Arthrodesis of the Hallux Interphalangeal Joint
David R. Richardson
G. Andrew Murphy
There are a number of disorders affecting the interphalangeal (IP) joint of the hallux to the extent that stabilization, with or without realignment, is warranted when soft tissue reconstruction alone is not a viable option.
The IP joint is a hinge joint that flexes and extends in the sagittal plane. Most of the motion occurs in plantarflexion, and the total range of motion averages about 46°. It is stabilized by the joint capsule and medial and lateral collateral ligaments. The capsular tissue is thicker plantarward and may include an IP sesamoid, which is occasionally symptomatic from an intractable plantar keratosis overlying the prominent sesamoid. The flexor hallucis longus (FHL) tendon crosses the joint on the plantar aspect and the extensor hallucis longus (EHL) dorsally.
It is commonly affected by arthritis, instability, or deformity in plantarflexion or dorsiflexion or valgus. Certain athletic activities that place significant stress on the hallux (ballet, track, martial arts) may predispose this joint to early arthrosis. Direct trauma may cause an IP fracture with posttraumatic stiffness and/or arthritis. IP dislocation may occur from a higher energy injury and sometimes may be irreducible. Inflammatory arthritis, such as rheumatoid or psoriatic arthritis, may affect the IP joint. Degenerative arthritis can affect the IP joint, and there are factors that may contribute to early degeneration. Stiffness of the more proximal metatarsophalangeal (MTP) joint may lead to IP degenerative joint disease (DJD) or dorsiflexion instability. First MTP arthrodesis may contribute to early IP degeneration, particularly if the hallux is positioned with too little dorsiflexion or too little valgus. The IP joint may be deformed in flexion, such as a claw toe, or angulated in valgus as in hallux valgus interphalangeus.
INDICATIONS AND CONTRAINDICATIONS
Arthrodesis of the IP joint is indicated in patients with painful IP arthritis, instability, or deformity. It is commonly used to treat pain and deformity caused by inflammatory arthritis (e.g., rheumatoid or psoriatic), previous trauma such as an IP dislocation or intra-articular fracture, degenerative arthritis, or repetitive stress to the hallux (1).
Arthrodesis may be combined with other operations such as tendon transfer (1, 2, 3 and 4). It is used in conjunction with other procedures to correct MTP instability of the hallux caused by muscle imbalance. These include transfer of the EHL to the metatarsal neck (Jones procedure) for intrinsic muscle denervation (e.g., Charcot-Marie-Tooth disease) (2,3) and EHL transfer to the lateral aspect of the proximal phalangeal base for hallux varus deformity. For flexor hallucis brevis weakness after a sesamoidectomy, fusion of the IP joint allows the FHL to flex the first MTP joint.
Arthrodesis of the IP joint is contraindicated in asymptomatic deformity or joint arthrosis based solely on cosmetic concerns or radiographic findings. Inadequate vascularity and active infection before surgery also are contraindications.
PREOPERATIVE PLANNING
Comorbidities, including renal failure, diabetes, vitamin D deficiency, alcoholism, and smoking, that may affect outcome should be carefully assessed and the risks discussed with the patient. Medications that a patient is currently taking also should be carefully reviewed, because some, such as corticosteroids, nicotine patches, and antirheumatic drugs, affect wound healing potential. Patients must have the ability to follow through with postoperative immobilization regimens. Although full weight bearing is allowed, immobilization in a stiff-soled postoperative shoe or boot is required.
The vascular status must be evaluated, and in high-risk individuals, noninvasive vascular studies should be obtained and a vascular consult requested as necessary. Absolute systolic toe pressure higher than 50 mm Hg indicates adequate wound healing potential. An osteotomy or cheilectomy in addition to the IP joint arthrodesis may be necessary if motion at the IP joint of the hallux is less than neutral dorsiflexion. If the EHL is to be transferred, function of the extensor hallucis brevis (EHB) should be determined.
Standing anteroposterior, lateral, and oblique radiographs should be obtained to evaluate the position of the IP joint of the hallux, bone quality, and the amount of hallucal shortening and to determine the appropriate screw length and diameter necessary for fixation. In addition, the radiographs may show a malunited fracture or cystic changes that may require bone grafting.
Appropriate hardware and surgical instruments should be available, including a cannulated compression screw (preferred), Kirschner wires for crossed fixation if necessary or staples, fluoroscope, tenaculum, microsagittal saw, and a no. 15 surgical scalpel blade.
SURGICAL TECHNIQUE
Regional anesthesia with monitored sedation is most commonly used. This may include an ankle, forefoot, or even digital block. If a digital block is used, the entire procedure should be distal to the MTP joint. For an ankle or forefoot block, three 10-mL syringes with local long-acting anesthetic (e.g., bupivacaine hydrochloride) are used. Epinephrine should not be used for regional anesthesia distal to the ankle.
After the foot is exsanguinated and a well-padded ankle tourniquet is placed, attention is turned to the dorsum of the hallux.
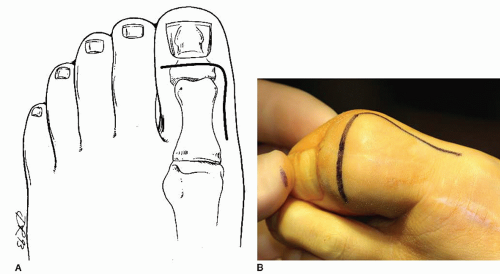
An L-shaped incision is made with the corner of the L dorsomedially just distal to the IP joint of the hallux and proximal to the nail eponychium (Fig. 2.1). As an alternative, an S-shaped incision centered at the level of the IP joint can be used.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree