A bimodal age distribution exists for patients with distal radius fractures (ie, young adults vs. elderly persons), and they frequently have a different mechanism of injury.
Patients 65 years of age or older have an annual incidence of 8 to 10 fractures of the distal radius per 1000 person-years.
The incidence is seven times higher in women than in men.
Sixteen percent of white women and 23% of white men will sustain a fracture of the distal radius after the age of 50 years.
Fractures of the distal radius are one of the most common skeletal injuries treated by orthopaedic surgeons.
These injuries account for one-sixth of all fractures that are evaluated in the emergency department.
Displaced intra-articular fractures of the distal radius are a unique subset of radius fractures.25
These fractures are a high-energy injury.
This high-energy injury results in comminuted fracture patterns.
These fractures are less amenable to traditional closed manipulation and casting.
The prognosis for these fractures depends on the amount of residual radius shortening, both radiocarpal and radioulnar articular congruity, and associated soft tissue injuries.31
The distal radius serves as a plateau to support the carpus.
The distal radius has three concave articular surfaces: the scaphoid fossa, the lunate fossa, and the sigmoid notch.
The distal articular surface of the radius has a radial inclination averaging 22 degrees and palmar tilt averaging 11 degrees.
Radial-based volar and dorsal ligaments arise from the distal radius to support the wrist.
The sigmoid notch of the distal radius articulates with the ulnar head about which it rotates.
The distal radioulnar joint (DRUJ) is primarily stabilized by the triangular fibrocartilage complex (TFCC).
The sigmoid notch angles distally and medially at an average of 22 degrees.
The biomechanical characteristics of each fracture type depend on the mechanism of injury.
Fernandez and Geissler11 developed a classification based on the mechanism of injury. They noted that the associated ligamentous lesions, subluxations, and associated carpal fractures are related directly to the degree of energy absorbed by the distal radius.
Type I fractures are bending fractures of the metaphysis in which one cortex fails due to tensile stress and the opposite one undergoes a certain degree of comminution (eg, extra-articular Smith or Colles fractures).
Type II fractures are shearing fractures of the joint surface (eg, radial styloid fractures, Barton fracture).
Type III fractures are compression fractures of the joint surface with impaction of the subchondral and metaphyseal cancellous bone (ie, intra-articular comminuted fractures).
Type IV fractures are avulsion fractures of ligamentous attachments, including radial styloid and ulnar styloid fractures, and are associated with radiocarpal fracturedislocations.
Type V fractures are high-energy injuries that involve a combination of bending, compression, shearing, and avulsion mechanisms or bone loss.
Several studies have shown that a high incidence of associated soft tissue injuries is seen with displaced intra-articular distal radius fractures.16, 18, 19, 20, 24, 26, 29
Arthroscopic studies demonstrate a high incidence of injury to the TFCC, followed by the scapholunate interosseous ligament (SLIL), and then the lunotriquetral interosseous ligament (LTIL) (which is the least injured).
A spectrum of injury occurs to the interosseous ligament in which it attenuates and eventually tears and the degree of rotation between the carpal bones increases.
Intra-articular fractures of the distal radius have two pathologies: the associated global injury to the soft tissues and the injury to the bone itself.
The natural history for an intra-articular fracture of the distal radius depends on restoration of anatomy as well as detection and management of any associated soft tissue injuries.4, 11
Knirk and Jupiter20 documented the importance of articular restoration over extra-articular orientation in predicting outcomes for fractures of the distal radius.
They showed solid evidence that the largest tolerable articular step-off is 2 mm.
They demonstrate that the better the restoration of the articular surface, the better the outcome.
A loss in radius length of 2.5 mm will shift the normal load transmitted across the ulna from 20% to 42%, which may lead to various stages of ulnar impaction syndrome.
SLIL and TFCC injuries are often associated with distal radius fractures and may be missed on plain x-ray.
In one study, nearly one-third of fractures had an associated SLIL injury and greater than 60% had a TFCC injury.1
Table 1 Geissler Arthroscopic Classification of Carpal Instability
Grade
Definition
Arthroscopic Findings
Management
I
Attenuation/hemorrhage of interosseous ligament as seen from the radiocarpal joint. No incongruency of carpal alignment in the midcarpal space.
There is a loss of the normal concave appearance between the carpal bones, and the interosseous ligament attenuates and becomes convex as seen from the radiocarpal space. In midcarpal space, the interval between the carpal bones will still be tight and congruent, with no step-off.
Immobilization
II
Attenuation/hemorrhage of the interosseous ligament as seen from the radiocarpal joint. Incongruency/stepoff as seen from the midcarpal space. A slight gap between the carpal bones may be present.
A slight gap (less than the width of a probe) between the carpal bones may be present. The interosseous ligament continues to become attenuated and is convex as seen from the radial carpal space. In the midcarpal space, the interval between the involved carpal bones is no longer congruent, and a step-off is present. In scapholunate instability, palmar flexion of the dorsal lip of the scaphoid will be seen as compared to the lunate. In lunotriquetral instability, increased translation between the triquetrum and lunate will be seen when palpated with a probe.
Arthroscopic reduction and pinning
III
Incongruency/step-off of carpal alignment is seen in both the radiocarpal and midcarpal spaces.
The interosseous ligament has started to tear, usually from volar to dorsal, and a gap is seen between the carpal bones in the radiocarpal space. A probe often is helpful to separate the involved carpal bones in the radiocarpal space. In the midcarpal space, a 2-mm probe may be placed between the carpal bones and twisted.
Arthroscopic/open reduction and pinning
IV
Incongruency/step-off of carpal alignment is seen in both the radiocarpal and midcarpal spaces. Gross instability with manipulation is noted.
A 2.7-mm arthroscope may be passed through the gap between the carpal bones. The interosseous ligament is completely detached between the involved carpal bones. This is the “drive-through” sign, when the arthroscope may be freely passed from the radiocarpal space through the tear to the midcarpal space.
Open reduction and repair
In another study, SLIL injuries were found in more than half, LTIL injuries in one-third, and TFCC in 60%. Only 17% of patients were free of any of the three injuries.28
Untreated complete tears of the SLIL, which are highly associated with radial styloid fractures, may progress to a wrist with scapholunate advanced collapse.
A thorough history should be obtained, including the circumstances surrounding the injury as well as any additional injuries.
Neurologic basis
Cardiac basis
Patients’ level of independence, dominant hand, status with assisted devices, work, activity level, and support structure should be determined.
Physical examination, while concentrating on the wrist, should also include the hand, elbow, and shoulder to check for concomitant injuries.
The hand, wrist, forearm, arm, and shoulder must be carefully inspected for open injury so that tetanus and antibiotic prophylaxis may be initiated if necessary.
A thorough distal sensory and motor function examination should be carried out in an organized manner.
Vascular examination should include palpation of both the radial and ulnar pulses and determination of capillary refill time.
Precise palpation is used to define areas of potential trauma.
Diminished sensibility, pallor, altered capillary refill, increased tenseness of the soft tissues, and pain out of proportion should raise suspicion for significant soft tissue injury, including compartment syndrome.
Posteroanterior (PA), oblique, and lateral radiographs are the primary radiographic studies used to workup distal radius fractures.
Radiographs of the uninvolved contralateral extremity are useful to compare radial inclination, ulnar variance, and sigmoid notch anatomy.
PA projections are useful to evaluate the radial inclination, radius height, presence of ulnar styloid fractures, widening of the DRUJ, widening of intercarpal spaces, and intra-articular involvement (FIG 1A).
Standard radiographic parameters of the distal radius include radial inclination of 22 degrees (range 13 to 30 degrees), radius length of 12 mm (range 8 to 18 mm), and volar tilt of 11 degrees (range 1 to 21 degrees).
Ulnar variance should be measured with the shoulder in 90 degrees of abduction, the elbow at 90 degrees of flexion, and the wrist in neutral pronation-supination.
A lateral projection is used to assess volar and dorsal tilt of the distal fragment, dislocation or subluxation of the DRUJ or carpus, lunate angulation, and dorsal comminution (FIG 1B).
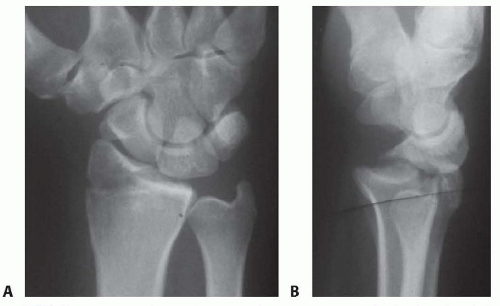
FIG 1 • A. PA radiographic view showing a minimally displaced radial styloid fracture fragment. B. The lateral view shows a complete fracturedislocation of the wrist.
A modified lateral radiograph with the beam angulating 10 to 30 degrees proximally improves visualization of the articular surface and evaluation of the volar rim of the lunate facet represented by the anterior teardrop.
An additional 30-degree anteroposterior (AP) cephalic projection is useful to evaluate the dorsal ulnar margin of the distal radius.
Oblique radiographs are very helpful because major fracture fragments may be rotated out of their anatomic planes.
Computed tomography (CT) evaluation, particularly threedimensional CT, can further delineate fragment location, joint compression, and rotation.
Magnetic resonance imaging (MRI) evaluation is useful in assessing for associated soft tissue injuries such as TFCC tears, interosseous ligament injuries, and carpal fractures.
Radiographic signs that demonstrate that the distal radius fracture is likely unstable and closed reduction would be insufficient include the following21:
Lateral tilt greater than 20 degrees dorsal
Dorsal comminution greater than 50% of the lateral width
Initial fragment displacement greater than 1 cm
Volar translation greater than 2 mm
Initial radius shortening more than 5 mm
Intra-articular step-off greater than 2 mm
Associated ulnar fracture
Severe osteoporosis
Age older than 60 years
Carpal bone fracture
Metacarpal or phalangeal fracture
DRUJ disruption
Essex-Lopresti lesion
Interosseous ligament tear
Carpal dislocation (perilunate)
Displaced fractures of the distal radius are reduced using an adequate anesthetic agent.
Knowledge of the mechanisms of injury helps facilitate manual reduction. Force is applied opposite the force that caused the fracture.
Gentle traction is necessary to disimpact the fracture fragments, followed by palmar translation of the hand and carpus in respect to the radius.
The radius articular surface will rotate around the intact volar cortical lip to restore volar inclination with palmar translation.
Care must be taken to avoid trauma to the skin during the reduction maneuver, particularly in elderly patients where the skin may be fragile.
A splint is supplied following the reduction. No consensus has been established regarding wrist or forearm position, longarm versus short-arm immobilization, or splint versus cast.
Extreme positions of wrist flexion and ulnar deviation should be avoided.
Postreduction radiographs are taken in plaster.
Depending on stability of the fracture, most patients treated nonoperatively require weekly visits for the first 3 weeks to monitor fracture reduction.
In patients older than 65 years, one-third of initially undisplaced fractures subsequently collapsed to some degree.
One study of elderly patients with moderately displaced fractures of the distal radius found that two-thirds of the correction obtained by closed manipulation was lost at 5 weeks.
Patients with minimally displaced or nondisplaced fractures of the distal radius treated nonoperatively must be made aware of possible complications, including rupture of the extensor pollicis longus tendon, carpal tunnel syndrome, and compartment syndrome.
Elderly patients typically tolerate nonoperative management well.
Distal radius fractures without extensive metaphyseal comminution are ideal candidates for arthroscopic-assisted fixation with K-wires or cannulated screws.14, 15, 22
Radial styloid fractures
Impacted fractures
Die-punch fractures
Three-part T-type fractures and four-part fractures with metaphyseal comminution are best treated with a combination of volar plate stabilization. Wrist arthroscopy is used as an adjunct to fine-tune the articular reduction and evaluate for associated soft tissue lesions.
Distal radius fractures that may be minimally displaced, and fractures with strongly suspected associated soft tissue injury, also are candidates for arthroscopic-assisted fixation to stabilize the fracture but, more importantly, to evaluate and treat the acute associated soft tissue injury.
Stabilization of associated ulnar styloid fragments is controversial.20 Wrist arthroscopy provides a rationale as to when to stabilize an ulnar styloid fragment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








