Arthroscopic Meniscectomy
Frederick M. Azar
Nicolas S. Bonnaig
DEFINITION
Irreparable meniscal tears are those for which no healing response is possible.
This may include all or part of a meniscus, prompting partial, subtotal, or total meniscectomy.
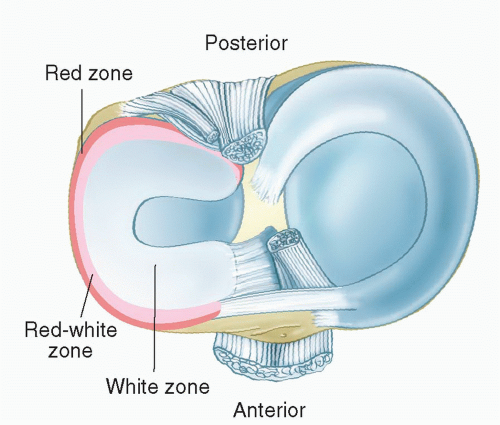
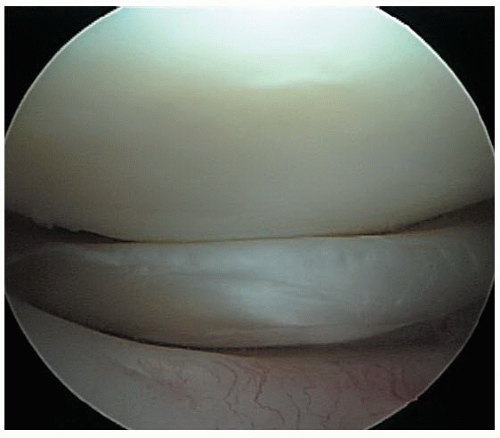
Meniscal injuries in the “white zone” (central avascular portion; FIG 1) most often require partial meniscectomy.
This usually involves the inner two-thirds of the meniscus.
Symptomatic tears of discoid lateral menisci also may require partial or subtotal saucerization of the meniscus.
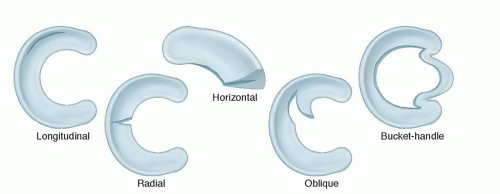
Numerous classifications of tears of the menisci have been proposed based on location or type of tear, etiology, and other factors; most of the commonly used classifications are based on the type of tear found at surgery (FIG 2).
Longitudinal tears
Transverse, radial, and oblique tears
A combination of longitudinal and transverse tears
Tears associated with cystic menisci
Tears associated with discoid menisci
The most common type of tear is the longitudinal tear, usually involving the posterior segment of either the medial or lateral meniscus.
More lateral meniscal tears have been diagnosed than medial tears.
Although no definitive study comparing the incidence of medial to lateral tears has been reported, the two types are believed to occur with almost equal frequency.
Most partial-thickness tears involve the inferior rather than the superior surface of the meniscus.
Certain patterns of meniscal tears are associated with mechanical locking.
Small longitudinal tears limited to the posterior horn usually are not capable of producing locking but rather cause pain, recurrent swelling, and subjective instability.
Extensive longitudinal tears can cause locking by displacing into the intercondylar notch. These unstable tears often are referred to as bucket-handle tears.
A pedunculated fragment may result if either the posterior or anterior attachment of the bucket-handle fragment becomes detached.
Transverse, radial, or oblique tears can occur in either meniscus but are more common in the lateral, usually at the junction of the anterior and middle thirds.
Transverse tears also can result from degenerative changes that make the meniscus less mobile.
Complex transverse and longitudinal tears may occur with degeneration or repeated traumatic episodes.
Meniscal cysts frequently are associated with tears and are nine times more common on the lateral than on the medial side.
Discoid menisci are abnormal in terms of both mobility and increased tissue bulk, making them vulnerable to compression and rotary stress.
ANATOMY
The menisci are crescents that are roughly triangular in cross-section.
They cover one-half to two-thirds of the articular surface of the corresponding tibial plateau.
They are composed of dense, tightly woven collagen fibers arranged in a pattern, providing great elasticity and ability to withstand compression.
The major orientation of collagen fibers in the meniscus is circumferential.
Radial fibers and perforating fibers also are present (FIG 3A).
The arrangement of these collagen fibers determines to some extent the characteristic patterns of meniscal tears (FIG 3B,C).
When meniscal samples are tested by applying a force perpendicular to the fiber direction, the strength is decreased to less than 10% because collagen fibers function primarily to resist tensile forces along the direction of the fibers.6
The circumferential fibers act in a similar manner as metal hoops placed around a pressurized wooden barrel: The tension in the hoops keeps the wooden staves in place (FIG 3D,E).
Hoop tension is lost when a single radial cut or tear extends to the capsular margin.
The peripheral edges of the menisci are convex, fixed, and attached to the inner surface of the knee joint capsule, except where the popliteus is interposed laterally; the peripheral edges also are attached loosely via coronary ligament to the borders of the tibial plateaus.
The inner edges are concave, thin, and unattached.
The menisci are largely avascular except near their peripheral attachment.
The inferior surface of each meniscus is flat, whereas the superior surface is concave, corresponding to the contour of the associated bony anatomy.
The medial meniscus is a C-shaped structure larger in radius than the lateral meniscus, with the posterior horn being wider than the anterior (FIG 4).19,24,30
The anterior horn is attached firmly to the tibia anterior to the intercondylar eminence and to the anterior cruciate ligament (ACL).
Most of the weight is born on the posterior portion of the meniscus.
The posterior horn is anchored immediately in front of the attachments of the posterior cruciate ligament posterior to the intercondylar eminence.
Its entire peripheral border is firmly attached to the medial capsule and through the coronary ligament to the upper border of the tibia.
The lateral meniscus is more circular in form, covering up to two-thirds of the articular surface of the underlying tibial plateau.
The anterior horn is attached to the tibia medially in front of the intercondylar eminence.
The posterior horn inserts into the posterior aspect of the intercondylar eminence and in front of the posterior attachment of the medial meniscus.
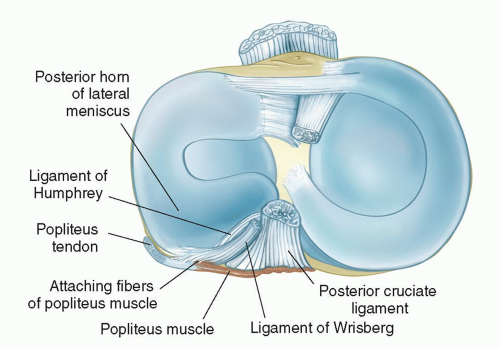
The posterior horn often receives anchorage also to the femur via the ligament of Wrisberg and the ligament of Humphrey and from fascia covering the popliteus muscle and the arcuate complex at the posterolateral corner of the knee.
The inner border, like that of the medial meniscus, is thin, concave, and free.
The tendon of the popliteus muscle separates the posterolateral periphery of the lateral meniscus from the joint capsule and the lateral collateral ligament. This tendon is enveloped in a synovial membrane and forms an oblique groove on the lateral border of the meniscus.
The lateral meniscus is smaller in diameter, thicker in periphery, wider in body, and more mobile than the medial meniscus.
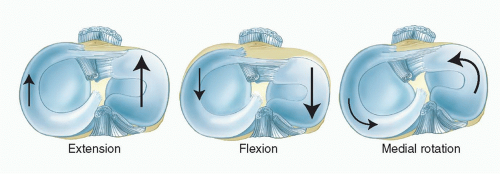
The menisci follow the tibial condyles during flexion and extension; but during rotation, they follow the femur and move on the tibia (FIG 5).
Consequently, the medial meniscus becomes distorted.
Its anterior and posterior attachments follow the tibia, but its intervening part follows the femur; thus, it is likely to be injured during rotation.
However, the lateral meniscus, because it is firmly attached to the popliteus muscle and to the ligament of Wrisberg or of Humphrey, follows the lateral femoral condyle during rotation and therefore is less likely to be injured.
In addition, when the tibia is rotated internally and the knee flexed, the popliteus muscle, by way of the arcuate ligament complex, draws the posterior segment of the lateral meniscus backward, thereby preventing the meniscus from being caught between the condyle of the femur and the plateau of the tibia.
The vascular supply to the medial and lateral menisci originates predominately from the lateral and medial geniculate vessels (both inferior and superior).
Branches from these vessels give rise to a perimeniscal capillary plexus within the synovial and capsular tissue, which supplies the peripheral border of the meniscus throughout its attachment to the joint capsule.
These vessels are oriented in a predominantly circumferential pattern, with radial branches directed toward the center of the joint.
Arnoczky and Warren6,7 used microinjection techniques to show that the depth of peripheral vascular penetration is 10% to 30% of the width of the medial meniscus and 10% to 25% of the width of the lateral meniscus.
The medial geniculate artery, along with a few terminal branches of the medial and lateral geniculate artery, also supplies vessels to the menisci through the vascular synovial covering.
The menisci have several proposed functions in the knee joint.
They act as a joint filler, compensating for gross incongruity between the femoral and tibial articulating surfaces.
They are believed to have a joint lubrication function, distributing synovial fluid and aiding the nutrition of the articular cartilage. A study by Ciccotti et al10 appears to confirm this function: In a series of patients undergoing arthroscopy for meniscal pathology, 85% of 252 patients aged 50 to 59 years and 86% of those aged 60 years or older had articular cartilage changes.
They serve as important secondary stabilizers in all planes, especially providing rotary stability to the joint, and allowing for smooth gliding or rotary motion as the knee extends.
PATHOGENESIS
Meniscal injuries generally have either a traumatic or degenerative cause.
Traumatic injuries in young, active individuals are often associated with tears of the anterior and posterior cruciate ligaments. Traumatic tears are more common in the lateral meniscus.
The most common traumatic tears are vertical longitudinal tears, followed by vertical transverse tears.
Degenerative meniscal tears occur most often in patients older than 40 years of age, typically with no history of a specific traumatic event and often in association with other degenerative changes in the knee joint.
Degenerative tears of the menisci are more common in the medial meniscus and have minimal or no healing potential.24
The most common degenerative tear patterns are horizontal cleavage tears, flap tears, and complex tears (see FIG 2).
Miller et al22 classified meniscal tears based on their location in three zones of vascularity and use this classification to determine the potential for healing after repair (see FIG 1):
Red: fully within the vascular area
Red-white: at the border of the vascular area
White: within the avascular area
After injury within the peripheral vascular zone, a fibrin clot forms that is rich in inflammatory cells.
Vessels from the perimeniscal capillary plexus proliferate throughout this fibrin scaffold and are accompanied by the proliferations of differentiated mesenchymal cells.
Eventually, the lesion is filled with cellular fibrovascular scar tissue that glues the wound edges together and appears continuous with the adjacent normal meniscal fibrocartilage.
Experimental studies in animals have shown that complete radial lesions of the meniscus are completely healed with a young fibrocartilaginous scar by 10 weeks, although several months are required for maturation to fibrocartilage that appears normal.
Controversy exists about the ability of a meniscus or a meniscus-like tissue to regenerate after meniscectomy.
It is now generally accepted that to have any regeneration, the entire meniscus must be resected to expose the vascular synovial tissue, or, in subtotal meniscectomy, the excision must extend to the peripheral vasculature of the meniscus.
The frequency and degree of regeneration of the meniscus have not been determined precisely.
Traumatic lesions of the menisci are produced most commonly by rotation as the flexed knee moves toward an extended position.
The most common location for injury is the posterior horn of the meniscus, and longitudinal tears are the most common type of injury.
The length, depth, and position of the tear depend on the position of the posterior horn in relation to the femoral and tibial condyles at the time of injury.
Less significant trauma is needed to injure a meniscus that is degenerated or made less mobile from prior injury, previous surgery, disease, or congenital anomaly (ie, discoid meniscus).
The menisci are also at increased risk in the presence of joint incongruities, ligamentous instability, profound muscle weakness, or congenitally relaxed joints.
As the knee is internally rotated during flexion, the medial meniscus is forced posteriorly. If the peripheral attachment stretches or tears, the posterior part of the meniscus is forced centrally, caught between the femur and tibia, and torn longitudinally as the knee extends.
If this longitudinal tear extends anteriorly beyond the medial collateral ligament, the inner segment of the meniscus is caught in the intercondylar notch and cannot return to its former position; thus, a classic bucket-handle tear with locking of the joint is produced (FIG 6).
The same mechanism can produce a posterior peripheral or a longitudinal tear of the lateral meniscus.
Because of its mobility and structure, the lateral meniscus is not as susceptible to bucket-handle tears, but incomplete transverse tears are more common here than in the medial meniscus.
NATURAL HISTORY
The effects of meniscectomy on joint laxity have been studied for anteroposterior and varus-valgus motions and rotation.
These studies indicated that the effect on joint laxity depends on whether the ligaments of the knee are intact and whether the joint is bearing weight.
In the presence of intact ligamentous structures, excision of the menisci produces small increases in joint laxity.
When combined with ligamentous insufficiency, these increased instabilities caused by meniscectomy are greatly exaggerated.
In an ACL-deficient knee, medial meniscectomy has been shown to increase tibial translation by 58% at 90 degrees, whereas primary anterior and posterior translations were not affected by lateral meniscectomy.3
Anatomically, the capsular components that attach the lateral meniscus to the tibia do not affix the lateral meniscus as firmly as they do the medial meniscus.
These results indicate that in contrast to the medial meniscus, the lateral meniscus does not act as an efficient posterior wedge to resist anterior translation of the tibia on the femur.
Therefore, in knees that lack an ACL, the lateral meniscus is subjected to different forces than those that occur on the medial side.
Allen et al,3 in a biomechanical study, determined that force in the medial meniscus increased significantly in response to an anterior tibial load after ACL transection, which may account for some of the differences in injury patterns between the medial and lateral menisci in the anterior cruciate-deficient knee.
Walker and Erkman29 noted that under loads of up to 150 kg, the lateral meniscus appeared to carry 70% of the load on that side of the joint, whereas on the medial side the load was shared about equally by the meniscus and the exposed articular cartilage.
Medial meniscectomy decreases contact area by 50% to 70% and increases contact stress by 100%.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree