Arthrodesis of the Tarsometatarsal Joint
Introduction
Lisfranc ligament runs from medial cuneiform to base of second metatarsal; strongest part is plantar portion; limits movement
Tarsometatarsal (TMT) joint movement
First joint—5° to 10°
Second and third joint—Almost none
Fourth and fifth joint—10° to 20°
Recessed second TMT joint stabilized by plantar ligaments between medial and lateral cuneiforms
Patient Selection
Indications
Primary fusion
Major ligament disruption with multidirectional instability of Lisfranc joint
Comminuted intra-articular fractures at base of first or second metatarsal
Crush injuries of midfoot with intra-articular fracture-dislocation
Secondary fusion
Posttraumatic degenerative joint disease (DJD) after Lisfranc injury
Idiopathic TMT DJD
Rheumatoid arthritis
Stable/chronic Charcot neuroarthropathy, other complications of diabetes
Contraindications
Skeletal immaturity
Acute Charcot neuroarthropathy (relative)
Incomplete ligamentous injuries
Infection
Procedure

Figure 1Intraoperative photograph shows the surgical approaches for a tarsometatarsal joint fusion in a left foot. The medial incision is between the first and second metatarsals, just lateral to the extensor hallucis tendon. The lateral incision is at least 4 cm farther lateral, overlying the fourth metatarsal.
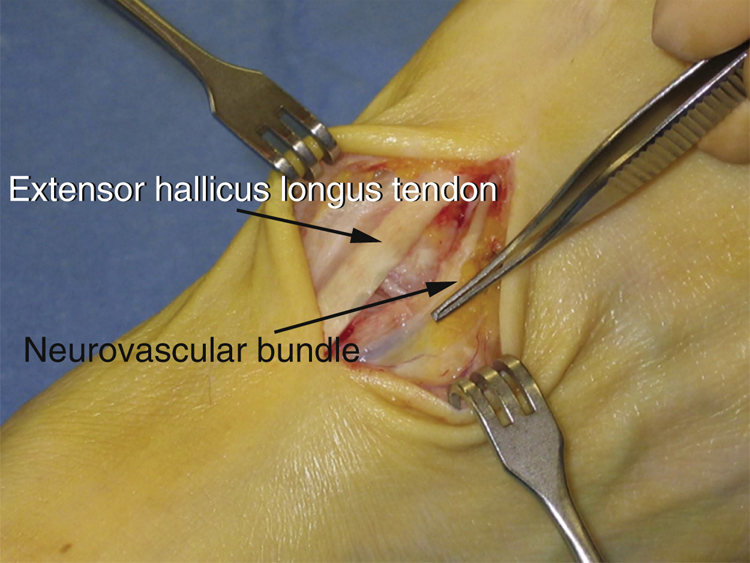
Figure 2Intraoperative photograph of a left foot shows the extensor hallucis longus tendon at the medial side of the incision. The dorsalis pedis artery and the deep peroneal nerve are lateral to the tendon and will be encountered during the exposure. A branch of the superficial peroneal nerve usually runs from lateral to medial across the distal portion of the exposure.

Figure 3AP radiograph shows typical screw placement in reduction of a dislocation of the first through third tarsometatarsal joints. The first ray is immobilized first, followed by the second and then the third.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


