Osteochondritis dissecans (OCD) is described as a focal, idiopathic alteration of subchondral bone with risk for instability and disruption of adjacent articular cartilage that may result in premature osteoarthritis.25
The most common location for OCD lesions to occur is in the knee; more specifically, on the lateral aspect of the medial femoral condyle.
The morphology of the OCD in this anatomic position varies and can appear as an initial softening of the subchondral bone and overlying articular cartilage, which can progress to early articular cartilage separation and later osteochondral separation (FIG 1).
Although the exact pathogenesis of OCD remains unclear, several hypotheses about the etiology of OCD have been proposed—ischemia, trauma, accessory centers of ossification, and genetic factors.
Ischemia
In 1870, Sir James Paget had described what was later thought to be OCD as “quiet necrosis.”24 Green and Banks14 also theorized that OCD was due to ischemia of subchondral bone leading to the development of OCD.
Later studies on the epiphyseal artery construct, however, would conclude that this hypothesis is less likely to explain the etiology.
Microtrauma
Fairbank’s12 early work described trauma as an etiology for OCD. Smillie27 strongly supported Fairbank’s “tibial spine” theory for the etiology of OCD. Although this may offer an explanation for the classic location on the lateral aspect of the medial femoral condyle, it does not account for other locations of OCD in the knee.
A theory of repetitive microtrauma is appealing given that multiple studies have shown up to 60% of patients with OCD report being involved in sporting activities.3,15,21
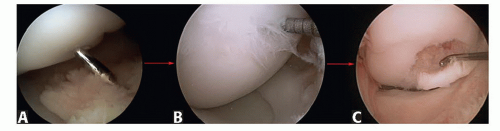
FIG 1 • Showing three common morphologies of OCD lesions of the knee. A. Ballotable, intact cartilage lesion. B. Fissured “locked door” lesion. C. Hinged trap door lesion.
Accessory centers of ossification
The one hypothesis that may unite all previous evidence is that of epiphyseal endochondral ossification described by Ribbing.26
These “accessory centers of ossification” were described by Ribbing26 and shown to occur in the classic location of the medial femoral condyle.
Genetic
Although a solitary lesion is the most common finding of OCD, cases of joint bilaterality, multiple lesions in a single joint, and reports of OCD in twin studies have provided support for a hypothesis of genetic predisposition.
Hughes et al16 documented the natural history of skeletally immature OCD of the knee through serial magnetic resonance imaging (MRIs) over a 5-year period, which they correlated with arthroscopy and clinical outcomes.
In this small series, they demonstrated that all lesions with intact cartilage will likely heal with conservative treatment; however, if the lesion shows evidence of cartilage breakdown or subchondral bone fragmentation, it loses its mechanical support and may progress to further breakdown resulting in extrusion into the joint.16
The presentation of OCD of the knee is variable, and the symptomatology is in large part due to the stage of the lesion when the particular symptoms present.
A stable lesion which remains in situ may present as nonspecific knee pain that is poorly localized by the patient, externally rotated gait, and a possible effusion.29
A lesion that has progressed to instability may become a “trap door”-type lesion with mobility or a loose body. Both lesion types may present with mechanical symptoms that may be described as a “catching” or “locking” sensation.
In 1967, Wilson29 describes a clinical examination finding which he suggests is diagnostic of OCD of the knee: “[With the patient] in the supine position, the knee on the affected side is flexed through about 90° and the tibia is medially rotated. The knee is then gradually extended and at a point of about 30° short of full extension the [patient] will complain of pain over the anterior part of the medial femoral condyle. Lateral rotation of the tibia relieves this pain immediately.”
However, Wilson sign has been shown to be unreliable and nonspecific.8
Imaging protocols have received close attention in the literature as a result of the varied success of nonoperative treatment. The goals of imaging are to characterize the lesion, determine the prognosis of nonoperative management, and monitor the healing of the lesion.
Radiographs are useful for making the diagnosis of OCD and should be the first imaging modality of choice, as they usually characterize and localize the lesion and rule out other bony pathology of the knee region. In a significant number of cases, however, OCD lesions may not be readily apparent on plain radiographs.
Imaging workup begins with plain radiographs, including anteroposterior (AP), tunnel, and lateral views (FIG 2A-C).
A Merchant view should be included to best reveal any OCD lesions of the patella or trochlea.
MRI is most useful for determining the size of the lesion and the status of the cartilage and subchondral bone in addition to further characterizing the OCD lesions (FIG 2D-F).
The extent of bony edema, the presence of a high-signal zone beneath the fragment, and the presence of other loose bodies are also important findings on MRI. Arthroscopy continues to be the gold or reference standard for diagnosing stability.4
Scintigraphy and computed tomography (CT)
Although CT can better differentiate bone contour and congruency, this are rarely ordered especially in juvenile cases of OCD.
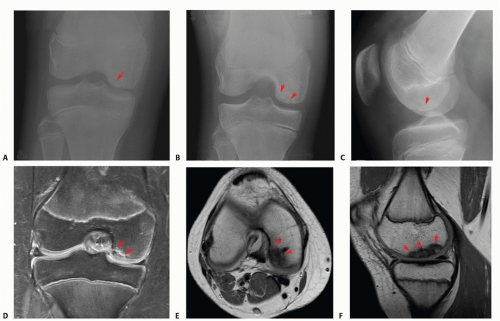
FIG 2 • Three-view series of OCD lesion: AP (A), tunnel view (B), and lateral view (C). MRI sequence of OCD: coronal (D), axial (E), and sagittal slice (F). Red arrows point to OCD lesion.
Similarly, technetium bone scans have been employed to provide information about the biologic capacity of an OCD lesion to heal. However, with the advent of MRI and its ability to be used without exposure to radiation yet still provide quality images of OCD lesions, scintigraphy is less commonly used.
Use of ionizing radiation in OCD lesions should be carefully considered, as other imaging options may provide excellent diagnostic and prognostic information with none or minimal exposure to radiation.
Irregular ossification
Acute osteochondral fractures
Meniscal injuries
An initial course of nonoperative management is the treatment of choice for skeletally immature children with small intact lesions with the goal of nonoperative intervention to promote healing in the subchondral bone and potentially prevent chondral collapse, subsequent fracture, and crater formation.
Controversy exists regarding the ideal nonoperative management for these patients. Clinicians who adhere to treating the subchondral bone as the primary source of pathology favor a period of immobilization. Those whose focus is on
the articular cartilage as a source of pathology tend to favor mobilization.
Table 1 Three-Phase Approach to Nonoperative Management of Skeletally Immature Osteochondritis Dissecans
Phase I (wk 1-6)
Knee immobilization in a hinged brace. The patient may walk with the hinged brace locked in extension. The brace may be unlocked to work on range of motion for 5 minutes five times per day.
Phase II (wk 6-12)
If the patient is pain-free and radiographs show signs of healing after 6 weeks, he or she is allowed to begin weight bearing without immobilization and to begin a physical therapy protocol to improve knee range of motion and quadriceps and hamstring strength.
Phase III* (wk 8-12)
Running, jumping, and cutting sports are permitted under close observation. High-impact activities and activities that might involve shear stress to the knee should be restricted until the child has been pain-free for several months and the radiographs show a healed lesion.
* This phase begins typically 3 months after treatment and is instituted if the patient continues to remain pain-free and shows radiographic evidence of healing.
The options for immobilization include casting, bracing, and standard knee immobilizers.
We recommend a three-phase approach to the nonoperative management of OCD lesions (Table 1).
The goals of operative treatment are to promote healing of the native articular cartilage and subchondral bone when possible, to maintain joint congruity, to rigidly fix unstable fragments, and to replace osteochondral defects with cells that can replace and grow cartilage.
It is widely accepted that operative treatment should be considered for patients with unstable or detached lesions and in patients whose lesions have not resolved with an appropriate period of nonoperative management, especially in those approaching skeletal maturity.
Operative treatment is recommended if one or more of the following conditions are met:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








