Arthroscopic Débridement for Elbow Degenerative Joint Disease
Julie E. Adams
Scott P. Steinmann
DEFINITION
Patients with primary osteoarthritis of the elbow are frequently manual laborers, athletes, and those who rely on wheelchairs or crutches for ambulation.4,15,18,21
Although total elbow arthroplasty provides pain relief and improved range of motion in patients with inflammatory arthritis and/or those with low demands, use in young active patients has been associated with early loosening and is undesirable in this group. Likewise, elbow arthrodesis is undesirable to many patients who do not wish to sacrifice motion in favor of pain relief.8
Arthroscopic procedures have gained acceptance with patients and surgeons in part due to perceived benefits of a minimally invasive nature and better visualization of the joint.
Several series confirm results at least equivalent to open procedures, with similar complication rates.
ANATOMY
At the elbow, the coronoid fossa anteriorly, the trochlea, and the olecranon fossa posteriorly articulate with the coronoid and olecranon. Bony osteophytes may develop, leading to impingement in flexion and extension in the setting of degenerative conditions.
PATHOGENESIS
Three main pathologic processes are involved in primary elbow arthritis. Loss and fragmentation of cartilage lead to loose body formation. Osteophytes arise from reactive bone formation. Presence of impinging bone spurs and a thickened and contracted capsule lead to joint stiffness.21,22
Symptoms include loss of terminal flexion and extension, pain at the end points of motion, and mechanical symptoms such as catching or locking.4,9
NATURAL HISTORY
The natural history is one of slowly progressive joint contracture and discomfort. Ulnar neuritis may develop.
PATIENT HISTORY AND PHYSICAL FINDINGS
The typical patient is a middle-aged male laborer with a painful dominant elbow, worse with use.
Less frequently, patients who depend on wheelchairs or crutches for mobility, and who thus put increased forces across their elbow joints, may be afflicted.
Progressive loss of motion and pain at the extremes of motion due to impingement of osteophytes are noted.
Painful crepitus and catching or locking sensations may be noted with range of motion. Usually, pain in the mid-arc of motion is absent.
Patients with contracture of the posterior capsule will lack flexion, whereas those with anterior contractures of the capsule will lack extension.
Not infrequently, ulnar nerve irritation is noted. This should be documented and will contribute to decision making regarding the surgical approach and the need for decompression or transposition.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Usually, plain film radiographs, clinical examination, and history are sufficient to make the diagnosis (FIG 1).
Radiographs may show joint space narrowing, hypertrophic bony osteophytes, loose bodies, and subchondral sclerosis typical of osteoarthritis.
Computed tomography scans with two-dimensional (2-D) and 3-D reconstructions are especially helpful for evaluation of the bony anatomy of the elbow and for preoperative planning.
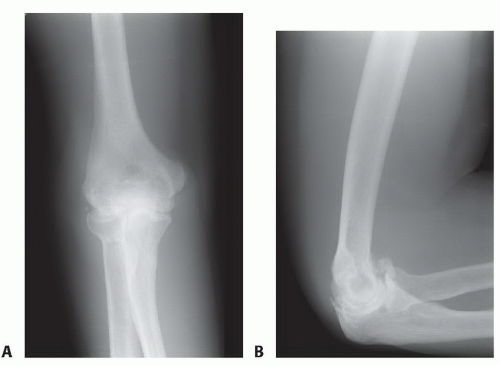 FIG 1 • Anteroposterior (A) and lateral (B) radiographs of the typical patient with degenerative arthritis of the elbow. Bony osteophytes are noted with loose body formation. |
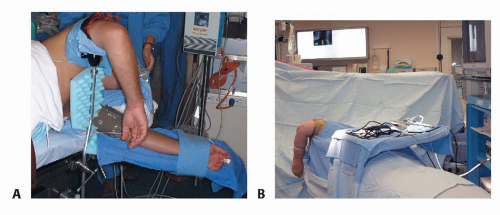 FIG 2 • A. The patient is positioned laterally with the arm secured in a dedicated arm holder. B. Operative setup.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





