearing, débridement alone may be adequate to eliminate its contribution as a pain generator.
This is particularly true in cases in which the preoperative workup did not suggest the biceps as a significant component of patient symptoms and when concomitant pathology may otherwise explain the patient’s presentation.
The degree of tendon involvement requiring definite surgical management with either tenotomy or tenodesis has not been scientifically established in the literature and varies depending on concomitant pathology.
Some authors have advocated consideration of addressing the biceps tendon surgically with débridement alone when less than 50% of the tendon’s diameter appears involved (in addition to addressing any concomitant pathology), but assessing the percentage of tendon involvement is an inexact science.
When the biceps is thought to be the predominant cause of symptoms or occurs in isolation, débridement alone may fail to adequately address the pathology and relieve the patient’s symptoms.
With regard to tenodesis studies, biomechanical analysis has focused on construct strength.
One such study found that interference screw tenodesis had a statistically significantly greater resistance to pullout than a double suture anchor technique.27
A recent biomechanical study of the interference screw technique highlighted the importance of placing the screw flush with the humeral cortex or just slightly proud. Recessed screw placement resulted in a higher rate of failure under cyclic loading.28
Some authors have performed recent biomechanical studies investigating the use of a unicortical or bicortical button as an alternative to interference screw or suture anchor fixation.31
Despite biomechanical testing, the actual amount of fixation strength necessary (and whether there is clear superiority of bone or soft tissue reattachment) remains unknown.
One recent study of biceps tenodeses found a statistically significant higher failure rate with proximal techniques compared to more distal techniques, as well as finding greater clinical failure when the biceps sheath (transverse humeral ligament) was not released.29 On this basis, they advocated a more distal tenodesis site lower in the groove.
Another study found a higher rate of persistent pain following tenodesis when the LHB tendon was fixed proximally versus distally within the bicipital groove. On this basis, they advocate a distal arthroscopic technique, with the tenodesis site just proximal to the pectoralis major tendon.19
Others have recommended a mini-open subpectoral technique in the belief that moving further distal along the groove minimizes the risk of postoperative pain.
Recent studies have focused on the risk of complications following mini-open subpectoral biceps tenodesis.26
One study reported the musculocutaneous and radial nerves, as well as the deep brachial artery, to be within 1 cm of the standard medial retractor for this procedure. They further found that the safety margin from the neurovascular structures was enhanced with external rotation, moving the musculocutaneous nerve an additional 11.3 mm away from the tenodesis site.9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree