The capsule, labrum, glenohumeral ligaments, and rotator cuff represent the static and dynamic stabilizers of the glenohumeral joint. Various injuries can occur to one or more of these structures during traumatic shoulder dislocation, predisposing the patient to recurrent instability. Improved understanding of shoulder anatomy and biomechanics, and advancements in arthroscopic technique led to the recognition of various pathologic lesions that may contribute to instability. The ability to identify and address these lesions during arthroscopy will allow the surgeon to more fully tailor operative treatments for each individual patient suffering from shoulder instability. Furthermore, the ability to differentiate pathologic lesions from normal anatomic variants is critical to avoid inadvertent repair that will lead to loss of normal function and worsening symptoms.
The importance of diagnostic arthroscopy in the management of patients with acute and recurrent shoulder instability is well recognized. Prior to the use of arthroscopy to diagnose and repair pathologic causes of shoulder instability, the patient’s age at time of initial dislocation and to a lesser degree the period of immobilization were the main risk factors determining recurrent dislocation. Recent level I evidence showed that primary arthroscopic repair in patients with first-time shoulder dislocation reduces the risk of recurrent dislocation and improves the patient’s functional outcome. Improved understanding of shoulder anatomy and biomechanics led to the recognition of various pathologic lesions that may contribute to instability. The ability to identify and address these lesions during arthroscopy will allow the surgeon to more fully tailor operative treatments for each individual patient suffering from shoulder instability.
Although the Bankart lesion is still the most common lesion associated with shoulder instability, various other lesions have been identified and must be addressed during shoulder arthroscopy to prevent significant disability associated with recurrent dislocations. In 1993 Norlin reviewed 24 patients with first-time anterior shoulder dislocation who were evaluated with examination under anesthesia and arthroscopy. He found that all shoulders sustaining anterior dislocations had Bankart and Hill-Sachs lesions, and concluded that these uniform arthroscopic findings did not allow them to be used as predictors for recurrent instability.
Normal anatomy
The shoulder joint has few restraints to motion, thus providing it with 6° of freedom to allow for a wide array of actions ranging from the activities of daily living to high-intensity athletics. To strike a balance between broad functionality and frank instability, the shoulder is equipped with many important anatomic structures that act in concert to maintain stability while facilitating function.
Labrum
The glenohumeral joint has been analogized to a golf ball sitting on a tee, to highlight the glenoid’s relative lack of depth and surface area when compared with the larger spherical humeral articular surface. The fibrocartilagenous labrum compensates for this relative deficiency by acting to maintain glenohumeral congruency via several mechanisms.
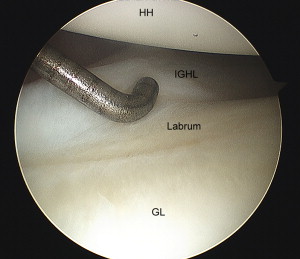
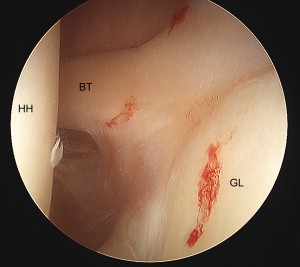
First it acts as an attachment for the capsule and ligamentous structures, anchoring these stabilizers to the glenoid rim. The labrum itself is firmly attached to the glenoid in its inferior hemisphere through a narrow rim of fibrocartilagenous tissue that directly transitions into the glenoid articular cartilage. The inferior glenohumeral ligament (IGHL) blends in directly with the inferior labrum ( Fig. 1 ). In its superior half above the glenoid equator, the labrum is more loosely and variably inserted, leading to anatomic variants that may be confused as pathologic when identified during arthroscopy. The superior labrum receives fibers directly from the long head of the biceps tendon (LHBT) that inserts onto the supraglenoid tubercle in close proximity to the superior edge of the glenoid ( Fig. 2 ). Cooper and colleagues demonstrated that the labrum is vascularized only in its periphery, and is more perfused in the posterosuperior and inferior portions.
Furthermore, the labrum significantly enhances the concavity of the glenoid socket. Howell and Galinat showed that the labrum deepens the glenoid by 9 mm in the superoinferior plane and 5 mm in the anteroposterior plane, and that loss of the labrum would reduce glenoid depth by more than 50% in both directions. The labrum also increases the surface area of contact for the humeral head, and may function as a load-bearing structure loosely analogous to the meniscus in the knee.
Superior Glenohumeral Ligament, Coracohumeral Ligament, and Rotator Interval
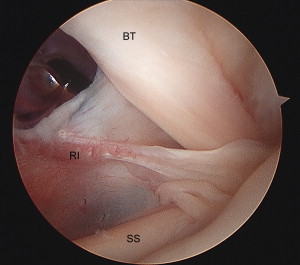
The rotator interval (RI) is a medially based triangular space within the glenohumeral joint capsule. The RI contains 3 structures in close association (coracohumeral ligament [CHL], superior glenohumeral ligament [SGHL], and long head of the biceps tendon), and is considered important to shoulder stability because sectioning of the interval leads to increased anterior, posterior, and inferior humeral head translation. The borders of the interval are as follows: the medial base is formed by the lateral aspect of the coracoid, the superior border is formed by the anterior margin of the supraspinatus tendon, and the inferior border is formed by the superior margin of the subscapularis tendon ( Fig. 3 ). The CHL is a broad (1–2 cm), thin structure that originates on the lateral aspect of the coracoid and courses through the RI to insert onto the greater and lesser tuberosities on either side of the bicipital groove. Deep to the CHL in the RI lies the SGHL, which is variable in size and is present in more than 90% of cases. The SGHL is usually small and variably originates from the supraglenoid tubercle and anterosuperior labrum, running just anterior to the long biceps tendon and parallel to the CHL as it inserts onto the humerus just superior to the lesser tuberosity. The intra-articular portion of the long biceps tendon pierces the interval at its apex during the tendon’s course out of the joint, after which it immediately enters the bicipital groove.
The biomechanical role of the CHL and SGHL has been extensively studied and there exists various opinions regarding their relative importance in maintaining stability. These 2 structures have similar roles because they share a parallel course, and act to limit inferior translation and external rotation when the arm is adducted. There is also evidence that they limit posterior translation when the shoulder is in forward flexion, adduction, and internal rotation.
Middle Glenohumeral Ligament
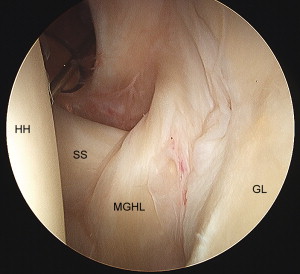
The middle glenohumeral ligament (MGHL) is the most variable in size and appearance of all the glenohumeral ligaments. Typically, the MGHL originates from the supraglenoid tubercle and anterosuperior labrum in close relation to the SGHL and inserts just anterior to the lesser tuberosity, blending with the fibers of the subscapularis tendon ( Fig. 4 ). The MGHL acts to limit anterior and posterior humeral head translation when the arm is abducted between 60° and 90° and limits inferior translation when the arm is adducted.
Inferior Glenohumeral Ligament Complex
The IGHL originates from the inferior half of the labrum and adjacent glenoid neck and inserts just inferior to the MGHL on the humerus (see Fig. 1 ). Arthroscopic, gross, and histologic studies by O’Brien and colleagues delineated the IGHL as a complex of 3 components: the anterior band, the axillary pouch, and the posterior band. Later studies by Ticker and colleagues indicated that the posterior band was less discrete and showed greater variation than the anterior band and axillary pouch.
The IGHL complex clearly plays an important role in shoulder stability as it often becomes disrupted following anterior dislocation. The relative location of the IGHLC changes with respect to arm position. When the shoulder is internally rotated, the complex moves posteriorly, preventing excessive posterior translation. Conversely, the complex moves anteriorly during external rotation to limit anterior displacement. During abduction, the complex is located inferior to the humeral head and becomes taut, thereby limiting inferior translation. The anterior and posterior components of the complex variably tighten during forward flexion or extension to limit anteroposterior displacement. Therefore, the IGHLC makes up a net that captures the humeral head to limit its translation on the glenoid fossa throughout much of normal shoulder motion.
Rotator Cuff
The labrum and glenohumeral ligaments are regarded as static stabilizers because each of these structures provides a unidirectional limitation to translation in any given shoulder position. By contrast, the rotator cuff is perfectly positioned to dynamically stabilize the joint throughout its range of motion. Active contraction of the rotator cuff imparts stability via 2 mechanisms: (1) active joint compression of the humeral head into the glenoid, and (2) glenohumeral ligament dynamization through direct attachments to the rotator cuff.
Biomechanical studies by Lippitt and Matsen showed that the magnitude of tangential forces needed to dislocate the shoulder increased as more compression forces were applied across the joint. Lippitt and Matsen described the concept as “concavity-compression” and noted that given an intact labrum, the joint could sustain tangential forces up to 60% of the compressive force. Bowen and colleagues showed that even when three-fourths of the joint capsule had been sectioned, a compressive force of 111 N could prevent dislocation in the face of a 50-N tangential force. Synchronous rotator cuff contraction is needed to center and contain the humeral head on the glenoid, thus providing a stable fulcrum for humeral elevation. Deficiencies in rotator cuff musculature result in superior migration of the humeral head. The degree of migration is directly related to the magnitude of cuff deficiency. In overhead throwing athletes who have instability related to overuse injury, Warner and colleagues showed that symptomatic patients had altered rotator cuff strength patterns predisposing them to injury of the GHL and capsule.
Intraoperative arthroscopic observation indicates that the various glenohumeral ligaments are intimately related to the rotator cuff tendons, and anatomic studies have confirmed that in many locations the ligaments are directly attached to the cuff. Furthermore, the joint capsule is in contact with the cuff in all locations except in the RI. Therefore, it is postulated that with active joint motion, the rotator cuff will dynamize the attached capsuloligamentous structures, further enhancing their ability to maintain physiologic extents of humeral translation. Further studies are needed to elucidate the direct effect of dynamic cuff contraction on each ligamentous structure during shoulder range of motion.
Biceps Tendon
The LHBT originates from the supraglenoid tubercle and superior labrum and courses through the joint to pierce the apex of the RI, becoming extra-articular as it enters the bicipital groove. Using a dynamic cadaveric model, Rodosky and colleagues showed that detachment of the superior glenoid labrum increased anterior shoulder instability and placed greater strain in the IGHL complex during torsional loading in the abducted, externally rotated position. Pagnani and colleagues showed that a superior labral lesion that disrupted the supraglenoid biceps origin resulted in increased glenohumeral translation in anteroposterior and superoinferior directions. In an electromyographic analysis of biceps muscle function in patients with anterior instability, Kim and colleagues found that the voltage of the biceps was significantly greater in affected individuals than in matched controls, especially with the shoulder in abduction or external rotation. These studies support the concept that the biceps play a compensatory role as a dynamic stabilizer when the rotator cuff and static stabilizers are deficient, as in patients with recurrent instability or at the extremes of shoulder motion in overhead athletes.
Normal variants
Although the various anatomic structures all have a defined role in maintaining shoulder stability, there are many variations in normal anatomy that must be recognized at arthroscopy so they are not mistaken for pathologic lesions.
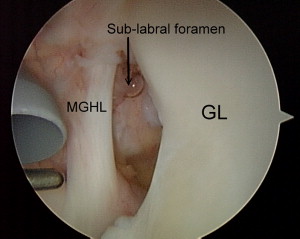
Sublabral Foramen and the Buford Complex
As described previously, the superior half of the labrum is more loosely and variably attached to the glenoid than the inferior hemisphere. The result is the presence of sublabral foramen, either in isolation or in conjunction with other variant anatomy, in a significant percentage of patients undergoing arthroscopy ( Fig. 5 ). The anterosuperior quadrant is the most common location for sublabral foramen, with incidence of 11.9% to 18.5% in shoulders undergoing arthroscopy in recent series. These observational studies found that sublabral foramens are not independent contributors to instability, and validated the prevailing practice of ignoring them during arthroscopy, especially if they occur above the glenoid equator and are in isolation.
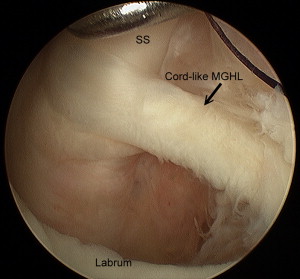
The Buford complex is a rare but widely recognized normal variant defined by a large anterosuperior sublabral foramen occurring in conjunction with a thickened, cordlike MGHL. The Buford complex can be mistaken for an anterior labral avulsion or superior labral tear when interpreted on magnetic resonance imaging (MRI), but is readily recognizable during arthroscopy because of its characteristic appearance. In 3 recent series of patients undergoing arthroscopy, the incidence of the Buford complex was noted to be 6.5% to 10.2%, although a cadaveric series of 84 shoulders found the incidence to be 1.3%. Most investigators agree that the Buford complex in isolation does not necessitate arthroscopic repair, but there is some evidence that this variant may occur with greater frequency in patients with superior labral anterior posterior (SLAP) tears.
MGHL Variations
The MGHL is highly variable in appearance and can be absent in up to 30% to 40% of shoulders. MGHL can originate from the anterosuperior labrum, the suprageloid tubercle, or the scapular neck. The 2 most common versions of the MGHL are the cordlike appearance with foraminal separation between it and the IGHL ( Fig. 6 ) or the sheetlike variant that blends in with the anterior band of the IGHL. The MGHL can often be detached along with the IGHL during anterior dislocation as part of the Bankart lesion. This pathologic detachment of the MGHL must be differentiated from the anatomic sublabral foramen that often occurs in close proximity to this ligament.
Superior Labral Variants
The superior labrum can have great anatomic variability owing to its loose glenoid attachment and its relationship with the LHBT. Vangness and colleagues described the highly variable origin of the LHBT from the superior labrum and scapula, noting 4 main types of biceps insertion that each occurred with significant frequency (the rarest type was a primarily anterior origin that occurred in 8%). The presence of a synovial recess between the biceps tendon and the superior labrum should not be mistaken for a SLAP tear, because arthroscopic inspection will reveal a firm biceps insertion. Finally, a meniscoid superior labrum is a normal variant that is not associated with shoulder symptoms.
Normal variants
Although the various anatomic structures all have a defined role in maintaining shoulder stability, there are many variations in normal anatomy that must be recognized at arthroscopy so they are not mistaken for pathologic lesions.
Sublabral Foramen and the Buford Complex
As described previously, the superior half of the labrum is more loosely and variably attached to the glenoid than the inferior hemisphere. The result is the presence of sublabral foramen, either in isolation or in conjunction with other variant anatomy, in a significant percentage of patients undergoing arthroscopy ( Fig. 5 ). The anterosuperior quadrant is the most common location for sublabral foramen, with incidence of 11.9% to 18.5% in shoulders undergoing arthroscopy in recent series. These observational studies found that sublabral foramens are not independent contributors to instability, and validated the prevailing practice of ignoring them during arthroscopy, especially if they occur above the glenoid equator and are in isolation.
The Buford complex is a rare but widely recognized normal variant defined by a large anterosuperior sublabral foramen occurring in conjunction with a thickened, cordlike MGHL. The Buford complex can be mistaken for an anterior labral avulsion or superior labral tear when interpreted on magnetic resonance imaging (MRI), but is readily recognizable during arthroscopy because of its characteristic appearance. In 3 recent series of patients undergoing arthroscopy, the incidence of the Buford complex was noted to be 6.5% to 10.2%, although a cadaveric series of 84 shoulders found the incidence to be 1.3%. Most investigators agree that the Buford complex in isolation does not necessitate arthroscopic repair, but there is some evidence that this variant may occur with greater frequency in patients with superior labral anterior posterior (SLAP) tears.
MGHL Variations
The MGHL is highly variable in appearance and can be absent in up to 30% to 40% of shoulders. MGHL can originate from the anterosuperior labrum, the suprageloid tubercle, or the scapular neck. The 2 most common versions of the MGHL are the cordlike appearance with foraminal separation between it and the IGHL ( Fig. 6 ) or the sheetlike variant that blends in with the anterior band of the IGHL. The MGHL can often be detached along with the IGHL during anterior dislocation as part of the Bankart lesion. This pathologic detachment of the MGHL must be differentiated from the anatomic sublabral foramen that often occurs in close proximity to this ligament.









