CHAPTER 20 Arthroscopic Synovectomy and Abrasion Chondroplasty of the Wrist
Introduction: Rationale and Basic Science
The wrist is a crucial anatomical link between the hand and forearm, with multiple articular surfaces. When it is afflicted by arthritis and conditions that limit motion, it greatly affects the lives of our patients. The advent of arthroscopy has revolutionized the practice of orthopedic surgery, as well as the practice of hand surgery. Many pioneers have contributed newer techniques, and they have fueled the significant growth in wrist and small–joint arthroscopy.1,2
Wrist arthroscopy has provided a means of examining and treating intra–articular abnormalities. Early reports on arthroscopic wrist synovectomy have noted reduced pain, reduced swelling, and improvement of joint function.3–6 The effects, either transitory or permanent, depend mainly on the activities of the patient and the underlying cause of arthritis. Abrasion chondroplasty of the wrist has not been described at length, but what is known is that in canine models “repair cartilage” (fibrocartilage) is formed in place of articular cartilage.7 Excitingly, abrasion chondroplasty appears to have a role specifically in the treatment of patients with proximal pole hamate arthrosis as well as radiocarpal arthrosis. Preliminary results of this method of treatment have been excellent.8–10 This chapter discusses the indications and techniques for arthroscopic synovectomy and abrasion chondroplasty.
Indications
Arthroscopic synovectomy is an effective modality for the treatment of patients with rheumatoid arthritis, juvenile arthritis (JRA), systemic lupus erythematosus (SLE), and postinfectious arthritis.3–5 Patients who have developed post–traumatic joint contractures and patients with persistent septic arthritis of the wrist despite systemic antibiotics and lavage benefit from arthroscopic synovectomy as well. In the rheumatoid patient, we follow the protocol established by Adolfsson et al.5 We treat those patients who present with radiographic changes of grades 0 through II (and who have failed to respond to pharmacologic treatment and who have a persistent joint synovitis for more than six months) according to the staging system by Larsen, Dale, and Eek.4,11 In nonrheumatoid patients, the radiographic classification system used to evaluate the progression of the disease is the Outerbridge classification system (originally developed for chondromalacia patellae).12
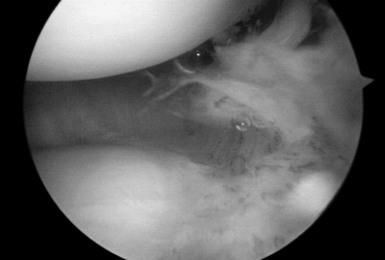
Those patients with early presentation of SLE or reactive arthritis (bacterial or viral), and those patients with osteoarthritis with nominal radiographic changes and florid synovitis, are also considered candidates for wrist synovectomy. Furthermore, those patients who have sustained intra–articular fractures of the distal radius or who have undergone multiple previous wrist interventions also benefit from capsular release, removal of adhesions, and synovectomy (Figure 20.1).
Abrasion chondroplasty is very effective in patients with proximal pole hamate arthritis, specifically those patients with type II lunates (Figure 20.2). This condition causes ulnar–sided pain that occurs when those patients load their wrists in ulnar deviation. When the arthrosis in this area is advanced with exposure of subchondral bone (Outerbridge grade IV), we follow the recommendation of Yao et al. and proceed with an excision of the proximal pole.13 The lunate morphology plays a key role in this condition.

FIGURE 20.2 (A) Plain radiograph AP of a type II lunate. (B) MRI of type II lunate with proximal pole arthrosis.
The type II lunate and its medial facet can lead to arthritis with contact loading of the proximal pole of the hamate. This has been reported in up to 44% of type II lunates versus 2% in type I lunates.9,13–19 Patients with this condition may also have concomitant wrist pathology that can be treated simultaneously, such as triangular fibrocartilage complex (TFCC) tears, lunotriquetral interosseous ligament (LTIL) tear (i.e., hamate arthrosis lunotriquetral ligament tear, or HALT),9 ulnar impaction, and radial–sided, pathology. The presence of a TFCC injury can almost be assured when synovitis along the ulnar side of the wrist is seen during arthroscopy in the absence of any other structural problem.
Radiographic Evaluation
The radiographic evaluation system of Larsen et al. is used for staging the wrist arthritis. We have found that along with an appropriate clinical history dedicated MRI coils and special imaging sequences of the articular cartilage improve the sensitivity and specificity of these studies for detecting chondral defects. This has been a great tool for correlating the clinical and expected arthroscopic findings. Others do not share this viewpoint. In a study of 41 indirect MR arthrograms and 45 unenhanced (nonarthrographic) MR images that were compared to the arthrographic findings, Haims et al. concluded that MRI of the wrist is not adequately sensitive nor accurate in the diagnosis of cartilage defects in the distal radius, scaphoid, lunate, or triquetrum.20
MRI is, however, a good predictor of cases of synovitis and ulnar–sided pathology. Arthroscopic abrasion arthroplasty, subchondral drilling, and microfracture can be performed for the treatment of focal chondral defects in patients with moderate degenerative wrist arthritis or when plain radiographs are suggestive of avascular necrosis. The MRI has been shown to be a sensitive modality that may be used to exclude avascular necrosis as well as to evaluate the extent to which fibrocartilaginous repair tissue has formed postoperatively. This has been demonstrated in the knee, and we have incorporated an MRI evaluation as a part of our postoperative protocol.20,21