and C. Niek van Dijk3
(1)
Human Anatomy and Embriology Unit, Laboratory of Arthroscopic and Surgical Anatomy, Department of Pathology and Experimental Therapeutics, School of Medicine, University of Barcelona, Barcelona, Spain
(2)
Department of Orthopaedic Surgery, School of Medicine, University of Pittsburgh, Pittsburgh, PA, USA
(3)
Department of Orthopedic Surgery, Academic Medical Centre, University of Amsterdam, Amsterdam, The Netherlands
Abstract
With the introduction of arthroscopy, we learned to avoid the anatomy. Knowledge of the anatomy however is mandatory for any surgical procedure. This chapter provides the anatomical basis for correct portal placement. It also contains a detailed description of the ligaments of the ankle.
With the introduction of arthroscopy, we learned to avoid the anatomy.
Knowledge of the anatomy is mandatory for any surgical procedure.
3.1 Introduction
Any operative intervention consists of two elements: the approach and the actual procedure itself. The actual procedure can be practiced on sawbones, but the approach is mostly practiced on patients (Amis et al. 2010). The learning curve for the approach is steep. In the past, surgeons made wide exposures and thus practiced their anatomical skills on a day-to-day basis. With the introduction of minimally invasive and arthroscopic surgery, we learned to avoid the extra-articular anatomy. We go straight to the bone and feel comfortable once inside a joint. Our incisions for open procedures get smaller and smaller. The patients like it if their surgical scars are small, but our knowledge of the anatomy thus gets more and more forgotten. Our knowledge dates from anatomy books but anatomy books are not specifically designed for surgical approaches.
A session in the cadaver lab can be really helpful to refresh our memories of the surgical anatomy approaches. It is important to know “what is around the corner” especially in cases where an extended or unusual approach is needed. Foot and ankle surgeons who do not have access to anatomy specimens will find it useful to study the detailed pictures in this chapter. These pictures can serve as a guide for approaches to the structures, how to identify them, how to avoid trouble, and how to understand their functional significance.
3.2 Ankle Joint
The talocrural or ankle joint is formed by the articular surfaces of the tibial and fibular distal epiphyses and the talus in its superior, lateral, and medial aspects (Figs. 3.1 and 3.2). The morphology of these surfaces forms a hinge-type synovial joint with a single axis of movement: the bimalleolar axis. The bimalleolar axis allows dorsiflexion (flexion) and plantar flexion (extension) of the ankle and foot in the sagittal plane. Because of this configuration and the fact that the ankle is a load-bearing joint, the interarticular space is narrow, making insertion of arthroscopic instruments between the articular surfaces difficult. Hence, articular distraction systems are required to perform complete arthroscopic inspection of the joint (Golanó et al. 2006a).

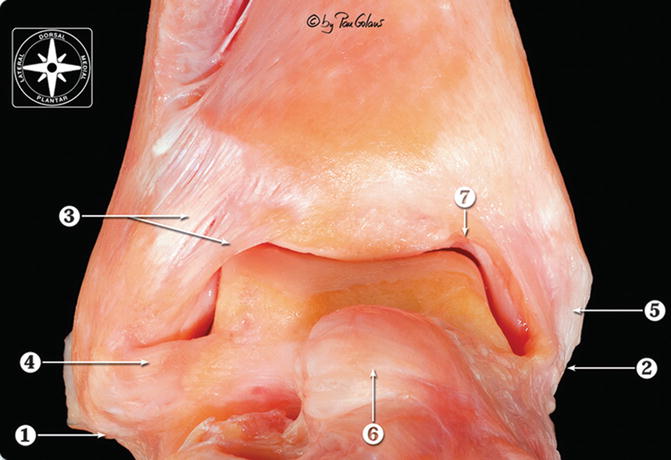

Fig. 3.1
The bones and articular surfaces forming the talocrural or ankle joint. The articular surfaces were painted digitally (Adobe Photoshop) (With kind permission of © Pau Golanó 2013)
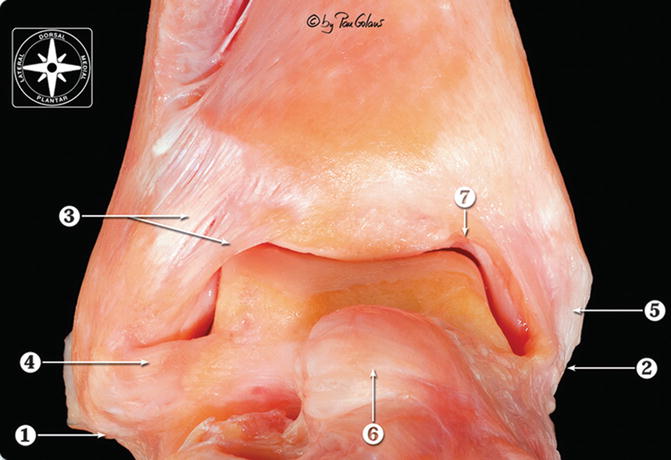
Fig. 3.2
Anterior view of the ankle joint showing the typically hinge-type synovial joint morphology of the ankle joint. 1 Lateral malleolus (tip), 2 medial malleolus (tip), 3 anterior tibiofibular ligament, 4 anterior talofibular ligament, 5 medial collateral ligament, 6 head of the talus (dorsal talonavicular ligament), 7 notch of Harty (With kind permission of © Pau Golanó 2013)
On the other hand, the ankle joint capsule is similar to the capsule of any other joint, but with the exception of a singular characteristic: the anterior capsular insertion in the tibia and talus occurs at a distance from the cartilaginous layer. The distance is approximately 6–8 mm in the tibia and 8–10 mm in the talus (Testut and Latarjet 1985). In a recent study, the distance was found to be 4.3 mm (0.5–9.0 mm) and 2.4 mm (1.8–3.3 mm) in the tibia and talus, respectively (Tol and van Dijk 2004). This peculiarity determines the existence of a substantial anterior capsular recess that allows the arthroscopist to encounter an anterior working area. Nevertheless, the size of this area depends on the position of the foot. When the foot is in dorsiflexion, the capsular recess is evident, whereas when it is in plantar flexion, capsular tension makes the recess smaller (Figs. 3.3, 3.4, 3.5, 3.6, and 3.7). Hence, van Dijk recommended that treatment of anterior ankle pathology should be done with the joint in dorsiflexion: “the anterior working area is opened up and a bony or soft tissue impediment in front of the malleolus, at the talar neck or at the distal tibia can be visualised and treated.” Similarly, when distraction is used, the tension in the articular capsule is increased and applied to the bone ends, reducing the working area (van Dijk 2001).
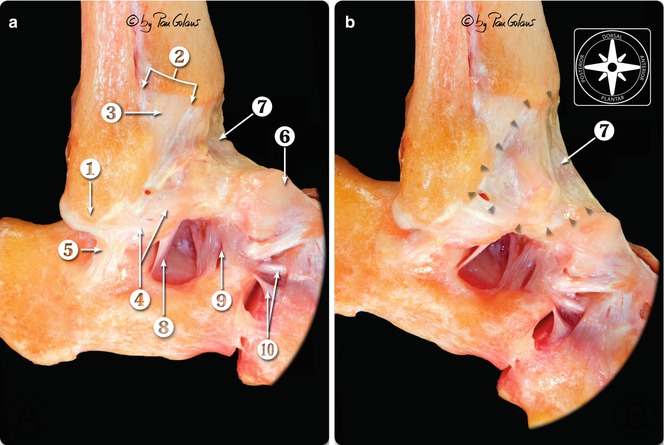
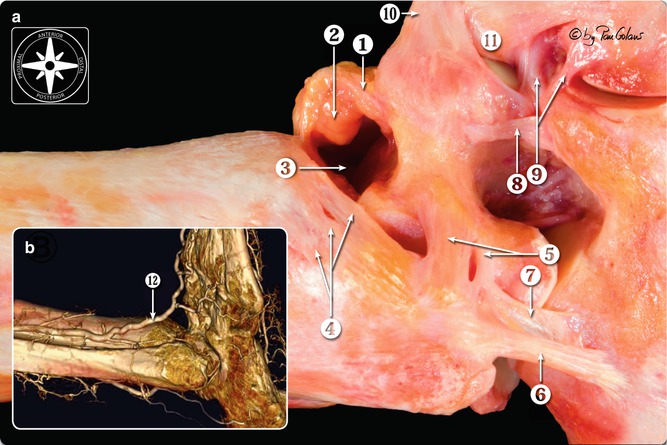
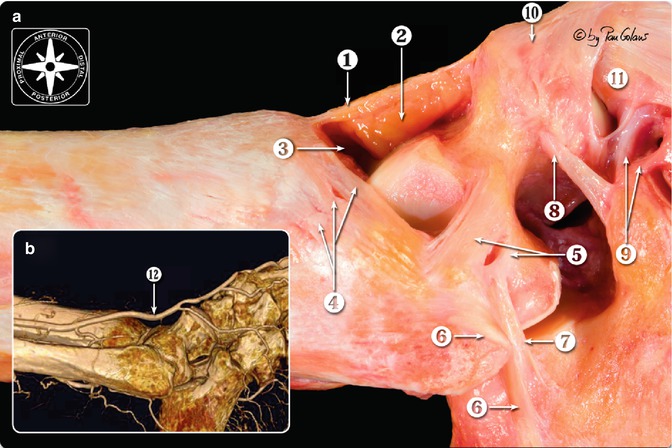
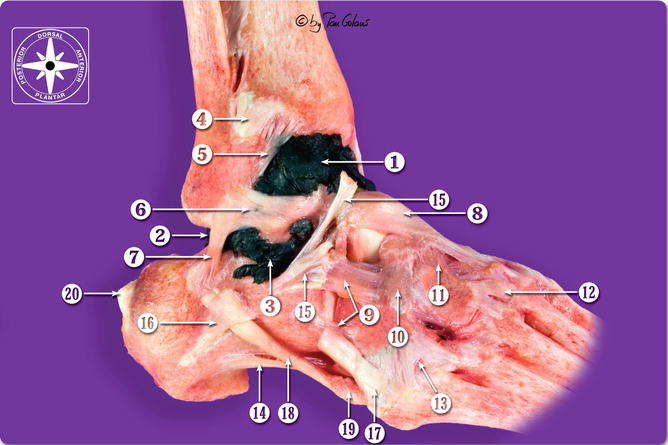
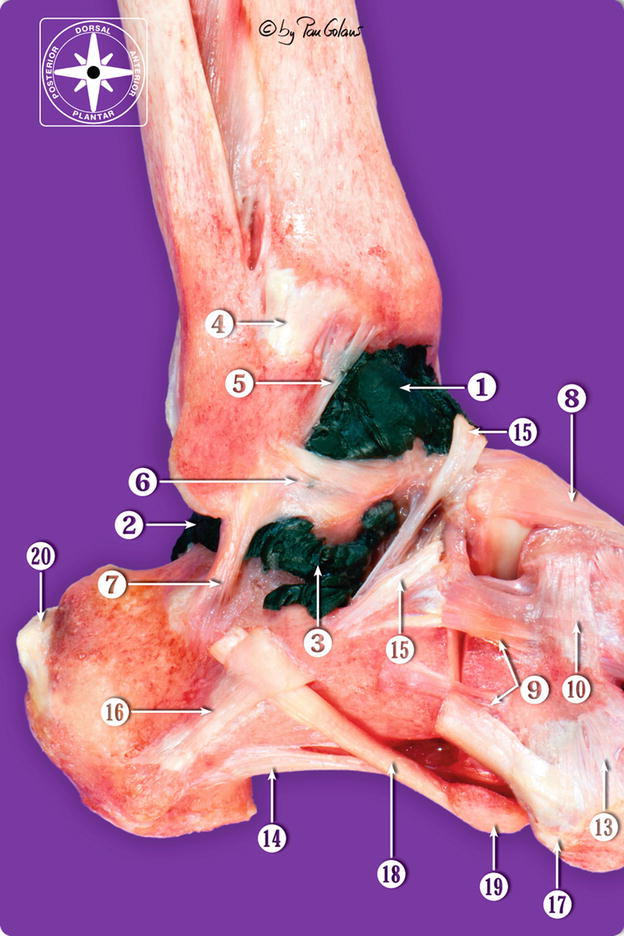
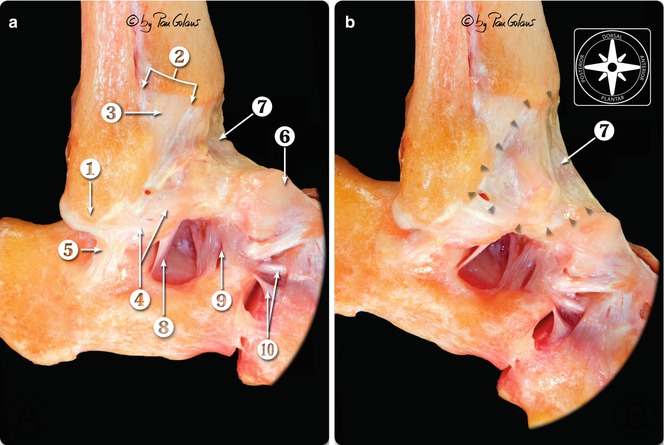
Fig. 3.3
Anterolateral view of the osteoarticular layer of the foot and ankle joint. The capsule of the ankle joint was maintained in order to observe changes in tension during ankle movements and their insertion sites (arrowheads). (a) Dorsiflexion (the capsule is relaxed. Following to joint distension, the capsule can form a capsular recess: the anterior working area is opened up). (b) Plantar flexion (the tension in the articular capsule is increased and applied to the bone ends, reducing the working area). 1 Lateral malleolus (tip), 2 anterior tubercle of the tibia, 3 anterior tibiofibular ligament, 4 anterior talofibular ligament (two bands), 5 calcaneofibular ligament, 6 dorsal talonavicular ligament, 7 ankle articular capsule, 8 talocalcaneal interosseous ligament, 9 cervical ligament, 10 bifurcate ligament (With kind permission of © Pau Golanó 2013)
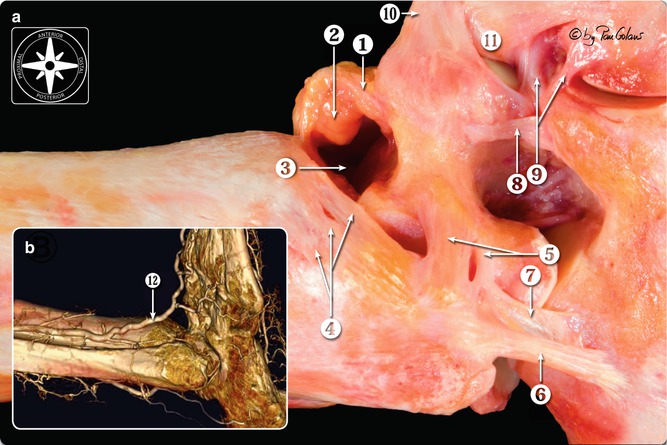
Fig. 3.4
Lateral view of osteoarticular dissection of the ankle. The ankle was placed similar to the patient’s position during anterior ankle arthroscopy. The capsule was opened to observe the intra-articular but extra-articular fat pad of the ankle joint (comparable to Hoffa fat pad of the knee). (a) Dorsiflexion. The anterior working area is opened up; (b) dorsiflexion. Cadaveric CT reconstruction of foot and ankle arterial system. In ankle dorsiflexion the anterior neurovascular bundle moves away anteriorly from the ankle joint. These pictures 4 and 5 beautifully show the increase distance to the neurovascular bundle which lies just anterior to the capsule. 1 Ankle articular capsule, 2 fat pad, 3 anterior working area, 4 anterior tibiofibular ligament, 5 anterior talofibular ligament, 6 calcaneofibular ligament, 7 lateral talocalcaneal ligament, 8 cervical ligament, 9 bifurcate ligament, 10 dorsal talonavicular ligament, 11 os naviculare, 12 anterior tibial artery/dorsalis pedis artery (With kind permission of © Pau Golanó 2013)
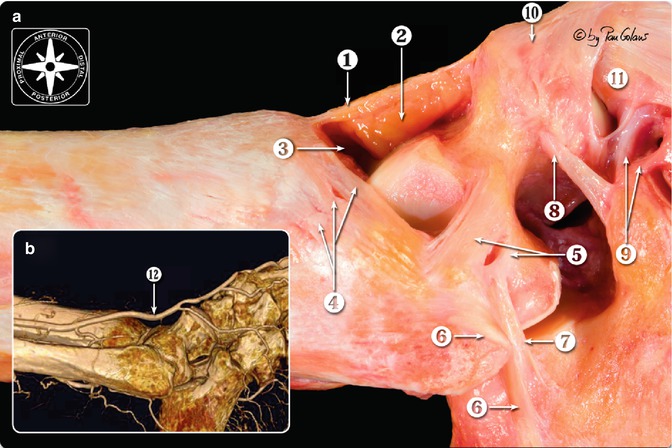
Fig. 3.5
Lateral view of osteoarticular dissection of the ankle. The ankle was similarly situated to the patient’s position during anterior ankle arthroscopy. The capsule was opened to observe the intra-articular but extra-articular fat pad of the ankle joint (comparable to Hoffa fat pad of the knee). (a) Plantar flexion. Similarly, when distraction is used, the tension in the articular capsule is increased and applied to the bone ends, reducing the working area. (b) Plantar flexion. Cadaveric CT reconstruction of foot and ankle arterial system. In plantar flexion the anterior neurovascular bundle is pulled tight towards the joint, thereby decreasing the safe anterior working area. 1 Ankle articular capsule, 2 fat pad, 3 anterior working area, 4 anterior tibiofibular ligament, 5 anterior talofibular ligament, 6 calcaneofibular ligament, 7 lateral talocalcaneal ligament, 8 cervical ligament, 9 bifurcate ligament, 10 dorsal talonavicular ligament, 11 os naviculare, 12 anterior tibial artery/dorsalis pedis artery (With kind permission of © Pau Golanó 2013)
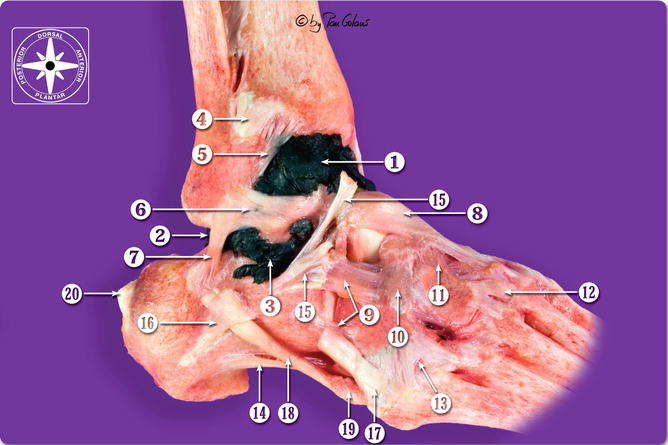
Fig. 3.6
Anterolateral view of osteoarticular dissection of the foot and ankle. The synovial cavity of the ankle joint was filled with black latex. 1 Anterior articular recess, 2 posterior articular recess, 3 posterior subtalar recess, 4 anterior tibiofibular ligament, 5 distal fascicle of the anterior tibiofibular ligament, 6 anterior talofibular ligament, 7 calcaneofibular ligament, 8 dorsal talonavicular ligament, 9 dorsolateral calcaneocuboid ligament, 10 dorsal cuboideonavicular ligament, 11 dorsal cuneonavicular ligament, 12 dorsal tarsometatarsal ligament, 13 dorsal tarsometatarsal ligament, 14 long plantar ligament, 15 inferior extensor retinaculum (cut), 16 inferior peroneal retinaculum, 17 peroneus brevis tendon (cut), 18 peroneus longus tendon (cut), 19 os peroneum, 20 calcaneal tendon (cut) (With kind permission of © Pau Golanó 2013)
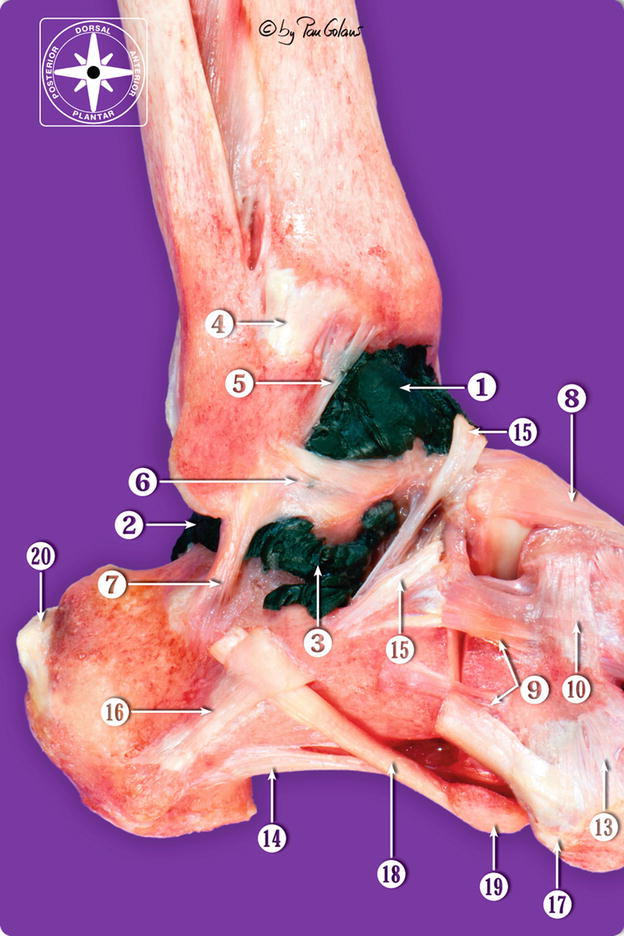
Fig. 3.7
Lateral view of osteoarticular dissection of the foot and ankle. The synovial cavity of the ankle joint was filled with black latex. Same numbering as in Fig. 3.6 (With kind permission of © Pau Golanó 2013)
If we transfer these concepts to the posterior compartment and to the use of the standard posterolateral portal, there are some differences. In contrast to what occurs with the anterior portal, the posterior articular recess is smaller, and the presence of structures that reinforce the capsule, such as the posterior intermalleolar ligament, converts it into multiple small recesses, making interarticular positioning of the arthroscope or instrumentation difficult in the posterolateral portal. In addition, when a distraction system is applied, capsular tension reduces the working space even more (Golanó et al. 2006a).
3.3 Landmarks
The anatomical landmarks of bone and tissue in the ankle joint are easily palpated and can be delimited on the patient’s skin with a dermographic marker. Landmarks are important for proper positioning of the portals and facilitate orientation during the procedure despite the edema associated with the technique (Golanó et al. 2006a). The following landmarks are the most important (Fig. 3.8): (1) both malleoli (lateral and medial); (2) the anterior joint line, which is easily palpated by moving the joint in dorsiflexion-plantar flexion and located approximately 2 cm proximal to the tip of the lateral malleolus and 1 cm proximal to the tip of the medial malleolus; (3) the tibialis anterior tendon, peroneus tertius tendon, and Achilles tendon; (4) vascular landmarks such as the great saphenous vein, which runs in front of the medial malleolus; and (5) neural structures such as the superficial peroneal nerve with its dividing branches—the medial and intermediate dorsal cutaneous nerves. This nerve is easily identified in thin patients when inversion of the foot is performed (Fig. 3.9). Other neural structures such as the sural nerve, which usually runs 2 cm posterior and distal to the lateral malleolus, together with the small saphenous vein, are also easily palpated (Ferkel 1996).
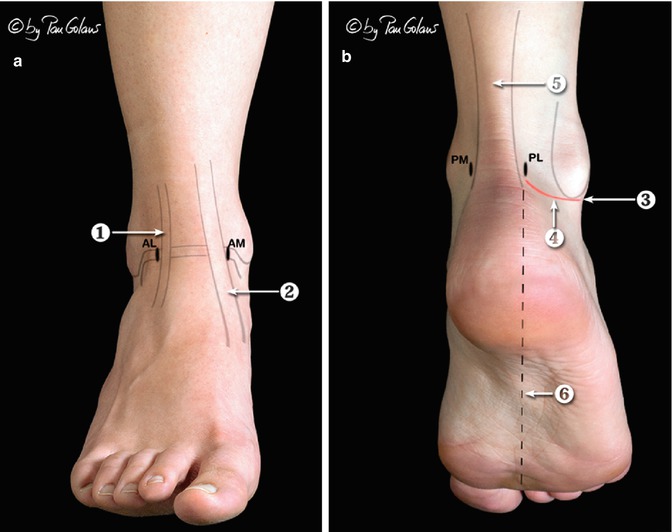
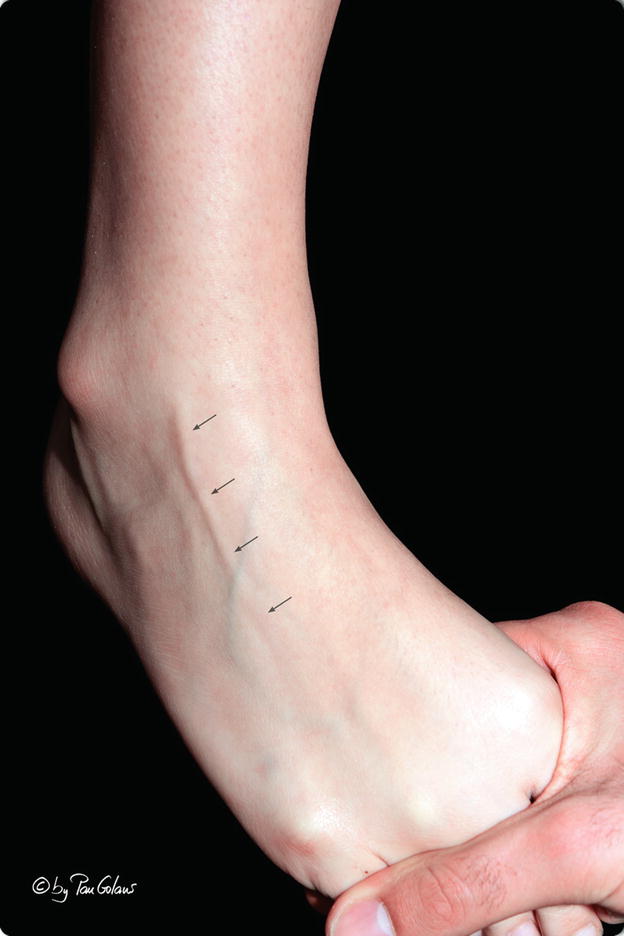
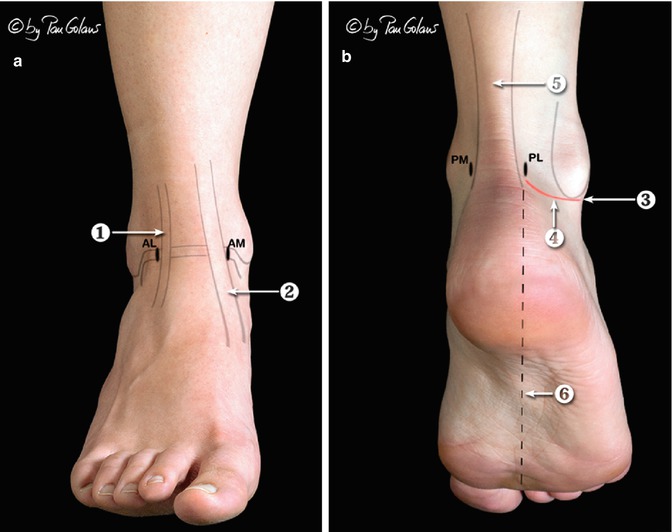
Fig. 3.8
Cutaneous landmarks. (a) Anterior view of the ankle in dorsiflexion; (b) posterior view of the ankle in supine position. AL anterolateral portal, AM anteromedial portal, PL posterolateral portal, PM posteromedial portal, 1 peroneus tertius tendon, 2 tibialis anterior tendon, 3 tip of the lateral malleolus, 4 PL portal incision level, 5 calcaneal tendon, 6 PL portal direction of the web space between the first and second toe (With kind permission of © Pau Golanó 2013)
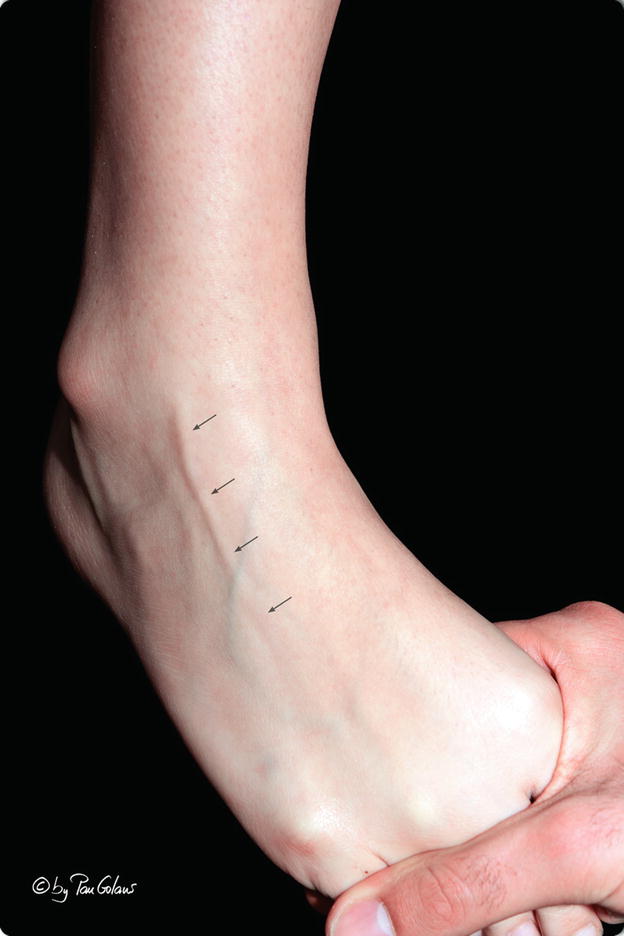
Fig. 3.9
Visible subcutaneous course of the superficial peroneal nerve (intermediate dorsal cutaneous branch) indicated with arrows on clinical examination by performing inversion of the foot and ankle (With kind permission of © Pau Golanó 2013)
3.4 Arthroscopic Portals
The numerous arthroscopic portals described for the ankle can be grouped into anterior, posterior, transmalleolar, and transtalar. The use of some of these portals involves considerable technical difficulty or an elevated potential for neurovascular lesion, and for these reasons, they have fallen into disuse.
The first description of the anteromedial, anterolateral, and posterior portals of the ankle was reported by Watanabe in 1972. In later years, investigators such as Ikehuchi (1977), Chen (1976), Drez et al. (1981, 1982), Parisien et al. (1987), and Andrews et al. (1985) described additional portals and the extra-articular and intra-articular anatomy of the ankle. Subsequently, several investigators described new portals to fill the need to access specific regions of the joint, particularly the central and posterior areas (Acevedo et al. 2000; Buckingham et al. 1997; Mandrino et al. 1994; Sim et al. 2006; van Dijk et al. 2000; Voto et al. 1989; Wang et al. 2007; Woo et al. 2010). This need also led to the development of various systems of distraction to allow a more complete visualization of the ankle joint (Aydin et al. 2006; Beals et al. 2010; Cameron 1997; Casteleyn and Handelberg 1993, 1995; Guhl 1988; Hedley et al. 2001; Kumar and Satku 1994; Miyamoto et al. 2008; Resch 1993; Sartoretti et al. 1996; Trager et al. 1989; van Dijk 2001; Waseem and Barrie 2002; Yates and Grana 1988).
Owing to the fact that all the portals run through an anatomical region surrounded by numerous neurovascular structures susceptible to injury, several anatomical studies to assess the potential for lesion to each of them have been published (Basarir et al. 2007; Feiwell and Frey 1993; Lijoi et al. 2002; Lijoi et al. 2003; Ögüt et al. 2004; Saito and Kikuchi 1998; Sitler et al. 2002; Solomon et al. 2006; Takao et al. 1998; Tryfonidis et al. 2008; Voto et al. 1989).
3.4.1 Anterior Portals
3.4.1.1 Anteromedial Portal
The anteromedial portal is the first to be performed. It is established just medial to the tibialis anterior tendon at the anterior joint line of the ankle and coinciding with a soft spot, a visible and palpable depression seen when the ankle is in dorsiflexion (Figs. 3.10 and 3.11). It is important to palpate the tibialis anterior tendon with the ankle in the dorsiflexed position. There is a potential for injury to the saphenous nerve and the great saphenous vein, which at this level, divides into numerous branches that communicate with the deep venous system (Fig. 3.12). These structures lie at a mean safe distance of 9 mm (3–16 mm) from the saphenous vein and 7.4 mm (0–17 mm) from the saphenous nerve (Feiwell and Frey 1993). Although some investigators consider these structures risk-free (Saito and Kikuchi 1998), Chen reported one case of saphenous vein lesion in 67 ankles treated with arthroscopy (Chen 1976); Ferkel and Fischer described 27 neurologic complications, 5 corresponding to saphenous nerve injuries (Ferkel and Fischer 1989); and Zengerink and van Dijk reported two cases in a large series of 1,305 arthroscopies (Zengerink and van Dijk 2012).
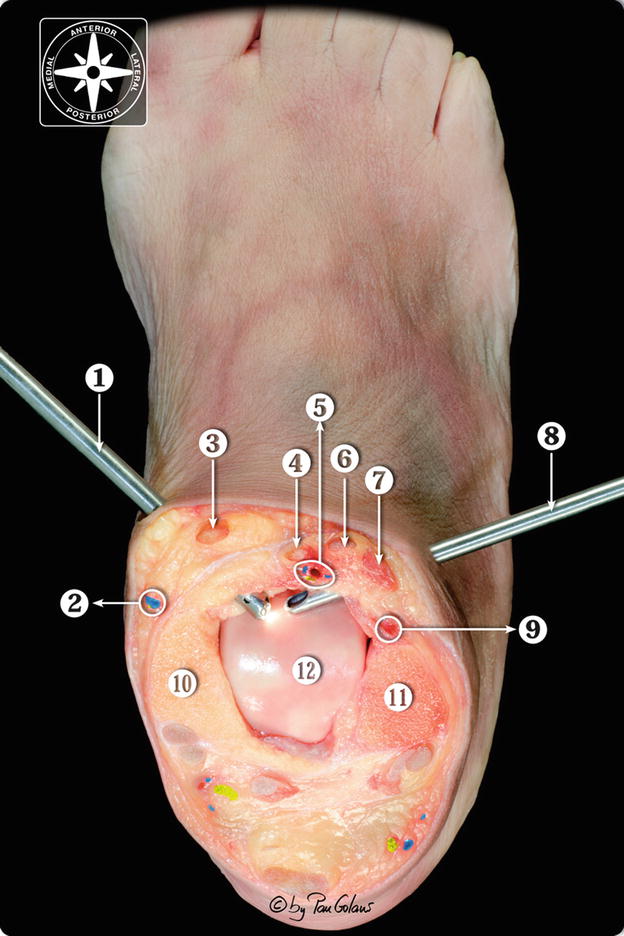
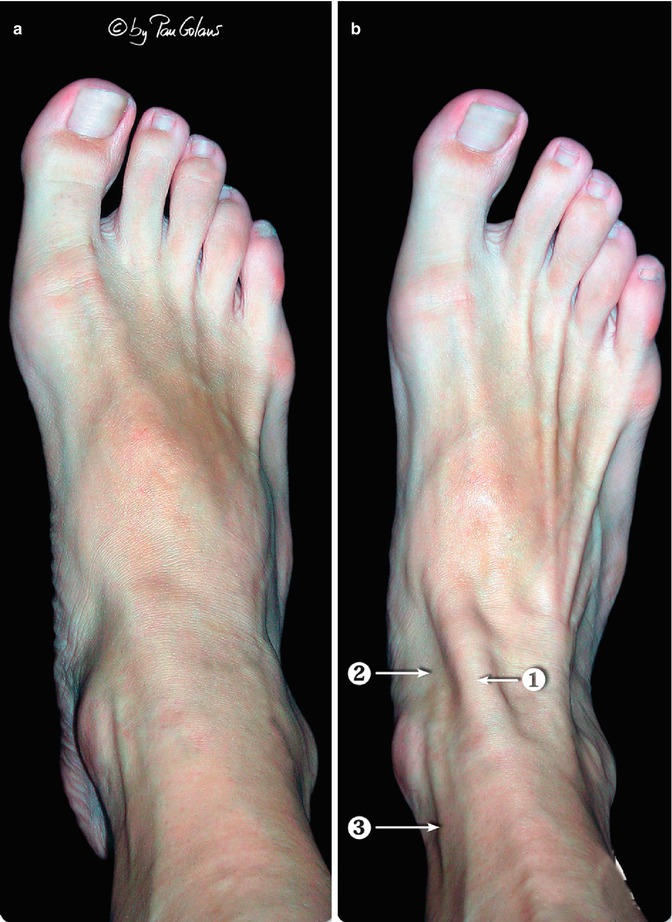
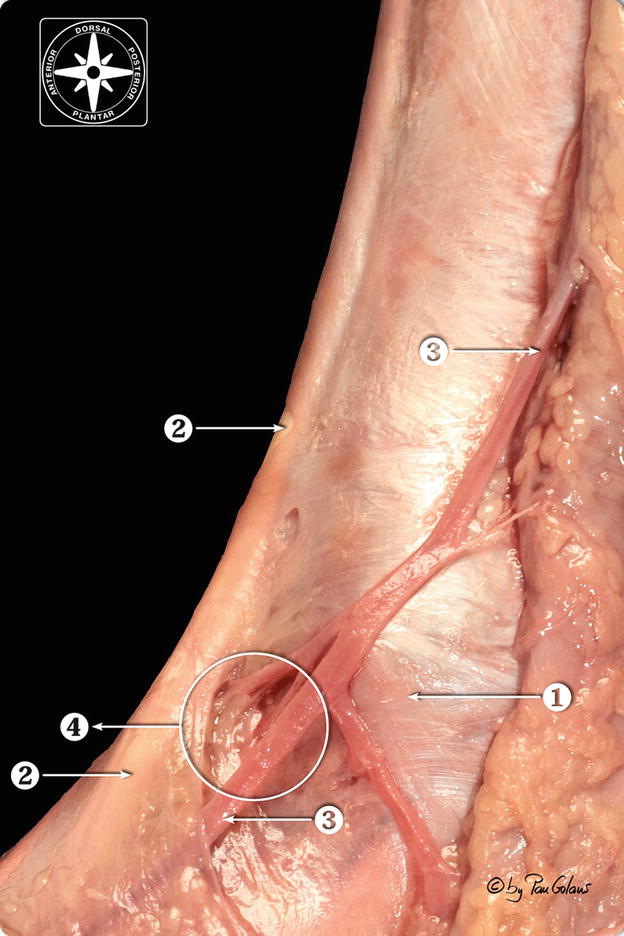
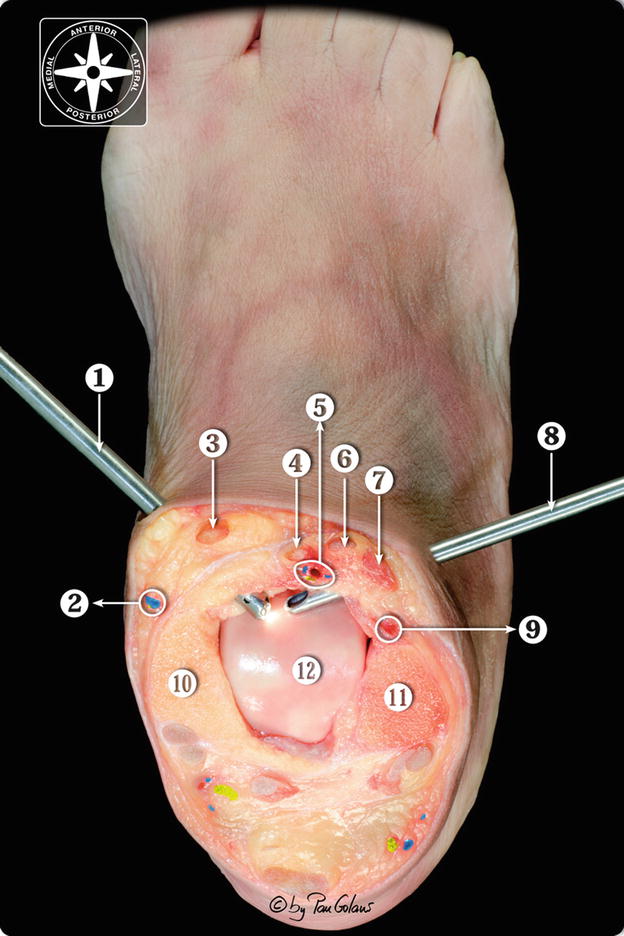
Fig. 3.10
Transversal section at the level of the ankle joint showing the anatomical relations of the anterior portals. The AM an AL portals were performed before the section. The nerves and vessels were painted digitally (Adobe Photoshop). 1 Anteromedial portal, 2 saphenous nerve and great saphenous vein, 3 tibialis anterior tendon, 4 extensor hallucis longus tendon, 5 anterior neurovascular bundle (deep peroneal nerve, anterior tibial artery and veins), 6 extensor digitorum longus tendon, 7 peroneus tertius muscle belly, 8 anterolateral portal, 9 anterior peroneal artery, 10 medial malleolus, 11 lateral malleolus, 12 dorsal articular surface of the talus (With kind permission of © Pau Golanó 2013)
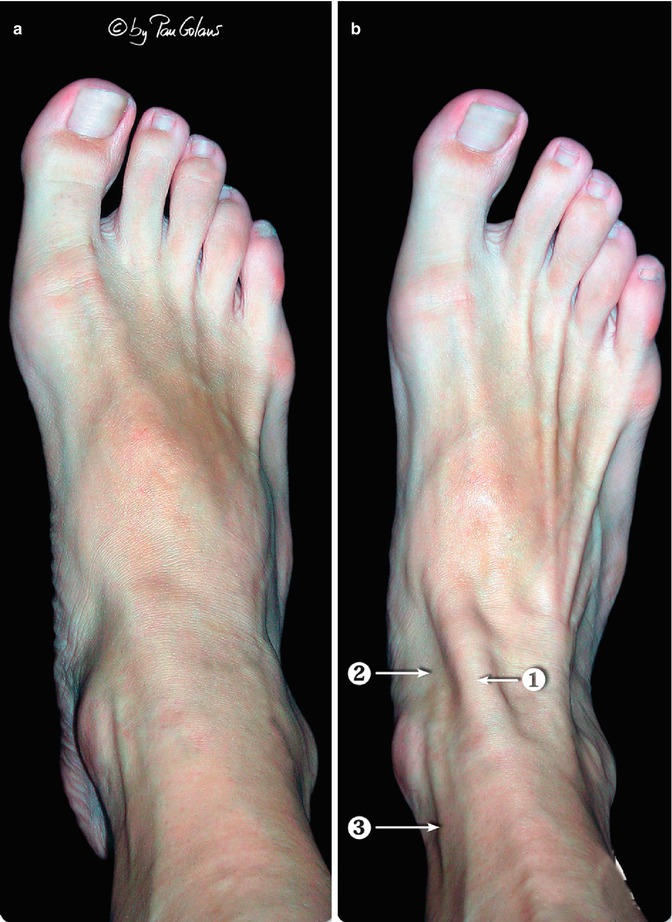
Fig. 3.11
The soft spot performed on the anteromedial portal is visible depending on the position of the ankle. (a) Plantar flexion. In plantar flexion the tibialis anterior tendon is in tension and the soft spot is less visible and palpable; (b) dorsal flexion. The tibialis anterior tendon is relaxed. A visible and palpable depression can be observed. Also, the tibialis posterior tendon can easily be displaced in the lateral direction, obtaining a more centrally portal in the joint and facilitating intra-articular visualization; 1 tibialis anterior tendon, 2 soft spot, 3 great saphenous vein (With kind permission of © Pau Golanó 2013)
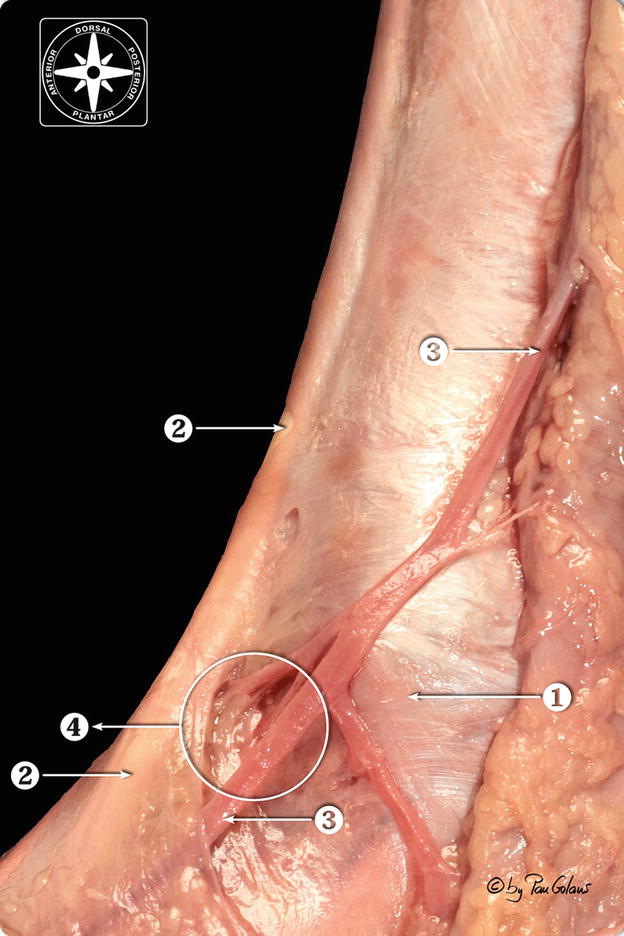
Fig. 3.12
Medial view of the ankle joint at the level of the anteromedial portal soft spot. 1 Medial malleolus (tip), 2 tibialis anterior tendon, 3 great saphenous vein and communicans branches, 4 soft spot area (With kind permission of © Pau Golanó 2013)
At the anterior edge of the tibia, where it joins with the medial malleolus, there is a notch (medial notch of Harty) (Harty 1985) that provides the anteromedial portal with additional space to allow easier passage of the instruments in the anteroposterior direction (Guhl 1993) (Fig. 3.13).
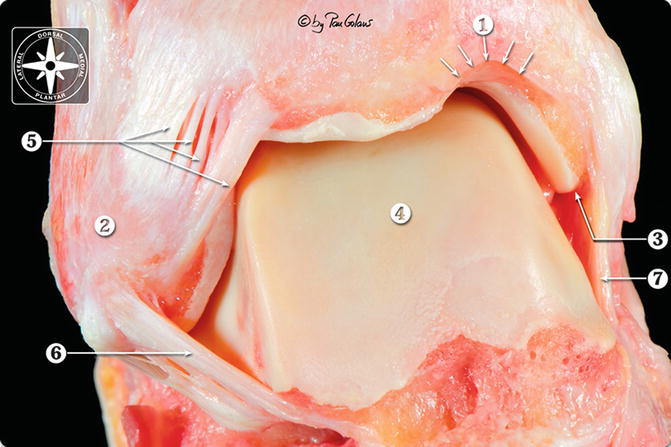
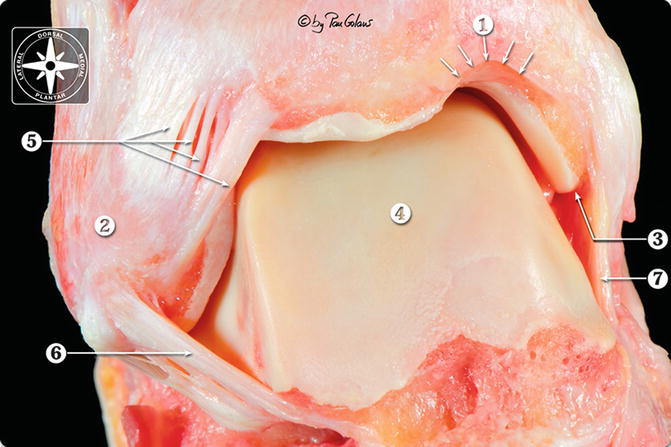
Fig. 3.13
Anterior superior lateral view of the osteoarticular dissection of the ankle joint. 1 Notch of Harty (arrows) at the anterior edge of the tibia, where it joins the medial malleolus, 2 lateral malleolus, 3 medial malleolus (tip), 4 dorsal articular surface of the talus, 5 anterior tibiofibular ligament, 6 anterior talofibular ligament, 7 medial collateral ligament (With kind permission of © Pau Golanó 2013)
3.4.1.2 Anterolateral Portal
The anterolateral portal is created at the anterior joint line just lateral to the peroneus tertius tendon (present in 90 % of cases) (Reinmann 1981) or, in its absence, lateral to the extensor digitorum longus tendons (Figs. 3.10 and 3.14). The main structure at risk of injury when performing this portal is the intermediate dorsal cutaneous nerve (the lateral branch of the superficial peroneal nerve) (Takao et al. 2001). Most of the complications described in arthroscopy of the ankle involve this nerve (Barber et al. 1990; Ferkel et al. 1996; Martin et al. 1989; Zengerink and van Dijk 2012) (Fig. 3.15).
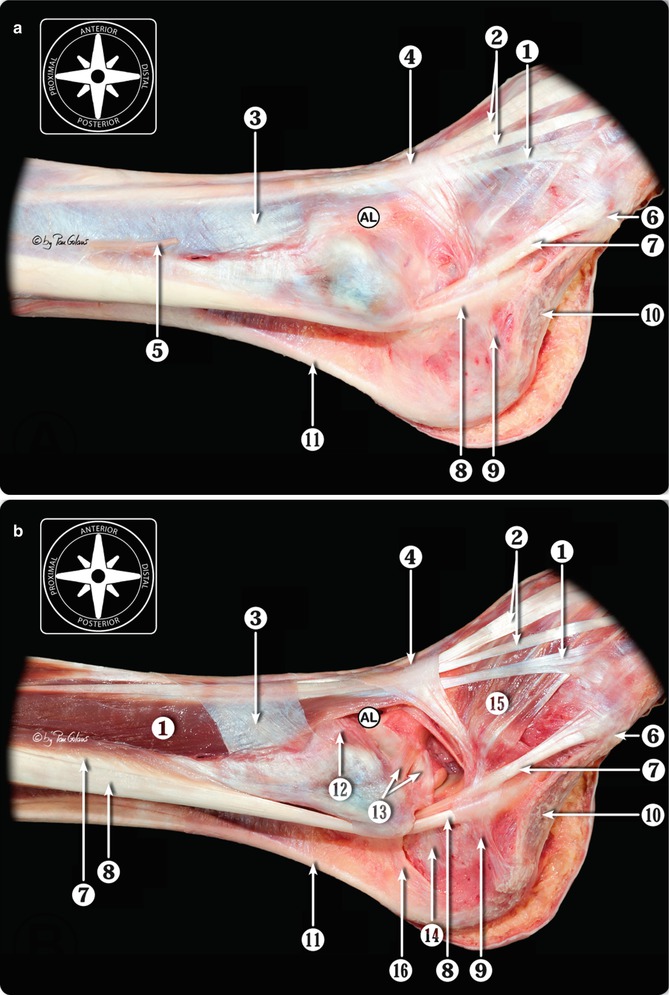
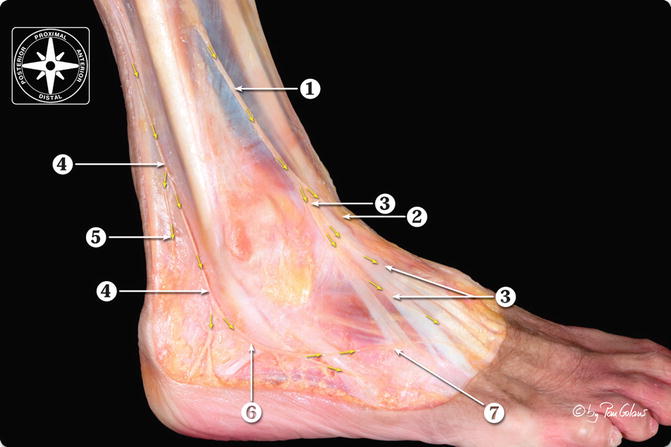
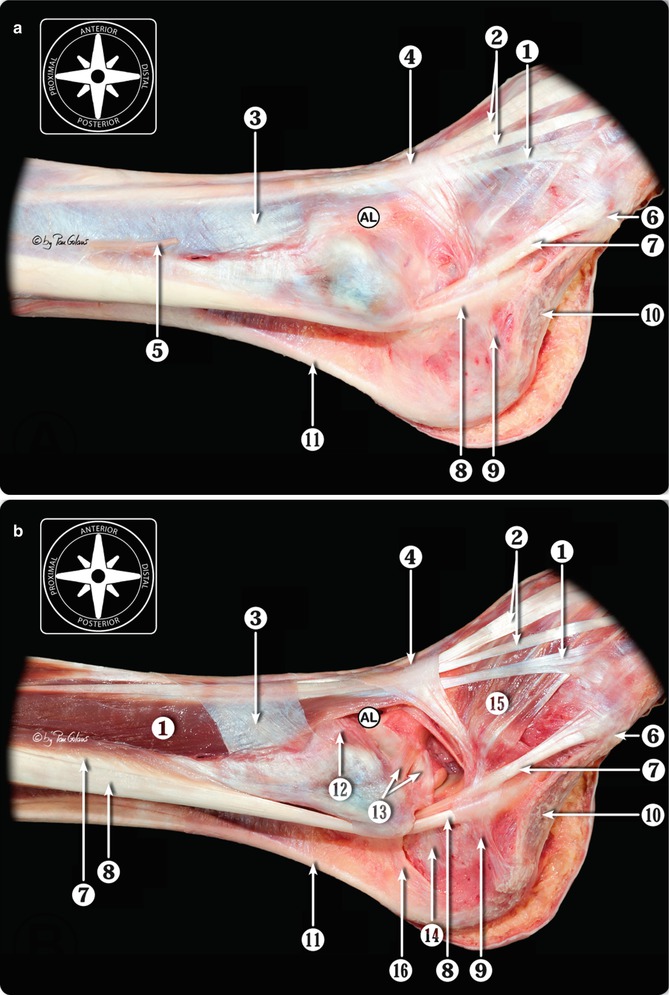
Fig. 3.14
Anatomical relations of the anterolateral portal (AL). (a) Fascial layer; (b) muscular layer; 1 peroneus tertius tendon and muscle belly, 2 extensor digitorum longus tendons, 3 superior extensor retinaculum, 4 inferior extensor retinaculum, 5 superficial peroneal nerve (cut), 6 tuberosity of the fifth metatarsal bone, 7 peroneus brevis muscle and tendon, 8 peroneus longus muscle and tendon, 9 inferior peroneal retinaculum, 10 abductor digiti minimi muscle and lateral component of plantar fascia, 11 calcaneal tendon, 12 anterior tibiofibular ligament, 13 anterior talofibular ligament (two bands), 14 calcaneofibular ligament (calcaneal insertion), 15 extensor digitorum brevis muscle belly, 16 superior peroneal retinaculum (With kind permission of © Pau Golanó 2013)
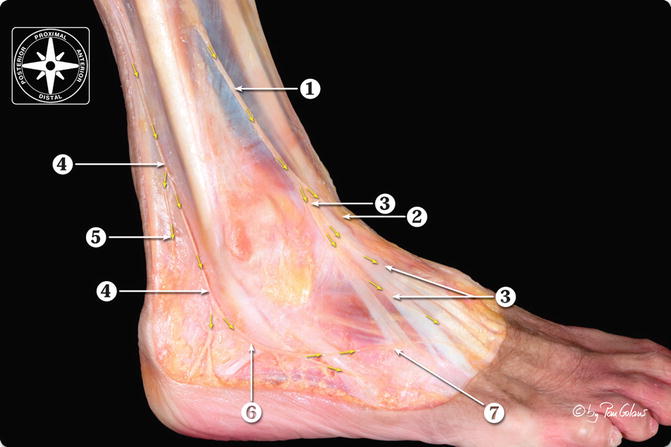
Fig. 3.15
Anatomical dissection of the cutaneous nerves at the dorsum of the foot. 1 Superficial peroneal nerve, 2 medial dorsal cutaneous nerve, 3 intermediate dorsal cutaneous nerve, 4 sural nerve, 5 lateral calcaneal branch, 6 lateral dorsal cutaneous nerve (terminal branch of sural nerve), 7 communication between intermediate and lateral dorsal cutaneous nerve (With kind permission of © Pau Golanó 2013)
The superficial peroneal nerve, which is the motor for the muscles of the lateral compartment of the leg (peroneus longus and peroneus brevis) and the sensory nerve for the greater part of the dorsal foot, has been the subject of numerous anatomical studies (Adkison et al. 1991; Blair and Botte 1994; Feiwell and Frey 1993; Ögüt et al. 2004; Saito and Kikuchi 1998; Sayli et al. 1998; Takao et al. 1998). After providing motor innervation, the superficial peroneal nerve runs along the lateral intermuscular septum. The superficial peroneal nerve usually divides into two branches: the more laterally located, the intermediate dorsal cutaneous nerve and the medial dorsal cutaneous nerve (Fig. 3.14). Various types or patterns have been described according to the level and manner in which the superficial peroneal nerve divides into its branches (Adkison et al. 1991; Blair and Botte 1994; Saito and Kikuchi 1998; Sayli et al. 1998; Takao et al. 1998).
The arthroscopist should be aware that this important nerve lies very close to the anterolateral portal and that a protocolled arthroscopic technique can avoid injury to this structure.
It is fortunate that this nerve is visible on clinical examination (it is the only nerve in the body that can be seen in this way) (Stephens and Kelly 2000). By performing inversion of the ankle, the nerve is tensed (particularly the intermediate dorsal cutaneous branch), and its subcutaneous course becomes evident (Ferkel 1996). De Leeuw et al. reported that the superficial peroneal nerve moves in a lateral direction in relation to the skin when the ankle is moved back from this inverted position to the neutral position. This movement is mean 3.6 mm to the lateral side. It is therefore important to stay on the medial side of the cutaneous nerve marking, performed in inversion of the ankle (de Leeuw et al. 2010).
A vertical incision affecting only the skin, together with blunt dissection up to the capsule, contributes to decreasing the risk of injury to the nerve. The anterolateral portal can also be created by an inside-out technique through the anteromedial portal, similar to the way the anterior portal is made in arthroscopy of the shoulder. Cutaneous transillumination obtained in this manner allows localization of the superficial peroneal nerve (intermediate dorsal cutaneous nerve) (Ferkel et al. 1996; Barber et al. 1988).
3.4.1.3 Medial Midline Portal
The medial midline portal, with the aim of obtaining an interarticular view similar to the anterocentral portal, but with a lower risk of lesion to vital structures, was first described by Buckingham et al. (1997).
The anterocentral portal is established between the extensor digitorum longus tendons at the level of the joint line. This portal provides a wide field of view and facilitates passage of the instruments in the anteroposterior direction (Guhl 1988). Nevertheless, most investigators discourage the use of this portal because there is a high associated risk of injury to numerous neurovascular structures, and today is an unused portal.
The medial midline portal is located just lateral to the tibialis anterior tendon, between the tibialis anterior and the extensor hallucis longus tendon, which is located medial to the portal.
This approach can also be used to introduce fluid into the joint.
3.4.1.4 Accessory Portals
Additional portals can be performed distal to the anterolateral and anteromedial portals. The separation between the main portal and the accessory portal should be wide enough to allow proper triangulation and instrumentation and to avoid the risk of cutaneous necrosis (around 5 mm).
These portals can facilitate the instrumentation in certain cases or can be used to introduce fluid into the joint.
3.4.2 Posterior Portals
3.4.2.1 Posterolateral Portal in Combination with Anterior Portals
The standard posterolateral in combination with anterior portals is the most widely used of the posterior portals because it presents the lowest risk of neurovascular injury. It is located 1.2–2.5 cm proximal to the tip of the lateral malleolus, adjacent to the lateral axis of the calcaneal or Achilles tendon (Ferkel 1996). The sural nerve and its branches and the small saphenous vein are in close proximity and at risk of injury (Ferkel et al. 1996; Guhl 1988; Martin et al. 1989). Ferkel et al. reported five cases of sural nerve lesion in 612 arthroscopic procedures of the ankle (Ferkel et al. 1996). According to Feiwell and Frey, the sural nerve is located at a mean distance of 6 mm (0–12 mm) and the small saphenous vein at 9.5 mm (2–18 mm) from the posterolateral portal (Feiwell and Frey 1993).
This portal is usually made with an outside-in technique. It is also possible to use an inside-out technique for this purpose (Katchis and Smith 1997), but considerable articular distraction is required to overcome the difference in positioning of the two joint lines, necessary for anteroposterior passage of the instruments.
In any case, after meticulous anatomical study of the posterior ligaments of the ankle joint (Golanó et al. 2002) and having performed and observed numerous arthroscopic procedures in this articulation, the authors concluded that the posterolateral portal is always established between two posterior ligaments of the ankle joint—the transverse ligament and the posterior intermalleolar ligament—which are constant and visible by arthroscopy. In dorsiflexion, the arrangement of these ligaments, together with the tibia, delimits a triangular area, with the base at the tibia and the tip at the lateral malleolus (Golanó et al. 2002). This space is similar to the anatomical intra-articular triangle of the shoulder used as a landmark to safely establish the anterior portal, as described by Matthews et al. (1985).
3.4.2.2 Posterior Endoscopic Portals
Even though numerous portals for accessing the ankle joint have been described and there are several available systems of distraction, the morphology of the joint makes access to the posterior region from the anterior portals difficult.
For this reason and with the aim of resolving treatment of periarticular pathology, van Dijk et al. described two posterior endoscopic portals that allow better access to the posterior aspect of the ankle and the subtalar joints (van Dijk et al. 2000).
To use these portals, the patient must be in the prone position. By means of this technique, it is possible to inspect and treat lesions in the posterior part of the ankle joint and pathology in the subtalar joint.
The posterolateral portal is created at the same level as or slightly above the tip of the lateral malleolus, just lateral to the calcaneal tendon. A blunt dissection is performed with a vascular or mosquito clamp, and the arthroscope shaft with a blunt trocar is inserted in the direction of the web space between the first and second toe until it touches the talar bone.
Subsequently, the posteromedial portal is established at the medial edge of the calcaneal tendon, at the same height as the posterolateral portal. The direction of the portal is the most important aspect to consider. The mosquito clamp is introduced and then arthroscope shaft with the blunt trocar is inserted in a medial-to-lateral direction until it touches the arthroscope shaft positioned in the posterolateral portal. It then slides along the shaft, which acts as a guide, until the tip is reached (Fig. 3.16). After the periarticular fatty tissue is removed. During resection of the periarticular fatty tissue, fascial fibers that have a transverse course and a consistent appearance can easily be recognized (Golanó et al. 2006a, b). These fibers are part of the deep crural fascia that, because of its constant movement, is considerably thickened at the level of the ankle joint. In 1932, Rouvière and Canela-Lázaro gave this structure the name fibulotalocalcaneal ligament (Rouvière and Canela-Lazaro 1932) (Figs. 3.17 and 3.18). The flexor hallucis longus tendon, the lateral talar process, the ankle joint capsule with the posterior ligaments of the joint, and the subtalar joint capsule can be identified. Among these structures, the flexor hallucis longus tendon acquires special relevance because the tibial neurovascular bundle (tibial nerve, posterior tibial artery and veins) is located medial to it (Fig. 3.17). Care should be taken to avoid injury to the flexor hallucis longus tendon, which is considered the main endoscopic landmark because its lateral border determines the working area. Proper positioning of the ankle and the hallux results in better visualization of the tendinous portion of the flexor hallucis longus muscle and avoids unnecessary resection of some of the muscle fibers that reach the lateral tendinous border in a semipeniform morphology. Plantar flexion of the ankle or hallux flexion facilitates visualization of the flexor hallucis longus tendon proximal to the lateral talar process.
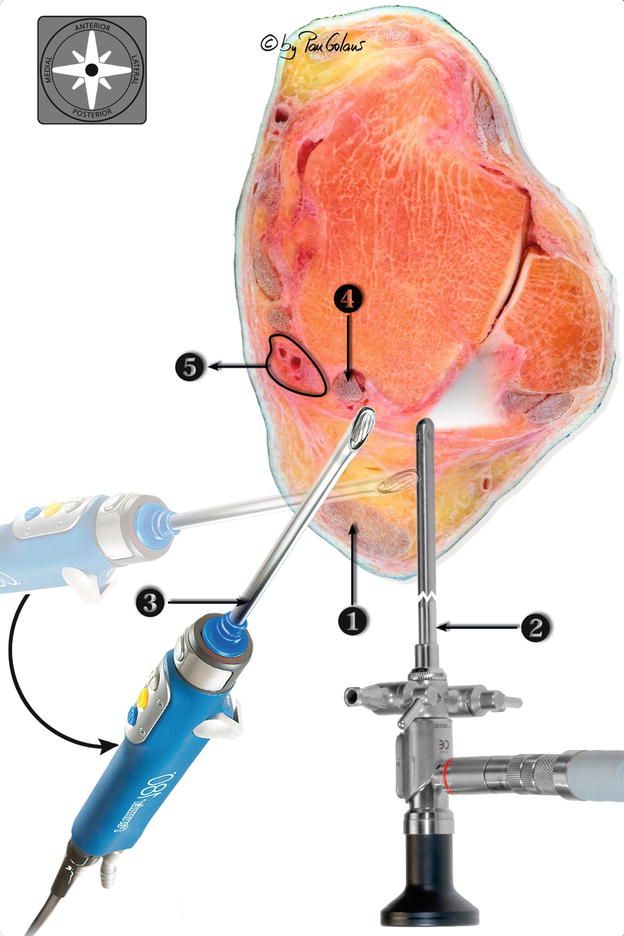
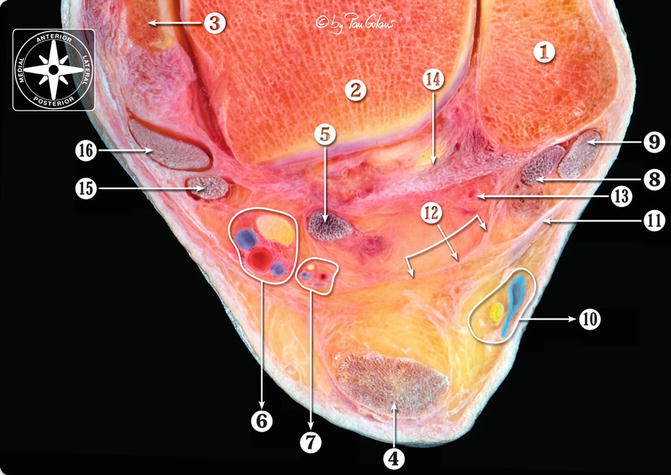
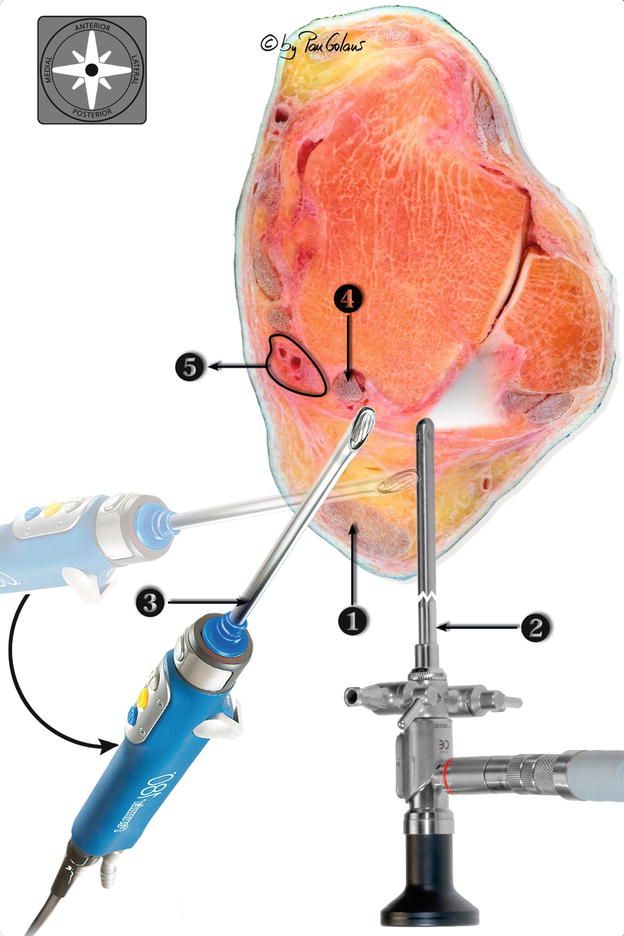
Fig. 3.16
Photocomposition showing the location of the posterolateral and posteromedial portals. The arthroscope and the arthroscopy motor were added digitally (Adobe Photoshop). The arthroscope is on the posterolateral portal. The arthroscopic view (light) is in lateral direction. The instruments are on the posteromedial portal. 1 Calcaneal tendon, 2 posterolateral portal, 3 posteromedial portal, 4 flexor hallucis tendon, 5 posterior neurovascular bundle (tibial nerve, posterior tibial artery and veins) (With kind permission of © Pau Golanó 2013)
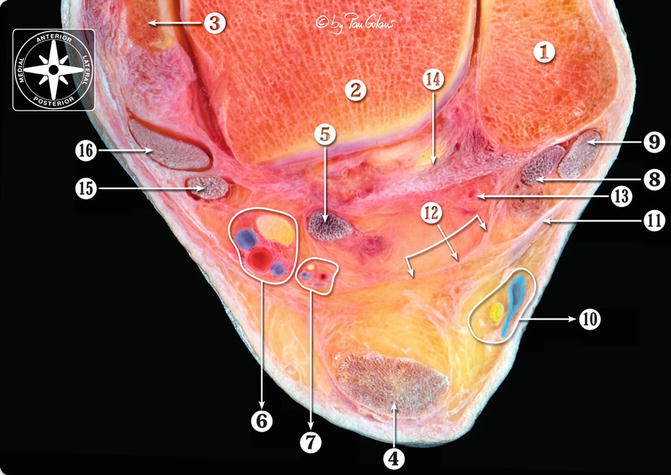
Fig. 3.17




Transversal section at the ankle joint (close- up). The nerves and vessels were painted digitally (Adobe Photoshop). 1 Lateral malleolus, 2 os talus, 3 medial malleolus, 4 calcaneal tendon, 5 flexor hallucis longus tendon, 6 posterior neurovascular bundle (tibial nerve, posterior tibial artery and veins), 7 medial calcaneal nerve, 8 peroneus brevis tendon, 9 peroneus longus tendon, 10 sural nerve and small saphenous vein, 11 superior peroneal retinaculum, 12 deep crural fascia (Rouvière and Canela Lazaro ligament), 13 posterior peroneal artery, 14 posterior tibiofibular ligament, 15 flexor digitorum longus tendon, 16 tibialis posterior tendon (With kind permission of © Pau Golanó 2013)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








