CHAPTER 29 Arthroscopic Debridement for Isolated Scaphotrapeziotrapezoid Arthritis
Introduction
Degenerative changes of the scaphotrapeziotrapezoid (STT) joint are seen in almost 40% of cadaveric wrists.1 Clinical involvement of the triscaphe joint occurs in 15 to 30% of wrists.2 Concomitant trapeziometacarpal arthritis occurs in the majority of patients, but isolated pathology is present in up to 20% of the population3,4—particularly in postmenopausal women.5 Symptomatically isolated STT disease leads to tenderness over the palmar aspect of the thenar eminence and is an important differential diagnosis in radial wrist pain. Frequently, flexor carpi radialis tendinitis and radiopalmar ganglia are also noted upon examination.6
Previous reports of treatment for STT osteoarthritis (OA) following failed conservative treatment include excisional arthroplasty (with7 or without4 a silicone spacer) and limited wrist fusion, including STT fusion.6 Pain relief is not uniform in these series, and morbidity due to postoperative complications has been noted. Wrist arthroscopy is a useful tool for visualizing articular damage, which can be a source of chronic wrist pain.8 Arthroscopic debridement has proven to be an effective method of achieving pain relief in the knee in two-thirds of patients for up to two to five years and carries a low morbidity.9,10 The authors have successfully used arthroscopic debridement of isolated STT arthritis to improve symptoms in selected patients.
The pain associated with STT arthritis can be surprisingly debilitating and leads to disability when axially loading the thumb during strong pinch and key turning. There are, however, other patients who have minimal symptoms. For example, the patient with a distal radius fracture will often have advanced STT joint arthritis on radiographs but will deny any symptoms. Watson and Ottoni11 suggested rotatory subluxation of the scaphoid as a possible cause of isolated STT arthritis. They noted that early degenerative changes of the STT joint occurred when abnormal unilateral hypermobility of the scaphoid was present. STT arthrodesis has been the traditionally recommended procedure and is noted to give good function and excellent pain relief.6 STT fusion, however, disturbs the usual wrist mechanics—which results in a high incidence of STT nonunion and secondary radial styloid arthritis due to impingement.
Arthroscopy in the Treatment of Arthritis
Arthroscopic debridement and washout remains a popular treatment method for degenerative arthritis in the knee.9,10 Considerable pain relief is noted in a third of patients, lasting into the medium term. Further surgical intervention is required in only a small proportion of those treated. The use of arthroscopy allows for joint assessment and therapeutic interventions.
We had previously treated patients with STT OA with either an excisional arthroplasty consisting of a distal scaphoid pole resection as described by Garcia-Elias et al.4 or STT joint arthrodesis using the technique reported by Watson and Hempton.12 Two of the excisional arthroplasty patients complained of persistent symptoms, and plain radiographs demonstrated increased extension of the scaphoid and the lunate. Some of the patients treated with an STT joint arthrodesis had continuing pain at sites of nonunion. We therefore searched for alternative methods of achieving good pain relief and function without the potential morbidity ensuing from the traditional techniques used to treat STT arthritis. It was felt that the arthroscopy had potential use for joint debridement and joint excision.
It is the authors’ experience that the degenerative changes noted at the time of arthroscopy are more advanced than those reported in recent cadaveric studies.13 This is probably because all patients who require therapeutic intervention have significant pain associated with advanced degenerative osteoarthritis. Moritomo et al. have noted that the most common site of degenerative changes is on the ulnar side of the distal scaphoid and centrally on the trapezoid and trapezium.1 Half of cases have involvement of the trapezoid alone, with the trapezium being involved in only a third.
Patient Selection
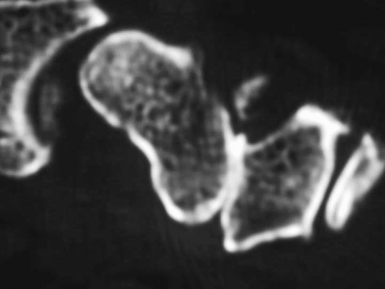
Radiographs showed joint narrowing and osteophyte formation isolated to the STT joint (Figure 29.1). Longitudinal computer tomography (CT) scans were performed, particularly if thumb carpometacarpal (CMC) joint arthritis was suspected (Figure 29.2).14 The thumb CMC joint pain can also be isolated with a diagnostic injection. Typically, the CT scans demonstrated complete loss of the joint space—which was often associated with osteophytes and degenerative cysts within the distal scaphoid. The scaphoid was always extended and the plain radiograph often showed dorsal instability of the lunate.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree