Arthroscopic Treatment of Anterior Shoulder Instability
Robert A. Arciero
Anthony Parrino
DEFINITION
Glenohumeral stability depends on static and dynamic restraints to ensure stable yet unconstrained range of motion.
Laxity is a physiologic term used to describe the passive translation of the humeral head on the glenoid.
Instability is a pathologic state characterized by abnormal translation of the humeral head on or over the glenoid, leading to frank dislocation, functional impairments, or pain.
The most common direction of glenohumeral instability is anteroinferior.
Anterior instability may be traumatic (occurring with the arm in abduction and external rotation), acquired (subtle instability associated with repeated microtrauma), or atraumatic (multidirectional with underlying anatomic contributions).
ANATOMY
The normal glenoid is broader inferiorly then superiorly (pear-shaped).
The articulating surface of the humeral head is about three times the size of the corresponding glenoid cavity.41
Static and dynamic stability must be provided by a complex interaction between the capsuloligamentous structures, the rotator cuff, the scapular stabilizers, and the biceps muscle.13
Glenoid concavity has three components: osseous glenoid, which is slightly concave; articular cartilage, which is thicker at the periphery; and the glenoid labrum, which deepens glenoid concavity.
The labrum optimizes the surface area of glenohumeral contact and creates a conforming seal with the humerus. The superior labrum provides an attachment for the biceps, whereas the inferior labrum serves as an attachment for the glenohumeral ligaments.14
The capsule and ligaments are intimately related, and different geographic areas contribute to stability based on the anatomic position of the arm.
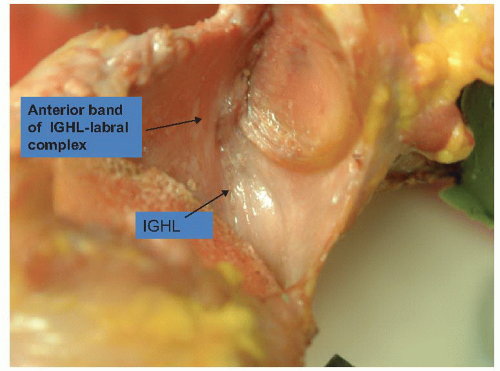
With the arm in an abducted and externally rotated position, the anterior band of the inferior glenohumeral ligament complex is the primary restraint to anterior glenohumeral translation (FIG 1).
The superior and middle glenohumeral ligaments limit inferior translation and anteroposterior (AP) translation with the arm in adduction.
The rotator cuff muscles and other scapulohumeral muscles contribute to the concavity compression mechanism by increasing humeral head compression into the glenoid.
Less important contributors to joint stability include negative intra-articular joint pressure, articular version, and adhesion-cohesion forces.
PATHOGENESIS
Trauma, especially athletic trauma, plays a significant role in recurrent anterior instability.
Overhead athletes can present with more subtle instability.
Repetitive microtrauma contributes to the development of pathologic subluxation.
Injury may result in subluxation and dislocation with spontaneous reduction or dislocation requiring reduction maneuvers.
Traumatic anterior instability is most common in the young, athletic population.
In the 21- to 30-year-old age group, the male/female incidence was reported as 9:1.21
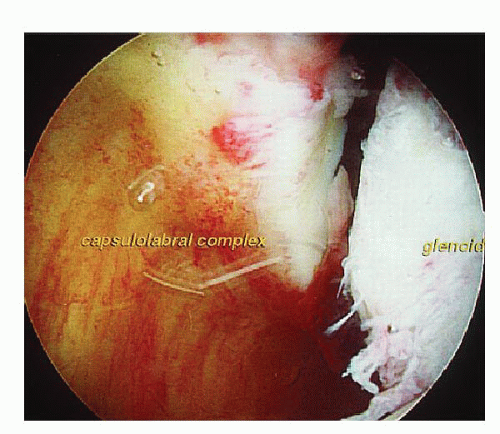
The Bankart lesion (detachment of the anterior inferior labrum and capsule) is considered the fundamental pathoanatomic lesion associated with anteroinferior instability. It may be present in about 90% of all traumatic glenohumeral dislocations (FIG 2).
Recurrent dislocations lead to plastic deformation of the middle and inferior glenohumeral ligaments, contributing to laxity in the “sling” that is designed to restrict translation of the humeral head in abduction.
Bone injuries to the humerus (such as the Hill-Sachs lesion) and the glenoid (bony Bankart or glenoid erosion) are known to contribute to increased glenohumeral translation, resulting in recurrent instability.
Evaluation of these defects is critical in assessing the suitability of arthroscopic repair.
Extensive soft tissue damage is rare but can include the humeral avulsion of the glenohumeral ligaments or a capsular tear.32 In addition, the injured labral tissue may heal medially on the glenoid neck (the so-called anterior labroligamentous periosteal sleeve avulsion [ALPSA lesion]), leading to insufficiency of the inferior glenohumeral ligament and labral complex.34
In the older patient with a traumatic dislocation, rotator cuff pathology must be ruled out through physical examination coupled with appropriate use of soft tissue imaging.
Other soft tissue injuries (capsular tear and neurovascular injury) as well as glenoid and humeral head defects can occur in this age group.
NATURAL HISTORY
Glenohumeral dislocation affects approximately 2% of the general population.21
Few natural history studies exist with long-term follow-up.
A 10-year review of dislocation treated nonoperatively revealed a redislocation rate of about 66% for patients presenting younger than age 22 years.19
Other studies have found the recurrence rate to be between 50% and 64%. Younger patients, especially those involved in overhead or contact sports, are at higher risk.20,40,46
Older patients have much lower redislocation rates (14%).39
Age is the most important predictor of recurrence rates after an initial dislocation. Activity level, especially collision or contact sports, may also increase recurrence rates but has not been definitively proven.
A U.S. Military Academy study showed that over a 4-year period, individuals with a history of prior glenohumeral instability were five times more likely to experience a subsequent instability event within a high-risk athletic population.8
PATIENT HISTORY AND PHYSICAL FINDINGS
The patient’s age and activity level are critical to decision making. Prior surgical procedures should be reviewed in detail.
There are five important questions in the history of instability:
Did the initial instability episode require a reduction?
What was the arm position for the first dislocation? The last dislocation?
What was the disability after the initial incident?
How many episodes of instability have occurred since the initial event? Were they dislocation or subluxation episodes?
What was the magnitude of the trauma associated with the initial event? Have subsequent events required similar force, or have they occurred with less provocation?
The physical examination should begin with inspection from posterior to assess any muscular atrophy of the trapezius, supraspinatus, and infraspinatus and teres minor. Muscle atrophy may point out nerve injury.
Generalized ligamentous laxity should be examined by testing thumb hyperextension and elbow extension.
Active and passive range of motion should be recorded and compared with the contralateral shoulder.
Strength testing should include all important shoulder musculature, with a focus on pain as limiting factor.
The contralateral side is examined when doing the load and shift examination; positive findings indicate lax anterior stabilizers.
It is critical to separate feelings of pain from instability relieved with Jobe relocation. A positive relocation maneuver may spotlight subtle instability.
Axillary nerve function should be assessed by carefully testing motor function of the deltoid and examining sensory distribution.
A positive posterior jerk test with pain and or crepitus elicited with posterior translation of the humeral head over the glenoid rim indicates posteroinferior capsular or labral pathology.
When examining for the sulcus sign, the clinician should compare the result with the contralateral side. Failure of external rotation to eliminate the sulcus sign may indicate multidirectional instability and may aid in decision making as to whether a rotator interval closure is required.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radiographs
Standard AP views of the arm with the arm in slight internal rotation: may show greater tuberosity fracture
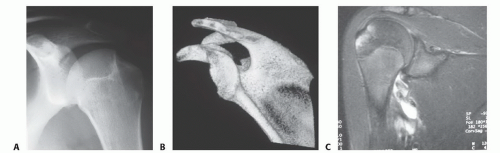
AP views of the glenohumeral joint (FIG 3A)
West Point axillary view: may be used to assess bony avulsions of the inferior glenohumeral ligament, bony Bankart lesions, or anteroinferior glenoid deficiency22,24
Stryker notch view: may be used to examine and quantify a Hill-Sachs lesion
Computed tomography (CT)
Three-dimensional (3-D) reconstructions are especially useful to quantify bone loss. 3-D CT has better accuracy than 2-D CT in determining glenoid defects and is more accurate than magnetic resonance imaging (MRI) in predicting the necessity of open repair versus arthroscopic (FIG 3B).5,33
Indications
Instability episodes while asleep
Instability episodes with minimal trauma after a primary instability episode that required manual reduction
Instability episodes at low degrees of humeral abduction
Failure of any prior instability procedure
Apprehension on examination at low degrees of humeral abduction
Remarkable laxity on load and shift test
Any bony lesion on radiographic evaluation
When bony deficiencies are identified, operative approaches must be adjusted accordingly. Careful consideration must be
given to open instability procedures with bony augmentation in cases of bone involvement (Table 1).
MRI
Contrast enhancement improves the ability to detect labral injury, rotator cuff tears, and articular cartilage lesions.
It may identify humeral avulsion of the glenohumeral ligament lesions and capsular tears, allowing recognition of these infrequent but critical injuries (FIG 3C).
DIFFERENTIAL DIAGNOSIS
Osseous lesions, including clavicle fractures, proximal humerus fractures, and scapular and glenoid fractures
Soft tissue lesions, including deltoid contusions, acromioclavicular joint sprains, and rotator cuff injuries (more common in patients older than 40 years)
Nerve lesions, including injuries to the axillary nerve, suprascapular nerve, and long thoracic nerve. Axillary nerve injury occurs up in up to 5% of patients.
NONOPERATIVE MANAGEMENT
Nonoperative management has traditionally consisted of a period of immobilization followed by intensive physical therapy to improve proprioception and muscular balance around the shoulder girdle. A review noted that recommendations for positioning, length of immobilization, and outcomes are inconsistent at best.6
Table 1 Arthroscopic versus Open Treatment of Anterior Instability
Arthroscopic
Minimal to no bone defects—small, nonengaging Hill-Sachs; no glenoid bone loss
Unidirectional dislocators
Bankart or anterior labroligamentous periosteal sleeve avulsion (ALPSA lesion)
Proper surgeon experience
Open
Bone defects—large Hill-Sachs lesions (> 25% articular surface), glenoid deficiencies > 20%; “inverted pear” large “HAGL” (humeral avulsion of glenohumeral ligament); capsular deficiency or loss (thermal ablation)
Controversial patient populations
Patients with multidirectional instability or hyperlaxity High-demand collision athletes
Work by Itoi et al22 suggested that immobilization in external rotation will reduce recurrence rates after MRI demonstrates coaptation of the Bankart lesion with the arm in external rotation.25 This same author reported a clinical series comparing immobilization in internal rotation versus external rotation after primary dislocation. Immobilization in external rotation reduced the risk of recurrence by 46%.23 Recent reviews of this study have called into question the randomization of patients, and initial results have not been reproducible.
Failure of nonoperative management may be manifested in recurrent symptoms of instability (dislocations, subluxations, or pain) despite adequate nonoperative management and activity modification where appropriate.
SURGICAL MANAGEMENT
The options for surgical management of anterior shoulder instability include arthroscopic, open, and coracoid transfer (Latarjet or Bristow procedure).
Surgical decision making is extremely important to ensure that the appropriate approach is used depending on various patient factors.
The guiding basis for the described arthroscopic technique is that restoration of the normal glenoid labrum anatomy and retensioning of the inferior glenohumeral ligament can be accomplished in a manner that mirrors the open method (FIG 4).
In the senior author’s experience with traumatic anterior instability, a Bankart lesion will typically extend from the 2 o’clock to the 6 o’clock position. To restore anatomy appropriately, the surgeon should be able to instrument and place suture anchors at the inferior aspect of the joint in the 6 o’clock position.
Arthroscopic knots may be sliding, sliding-locking, or simple. Knot selection is less important than consistency in knot security and tissue tensioning.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree