Fig. 9.1
(a) Bernageau view illustrating glenoid without bone loss. Published with kind permission of © Dr. Felix H. Savoie, III 2015. All Rights Reserved. (b) Bernageau view illustrating glenoid with bone loss. Published with kind permission of © Dr. Felix H. Savoie, III 2015. All Rights Reserved
There has been considerable attention paid to the concept of the “inverted pear” glenoid, which represents a great risk for failure after soft tissue stabilization and the method to accurately quantify this bone loss [1–4, 27, 29, 33–35]. Itoi et al. has shown that as little as 6 mm of glenoid bone loss leads to significantly increased instability of the glenohumeral joint. [4] Percentage of bone loss based on 3-D CT scan measurements and during arthroscopy have both been described [2, 3, 29, 36]. Anywhere from as little as 19–30 % glenoid bone loss has been shown to lead to significant increases in instability. Treatment based on percentage of glenoid bone loss has not been fully defined as of yet. We can, however, guide treatment based on several of these prior studies. In general, recurrent instability patients with <20 % bone loss may be considered for soft tissue stabilization procedures alone, whereas those with >25 % should be considered for bony augmentation.
We do not routinely perform MRI or MR arthrography as part of the workup for recurrent anterior shoulder instability. While these are helpful for assessing soft tissue lesions such as humeral avulsion of the glenohumeral ligament (HAGLs), Bankart lesions, and capsular injuries, these injuries may be better visualized during diagnostic arthroscopy.
The goal of a thorough clinical exam and radiographic workup is to identify clinical situations in which a soft tissue Bankart repair alone would be inadequate for stability and when a Latarjet procedure would be indicated. It is important to note that even with full preoperative radiographic workup, the decision to perform an arthroscopic Latarjet procedure sometimes is made after arthroscopic examination.
Indications and Contraindications
The arthroscopic Latarjet procedure is indicated in symptomatic patients with recurrent anterior shoulder instability and significant (>20 %) glenoid bone loss. An engaging or “on-track” humeral head defect is often present. Patients at high risk of redislocation secondary to increased activity levels such as rugby players and baseball pitchers are ideal candidates for the arthroscopic Latarjet procedure. The procedure allows for quicker rehabilitation time and return to sport for this population. Patients with epilepsy, voluntary dislocators, high-risk surgical candidates, and those unable to comply with postoperative rehabilitation protocols are not ideal candidates for surgery.
Conservative Treatment
Conservative treatment in this population is reserved for those patients not suitable for operative intervention as mentioned previously and/or elderly low-demand patients. Treatment is primarily based on strengthening periscapular and rotator cuff musculature. Ideal patients for conservative treatment have less than 20 % glenoid bone loss and are low demand. Successful conservative treatment entails maintenance of a stable shoulder with activities of daily living.
Arthroscopic Treatment
As stated, arthroscopic Latarjet procedure is indicated after appropriate preoperative workup has identified patients with significant (>20 %) glenoid bone loss and symptoms of instability. It is imperative to recognize scenarios where isolated soft tissue procedures are likely to fail. A surgeon’s personal experience and comfort level should dictate the surgical treatment performed.
The preference at our institution is to harvest the coracoid via a mini-open approach, harvest iliac crest, or use fresh osteochondral distal tibial articular surface [19] to reconstruct the glenoid, depending on age of patient, ligamentous laxity, and prior surgical history. If coracoid transfer or iliac crest is the source, the capsule is repaired arthroscopically to the native glenoid, making the graft extra-articular. Theoretically, this could reduce odds of developing arthritis. When the distal tibial articular surface is the bone source, we repair the capsule to the perimeter of the graft, making the bone transfer intra-articular. This combined technique of mini-open/arthroscopic bone grafting with capsule preservation and repair has been termed the “Tulane Technique.”
Technique
The patient is placed in the lateral decubitus position, rolled back approximately 30°. A standard posterior portal is made, and a diagnostic arthroscopy performed to confirm the amount of bone loss as well as evaluate the entire glenohumeral joint (Fig. 9.2).
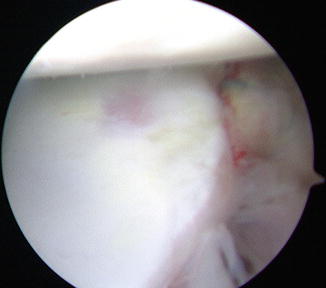
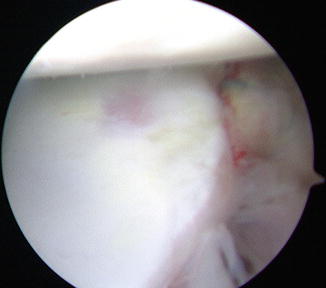
Fig. 9.2
Anterior superior viewing portal in a left shoulder demonstrating anterior glenoid bone loss. Published with kind permission of © Dr. Felix H. Savoie, III 2015. All Rights Reserved
An incision is made from the tip of the coracoid distally for approximately 3–5 cm (Fig. 9.3a). The coracoid is exposed and harvested using a standard Latarjet technique. We prefer to use a guide to ensure proper placement of the drill holes in the coracoid, but the harvest can certainly be performed free hand. The pectoralis minor is released, and the coracoid is attached to the Lafosse Latarjet holding device (Fig. 9.3b). The posterior concave surface of the coracoid is lightly abraded using a high-speed spur. The portion that will be the articular side (lateral) is also evaluated and burred to a smooth surface. The edge of the graft that will lie adjacent to the glenoid is marked to allow easier visualization once it is placed in the joint.
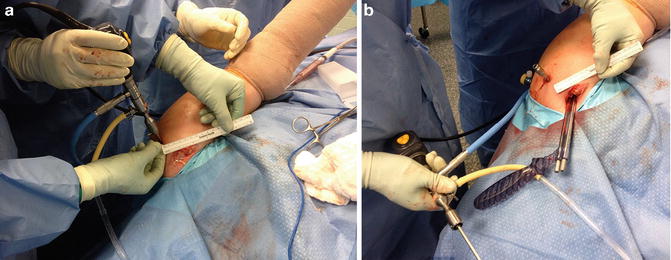
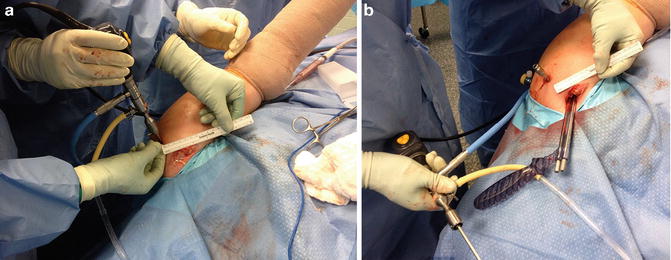
Fig. 9.3
(a) Anterior incision for coracoid graft harvest. Published with kind permission of © Dr. Felix H. Savoie, III 2015. All Rights Reserved. (b) Anterior incision with coracoid graft holder in place. Published with kind permission of © Dr. Felix H. Savoie, III 2015. All Rights Reserved
The arthroscope is then inserted back into the joint, and an anterior-superior viewing portal established just anterior to the supraspinatus tendon (not through the tendon). Utilizing the anterior incision, a cannula is inserted over the subscapularis and the capsule elevated completely from the glenoid neck and retracted. It is important that the capsule elevation from the glenoid continue to the attachment of the posterior-inferior glenohumeral ligament (PIGHL) on the posterior glenoid in order to allow later repair without limiting external rotation (Fig. 9.4). A crochet hook is inserted percutaneously to retract the capsule during the next step of the surgery (Fig. 9.5).
Fig. 9.4
The capsule is elevated to the level of the PIGHL attachment so that external rotation is not limited after repair. Published with kind permission of © Dr. Felix H. Savoie, III 2015. All Rights Reserved
Fig. 9.5
Crochet hook inserted to keep capsule retracted. Published with kind permission of © Dr. Felix H. Savoie, III 2015. All Rights Reserved
A switching stick is inserted via the posterior portal and passed across the glenoid, through the muscle belly of the subscapularis and out the small anterior incision. A series of dilators used to facilitate cannula passage are then inserted over the switching stick to create an atraumatic path through the subscapularis muscle. The graft, still attached to the holder, is slid along the switching stick into the joint under arthroscopic visualization through this dilated path. The graft is positioned with its center in the center of the defect, usually 4 O’clock, and it is fixated in this position by two Kirschner wires that are drilled across the glenoid neck exiting out the posterior aspect of the shoulder. Each wire is clamped to prevent accidental removal; the inferior hole is drilled, measured and the screw inserted. The length of the screw is usually 36–38 mm. The more superior hole is managed the same way. The anterior aspect of the bone block can be visualized with the arthroscope to confirm full seating of the screws into the bone graft (Fig. 9.6a, b). Any malalignment or protuberances on the bone graft can be burred at this time.
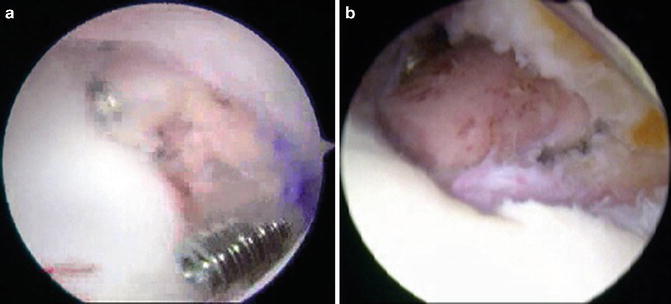
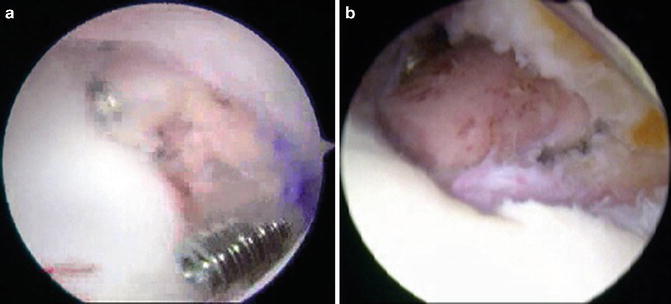
Fig. 9.6
(a) Graft being placed through subscapularis onto glenoid. Published with kind permission of © Dr. Felix H. Savoie, III 2015. All Rights Reserved. (b) Bone block position on glenoid. Published with kind permission of © Dr. Felix H. Savoie, III 2015. All Rights Reserved
The retractor holding the capsule is then removed, allowing the capsule to fall back toward the glenoid. A double-loaded suture anchor is placed into the native glenoid via the anterior-inferior portal (that had been made through the small incision). The arthroscope may be placed posteriorly, and the superior portal used to shift the anterior/inferior capsule in a superior direction. A retrograde retriever is then utilized to create two double, oblique vertical mattress sutures so that the capsule can be repaired over the bone block and back to the native glenoid. This is performed with the arm externally rotated 90° and completes the reconstruction (Fig. 9.7).
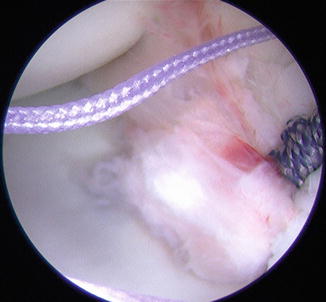
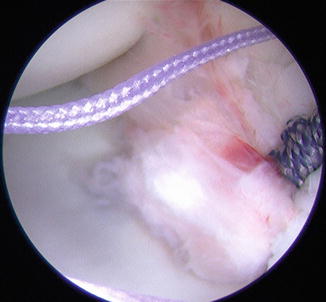
Fig. 9.7
Capsule repaired over bone block. Published with kind permission of © Dr. Felix H. Savoie, III 2015. All Rights Reserved
Fluoroscopy can be used to confirm screw placement. Radiographs are taken in recovery room (Fig. 9.8).


Fig. 9.8
Postoperative radiograph illustrating proper placement of screws. Published with kind permission of © Dr. Felix H. Savoie, III 2015. All Rights Reserved
Postoperative Rehabilitation
The patient is placed in an abduction sling for the early postoperative phase. Scapular retraction is started immediately. Limited active isometric exercises are also started week 1. Once the shoulder “settles down,” usually 3–4 weeks, the immobilization device is discontinued and active exercise initiated. There is no stretching allowed in physical therapy. X-rays are taken at 3 and 6 weeks, and we attempt to obtain a computed tomography (CT) scan at the 6–8 week mark.
Complications
Over time, multiple studies have established the Latarjet as a viable option for treating glenoid bone loss; however, more recent reports have uncovered associated technical difficulties [7, 20, 22, 37–39]. While the Latarjet procedure can reliably stabilize the chronically unstable shoulder, it is not without potential setbacks. Complications may consist of hematoma, infection, neurovascular injury, hardware impediments (broken, migrated), coracoid/glenoid fracture, coracoid lysis, osteoarthritis, decreased external rotation, and recurrent instability/reoperations.
In the most recent systematic review to date, Bhatia et al. [20] examined five studies which dealt with postoperative complications in open and arthroscopic cases [3, 7, 11, 22, 39]. Burkhart and De Beer [3] reported a 5 % complication rate in a cohort of 102 patients (2 hematomas, 2 asymptomatic screw loosenings, 1 asymptomatic fibrous union). Lafosse and Boyle [7] reported 2 hematomas, 1 intraoperative graft fracture, 1 transient musculocutaneous nerve palsy, 4 cases of nonunion, and 3 cases of screw osteolysis in their first 100 patients. Scmhid et al. [22] documented a 12 % complication rate (6/49 patients) that included 4 delayed wound healing cases, 1 case of adhesive capsulitis, and 1 malunion of the coracoid graft.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








