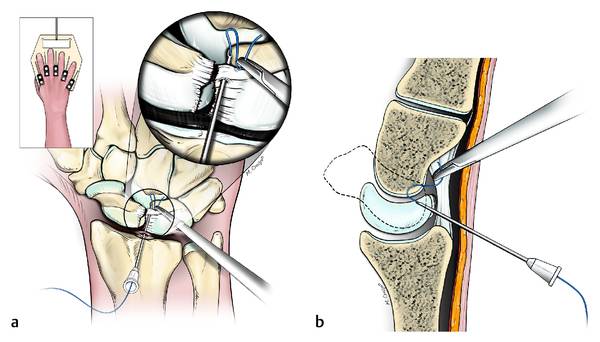
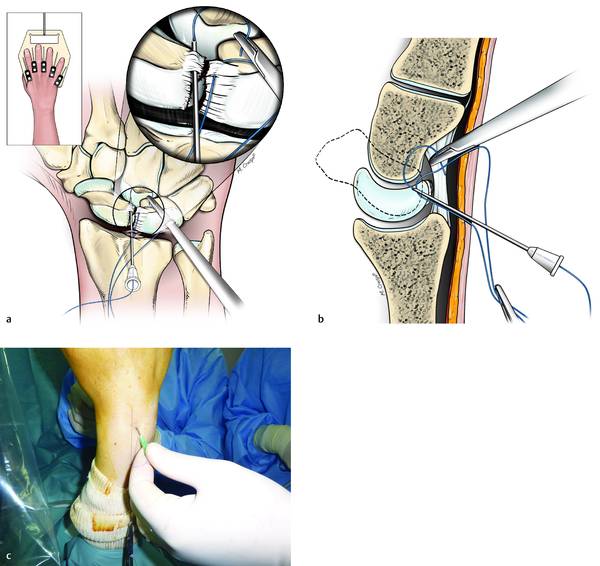
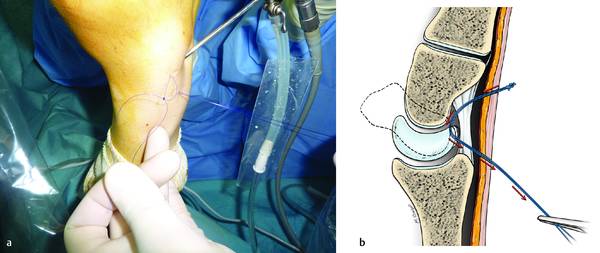
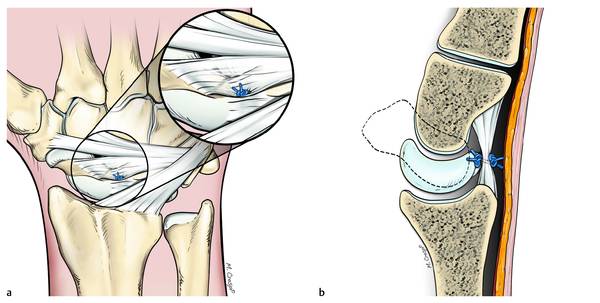
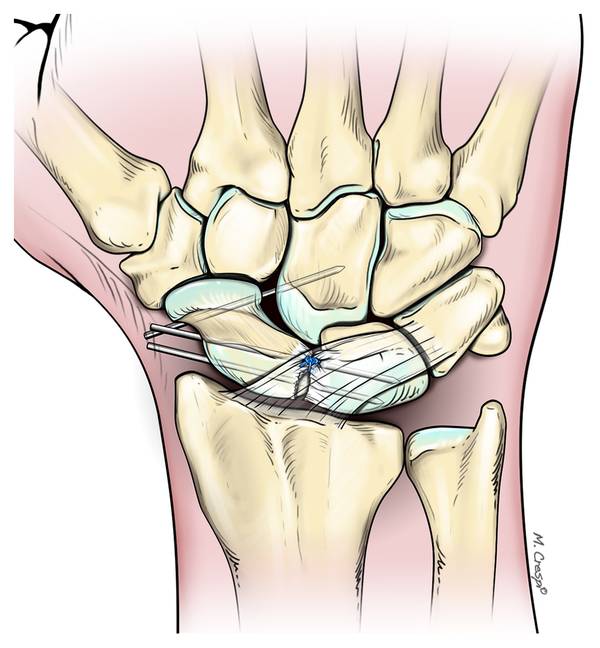
Arthroscopic Dorsal Capsuloligamentous Repair in the Treatment of Chronic Scapholunate Ligament Tears Scapholunate (SL) ligament injuries usually result from a fall on the outstretched hand. The natural history of untreated scapholunate instability remains controversial and usually results in late arthritic changes—the so-called scapholunate advanced collapse (SLAC) wrist. Arthroscopy is a valuable tool for the diagnosis and treatment of acute scapholunate dissociation. In chronic lesions, treatment options are more controversial than in the acute cases. In selected cases with reducible scapholunate instability (Garcia-Elias stages 2, 3, and 4) we propose a new “all-arthroscopic dorsal capsuloligamentous repair” with an added advantage of early rehabilitation and prevention of postoperative stiffness. Most forms of treatment recommended in the literature consist of an open repair or alternative reconstruction techniques that can improve pain and grip strength but very often lead to stiffness in the wrist joint.1 Furthermore, there is scant evidence that these interventions prevent, or at least delay, posttraumatic arthritis. Open techniques seem to result in some degree of wrist stiffness. This may be due to the extensive soft tissue dissection including the wrist capsule, which scars and contracts during the healing phase. We have therefore developed an all-arthroscopic dorsal capsuloligamentous repair technique to avoid open dissection of the wrist capsule.2 We use the Geissler and Haley3 arthroscopic classification and the Garcia-Elias et al4 classification to grade the scapholunate tear. We propose this technique in cases with a partial or complete scapholunate ligament (SLL) tear and with a well-aligned and reducible scaphoid. Additional stabilization of the scapholunate interval can be achieved with K-wires. Our series of 57 consecutive patients shows very encouraging preliminary results even in young, active individuals at a mean follow-up of more than 2 years. We report the results of our series of 57 consecutive patients suffering from chronic wrist pain refractory to conservative measures. All patients underwent a thorough clinical examination in addition to a standard set of radiographs and MRI examination; and they were treated by an all-arthroscopic dorsal capsuloligamentous repair under locoregional anesthesia on an ambulatory basis. All patients were available for follow-up at regular intervals during the postoperative period. At follow-up, the wrist range of movement (ROM) in all directions, the grip strength, Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire, and pain relief based on the Visual Analogue Scale (VAS) were recorded for both the operated and contralateral sides. Clinical assessment ROM on both sides was measured in all patients preoperatively. Tenderness on palpation in the affected wrist was noted and the Watson test was performed. Radiographic assessment Standard PA, lateral, and oblique radiographs were taken on all patients. The scapholunate gap and the scapholunate angles were measured. All patients also had an MR arthrogram. The procedures were performed on an outpatient basis under regional anesthesia and with an upper arm tourniquet. The elbow was flexed to 90° on an arm table and the hand was suspended by means of a hand holder with traction of 3 to 5 kg. We used the standard arthroscopic 3–4 and 6R portals for the radiocarpal joint and MCR and MCU for the midcarpal joint. The joints were first insufflated with normal saline. A small transverse incision was made with a no. 15 scalpel followed by blunt dissection with a mosquito forceps. The 2.4-mm arthroscope was introduced through the 3–4 portal and the instruments through the 6R portal—these two portals are interchangeable according to need. The midcarpal joint was explored through the MCU portal. Exploration and palpation of the structures in the two joints confirm the lesion and provide the staging. To evaluate the extent of scapholunate dissociation we used two classification systems, which stage cartilage status and the SLL lesion under arthroscopic vision. Geissler and Haley,3 described four stages of arthroscopic scapholunate lesions (▶ Table 16.1); and Garcia-Elias et al4 subdivided scapholunate dissociations into six different stages based on five clinical and arthroscopic criteria (▶ Table 16.2). Stage 1 Attenuation/hemorrhage SL in RCJ; no incongruency in MCJ Stage 2 Attenuation/perforation of SL in RCJ; small incongruency in MCJ Stage 3 Perforation of SL in RCJ/incongruency and step-off in MCJ (> probe) Stage 4 Incongruency and step-off in RCJ and MCJ: gross instability with manipulation Abbreviations: MCJ, midcarpal joint; RCJ, radiocarpal joint; SL, scapholunate. State of lesion Stage 1 2 3 4 5 6 Dorsal SLL intact? Yes No No No No No Repairable SLL? Yes Yes No No No No Scaphoid alignment normal? Yes Yes Yes Yes No No Carpal malalignment reducible? Yes Yes Yes Yes No No Cartilage in RCJ and MCJ normal? Yes Yes Yes Yes Yes No Abbreviations: MCJ, metacarpal joint; RCJ, radiocarpal joint; SLL, scapholunate ligament. Only Garcia-Elias stages 2, 3, and 4 were treated with this technique. The carpal alignment was noted as either being preserved (stages 2 and 3) or amenable to correction if malalignment was seen (stage 4). If the arthroscopic findings coincided with one of these three stages then the dorsal capsuloligamentous repair was carried out. Usually, the SLL is detached from the scaphoid and remains attached to the lunate, but on the dorsal aspect—close to the normal insertion of the SLL to the capsule—there are remnants of the SLL on both the dorsal horn of the lunate and the scaphoid. It is difficult to visualize the dorsal SLL (particularly its scaphoid portion) from a 6R portal because when the wrist is in traction, the dorsal capsule is apposed against the ruptured ligament. However, using correct triangulation with a 30° oblique scope in the 6R portal after releasing the traction allows for proper visualization of the torn ligament in this region. A needle is inserted under direct vision through the 3–4 radiocarpal portal into the radiocarpal joint. Care is taken not to directly enter the open part of the capsule. Needle is inserted through the dorsal capsule up to 1 mm from the capsular hole and then the needle is directed through the radial remnant of the SLL obliquely from dorsal to palmar and proximal to distal, with the tip of the needle seen in the midcarpal joint. The scope is then switched to the MCU portal and a 3.0 PDS suture is passed through the needle and pulled out through the MCR portal with a hemostat under direct vision from the MCU portal (▶ Fig. 16.1a, b). A second suture is then passed parallel to the first one in the lunate/ulnar remnant of SLL and brought out through the same portal (▶ Fig. 16.2a, b). A knot is tied between the two sutures. Following this, distal-to-proximal traction is applied to both proximal ends of the sutures in order to place the first knot into the mid-carpal joint between the scaphoid and the lunate, volar to the dorsal part of the SLL (▶ Fig. 16.3). A second knot is tied between the two proximal ends and introduced in the 3–4 portal incision, dorsal to the capsule. This knot lies outside the wrist joint on the dorsal capsule. The net effect of this achieves a capsuloligamentous repair between the SLL and the dorsal capsule overlying the ligament (▶ Fig. 16.4a, b). However, it must be borne in mind that if the SLL has been completely avulsed off the bone instead of being torn, and if there are no remnants, this procedure cannot be performed. Fig. 16.1 (a and b) Drawings representing the first step of the procedure. A strong suture is passed from the radiocarpal joint to the midcarpal joint, transfixing the portion of dorsal scapholunate ligament that has remains attached to the lunate. Fig. 16.2 (a–c) The second step of the procedure consists on passing another suture from the radiocarpal to the midcarpal joint, transfixing the remnant of scapholunate ligament attached to the scaphoid. Fig. 16.3 (a and b) Third step of the procedure: the distal end of the two sutures is tied, and the proximal end is tractioned in order to place the knot over the volar aspect of the two ligament remnants in the midcarpal joint space. Fig. 16.4 (a and b) Drawings representing front and side views of the second knot tied between the two proximal ends and introduced in the 3–4 portal incision, dorsal to the capsule. This knot lies outside the wrist joint on the dorsal capsule. The net effect of this achieves a capsuloplasty between the scapholunate ligament and the dorsal capsule overlying the ligament. The procedure for stage 4 cases is slightly different from that described previously. In such instances, the scaphoid must be reduced and stabilized with both the lunate and the capitate part of the SLL. This is done using external and internal maneuvers under fluoroscopic control. Once the reduction is confirmed then the capsuloligamentous repair can be performed. The scaphoid is stabilized with 1.2-mm parallel K-wires passed through the scaphoid into the capitate. The final dorsal knot is made after SL stabilization and fixation with K-wires (▶ Fig. 16.5). The radiocarpal and midcarpal joints are thoroughly lavaged before instrument retrieval. The portal incisions are not sutured. A bulky dressing and a simple volar splint are applied upon completion of the surgery. Fig. 16.5 Drawing representing the front view of the stabilization of the scaphoid with 1.2-mm parallel K-wires applied through the scaphoid into the capitate, used only in stage 4 according to the Garcia-Elias staging. The final dorsal knot was performed after SL fixation.
16.1 Introduction
16.2 Materials and Methods
16.3 Preoperative Assessment
16.4 Operative Technique
16.5 Intraoperative Staging
16.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








