Stage I
Small, subchondral compression of the bone
Stage II
Partial detachment of the fragment from the chondral surface
Stage III
Complete fragment detachment with no displacement
Stage IV
Total detachment of fragment with displacement
4.2 Clinical Evaluation and Diagnosis
The presenting signs and symptoms of osteochondral lesions of the talus can be vague and nonspecific, unless a trauma has recently occurred.
Clinically, there can be a low-grade persistent ankle pain after an ankle sprain. The patient may also describe swelling, catching, clicking, locking and, occasionally, giving way.
On physical examination, lateral or medial tenderness can be present, associated with reduced range of motion and instability of ankle joint [7].
The diagnosis of an osteochondral lesion of the talus can be delayed because plain radiographs often appear normal or only slightly altered. The real onset of symptoms ranges between 4 months and 2 years, as the ankle may appear completely normal during the inspection. For this reason, the diagnosis of this kind of injury requires a high index of suspicion [7].
Recent advances in diagnostic and operative arthroscopy have resulted in new techniques that allow for improved management of osteochondral lesions of the talus.
In addition to plain radiographs, more detailed studies include computer tomography (CT) scans, magnetic resonance imaging (MRI) studies and direct arthroscopy of the ankle.
CT is useful in determining the site, size, location, shape and degree of displacement of osteochondral fragments; still it does not give a good visualization of cartilage or bone bruises.
MRI assesses both articular cartilage and subchondral bony lesions, as well as evaluates surrounding soft tissue abnormalities.
MR arthrography has recently been considered a valuable choice for an accurate visualization of cartilage lesions, especially if compared with standard MR imaging. In 2003, Schmid et al. [8] examined both MR arthrography and CT for the evaluation of cartilage lesions in the ankle joint. They outlined CT superiority in the assessment of hyaline cartilage for being more sensitive than MR arthrography (when detecting articular cartilage lesions).
It has been suggested that plain radiographs should be the initial evaluation in patients presenting acute ankle injuries. Any detected lesion should be evaluated with CT to research more details. In cases with persistent ankle pain despite normal plain radiographs, an MRI may be helpful [3].
4.3 Treatment Options
There is a wide variety of management strategies for osteochondral lesions of the talus. They range from nonsurgical to biological repair and cartilage regeneration.
Management decisions should be based on symptoms, on size (>1,5 cm) and on the grade of the lesion [3].
4.3.1 Surgical Treatment
It is reserved for lesions that fail to respond to conservative measures, but it is also appropriate for patients with unstable lesions and mechanical symptoms: in this case, a long period of conservative management is not recommended, as there is little hope for spontaneous improvement.
Surgical options include excision with or without fibrocartilage growth stimulation techniques, such as microfracture, curettage, abrasion or transarticular drilling.
If a fragment is large enough, it could be reattached to the talar dome through retrograde drilling, bone grafting or internal fixation, using screws and pins [9], bone pegs [10] or Kirschner wires. The results are fairly good, although this is one of the most invasive techniques.
Other options include cancellous bone grafting and osteochondral transplantation through osteochondral autografts, allografts or cell culture [3].
In 1999, Kumai et al. [11] reported excellent outcomes after arthroscopic drilling in 18 patients. The same year, Taranow et al. [12] first described the retrograde drilling, effective when a subchondral cyst is present or when the lesion is hard to reach with the usual anteromedial and anterolateral portals. Anterograde drilling can also be effective (Figs. 4.1 and 4.2).
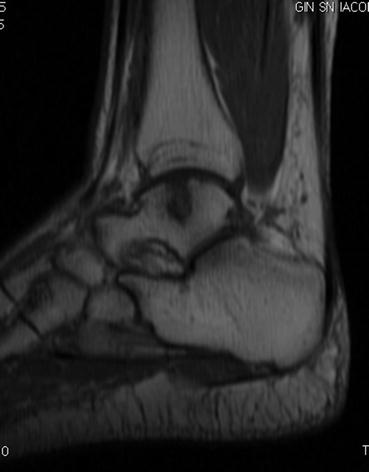

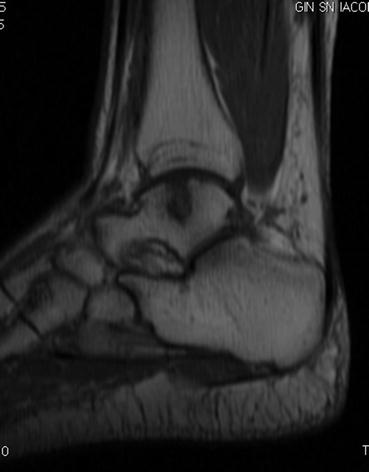
Fig. 4.1
Talar osteochondral lesion with cystic degeneration

Fig. 4.2
MRI 2 months later. Asymptomatic patient after 6 months (AOFAS score evaluation: 100)
In 2002, Schuman et al. [13] reported 82 % good to excellent results in 38 patients after arthroscopic curettage and drilling.
4.3.1.1 Debridement, Microfracture and Drilling
These procedures are reserved for completely detached talar osteochondral lesions that are not amenable by internal fixation.
Human articular cartilage has a limited reparative capability due to its avascularity. To address this problem, arthroscopic techniques have been developed to stimulate bone marrow reparative properties, including drilling and microfractures [14].
These techniques promote the development of a fibrocartilaginous formation over the defect, as frequently occurs in the case of small lesions.
The principal goal consists in breaching the subchondral plate at multiple intervals to stimulate chondroprogenitor cells of the bone marrow into the lesion site; the release of fatty drops from the new fractures provides a clinical indicator that the depth of the microfracture is adequate. This procedure stimulates the formation of fibrin clots and subsequently fibrocartilage (type I collagen) in the defect.
The technique is supplemented by excision and curettage of the damaged tissue for better results [14].
It is well documented that arthroscopic excision, curettage and bone marrow stimulation should be the first treatment of choice for primary osteochondral talar lesions: this procedure is relatively inexpensive; there is low morbidity, a quick recovery and a high success rate [1].
The best indications for bone marrow stimulation techniques are a lesion smaller than 1,5 cm2 with frayed cartilage, primary surgery, patients younger than 50 years old, a traumatic etiology, lateral lesions and low body mass index.
When advanced fraying of the lesion is present, whether or not the lesion is stable, curettage is indicated and can be eventually combined with penetration of the subchondral bone.
Microfracturing and microdrilling are mini-invasive techniques which require a short period of hospitalization, avoiding risks of thermal damage with easier access to the defects without more invasive steps such as transtibial drilling or osteotomy of the medial malleolus [15].
Drilling, first introduced by Pridie in 1959, was used for decades before microfractures were advocated in the 1990s [16]. These two techniques are thought to be very similar; nevertheless, some differences exist. Chen et al. were the first to compare microfractures (MF) to microdrilling (MD): in particular, they compared acute osteochondral characteristics 24 h after MF or MD procedures in a rabbit model. They found that MF produced a more compact bone around holes than MD did, avoiding marrow cells to reach the new holes and thus limiting the repairing process. On the other hand, MD did not produce the expected heat necrosis: this result was reached using a properly thin drill bit under cooled irrigation [16].
For Takao [17], arthroscopic drilling is less invasive than microfractures. It must be said that no reports of long-term follow-up results have been published yet; therefore, the incidence and degree of complications are not clear.
On the other hand, a disadvantage of the microfracture technique is that the repaired cartilage is fibrous, with inferior mechanical qualities when compared to hyaline cartilage, and it can often degenerate eventually causing osteoarthritis [18].
For this reason, if the cartilage is intact, a retrograde drilling of the subchondral bone without damaging the overlying cartilage can be considered [19].
Retrograde drilling was first described in 1999 by Taranow et al.: it avoids removal of healthy articular cartilage [12]. It has been reported that there is often no difference in functional outcomes between the transmalleolar and retrograde drilling. However, retrograde drilling avoids damage to healthy articular structures [20].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







