Triple Arthrodesis for Adult Acquired Flatfoot
Alan R. Catanzariti, DPMa∗acatanzariti@faiwp.com, Brian T. Dix, DPMa, Phillip E. Richardson, DPMa and Robert W. Mendicino, DPMbc, aDivision of Foot & Ankle Surgery, West Penn Hospital, 4800 Friendship Avenue, Pittsburgh, PA 15224, USA; bOhioHealth Orthopedic Surgeons, Hilliard, OH, USA; cFoot & Ankle Surgical Residency, West Penn Hospital, 4800 Friendship Avenue, Pittsburgh, PA 15224, USA
The primary goal of triple arthrodesis for stage III and IV adult acquired flatfoot is to obtain a well-aligned plantigrade foot that will support the ankle in optimal alignment. Ancillary procedures including posterior muscle group lengthening, medial displacement calcaneal osteotomy, medial column stabilization, peroneus brevis tenotomy, or transfer and harvest of regional bone graft are often necessary to achieve adequate realignment. Image intensification is helpful in confirming optimal realignment before fixation. Results of triple arthrodesis are enhanced with adequate preparation of joint surfaces, bone graft/orthobiologics, 2-point fixation of all 3 tritarsal joints, and a vertical heel position.
Key points
Triple arthrodesis for adult acquired flatfoot is typically indicated in stage III and stage IV deformities.1–4 These patients often have end-stage arthritis and significant deformity that is nonreducible. The authors also consider triple arthrodesis when there has been a failed joint-sparing procedure or a failed arthrodesis of an isolated tritarsal joint to address stage II adult acquired flatfoot. The goals of surgery include resolution of symptoms, realignment, and sound arthrodesis.
Medial displacement osteotomy of the calcaneus has been mentioned previously as an adjunct procedure to address ankle valgus or medial soft-tissue attenuation (Fig. 1). Resnick and colleagues5 have shown that a triple arthrodesis in combination with a medial displacement osteotomy of the calcaneus will reduce deltoid ligament forces by 56%. Song and colleagues6 have also suggested that medializing the calcaneus following triple arthrodesis protects the deltoid complex.
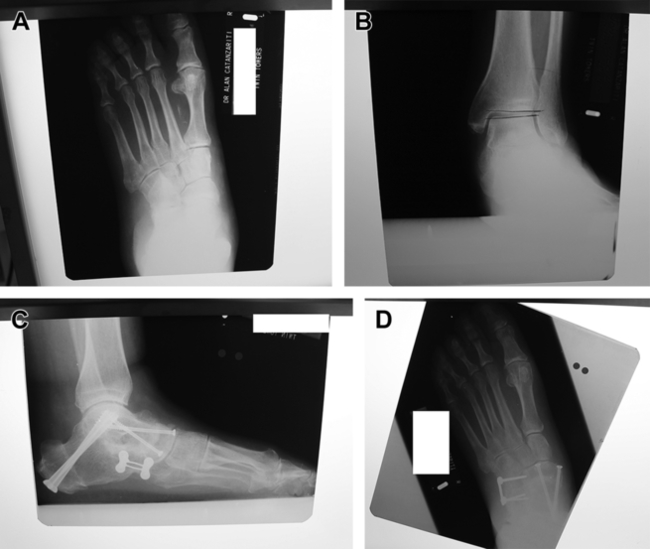
The authors will consider medial column stabilization, in the form of either naviculocuneiform arthrodesis or first tarsometatarsal arthrodesis, when medial column instability is identified following triple arthrodesis for stage III adult acquired flatfoot (Fig. 2). Insufficiency of the medial column can result in a functional varus. Failure to address medial column instability can result in a lateral column overload when patients begin weight bearing, with subsequent fifth metatarsal base bursitis or fifth metatarsal head callosities.

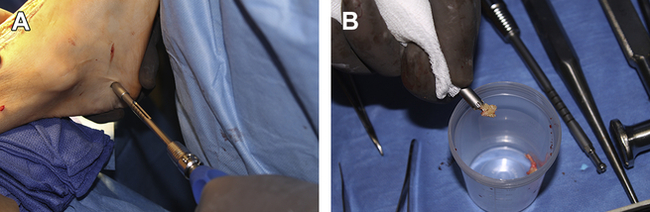
Harvesting of regional bone graft and/or bone marrow aspirate is a part of virtually every triple arthrodesis. Cancellous bone is often harvested from the calcaneus using 6- to 8-mm trephines through small lateral incisions (Fig. 3). Bone marrow aspirate is obtained from the calcaneus before tourniquet inflation. The cancellous bone is packed into arthrodesis sites. The extra-articular areas along the undersurface of the talus and the dorsal surface of the calcaneus are decorticated. The bone marrow aspirate is mixed with bioactive glass and is then packed into this extra-articular area.
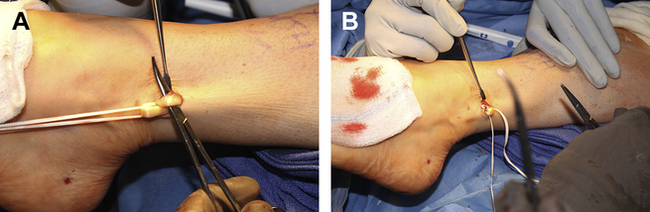
Transfer of peroneus brevis to peroneus longus tendon is performed when the deformity is severe (Fig. 4). Severe contracture of the peroneus brevis tendon can sometimes make it difficult to obtain complete realignment. As an alternative, the authors sometimes transect both tendons.
Surgical technique for triple arthrodesis
Subtalar and Calcaneocuboid Dissection
Triple arthrodesis is typically performed through a combination of medial and lateral incisions. The lateral incision extends from the tip of the lateral malleolus and courses distally to the fourth metatarsal base (Fig. 5). This incision is dorsal to the peroneal tendons and sural nerve. Care is taken to maintain hemostasis with cauterization or ligation of the venous structures within this area. A sponge lightly moistened with saline may be used for planal dissection down to the fascia. The peroneal tendons are then mobilized with Metzenbaum scissors and retracted inferiorly (Fig. 6). Dissection is then carried down to the level of deep fascia and the extensor digitorum brevis muscle belly. An inverted T-shaped incision is performed with the base of the incision along the inferior aspect of the muscle belly, extending proximally along the lateral capsule of the talocalcaneal joint. The vertical arm of the incision is within the sinus tarsi. A second vertical incision is then placed parallel within the sinus tarsi, and the contents of the sinus tarsi are thoroughly evacuated (Fig. 7). This action enhances visualization and access to the subtalar joint (STJ). Dissection is then carried proximally along the lateral talocalcaneal joint, where the calcaneofibular ligament is incised to facilitate access to the STJ (Fig. 8). The lateral talocalcaneal ligaments and calcaneofibular ligament are often contracted in long-standing adult acquired flatfoot. Releasing these periarticular structures will enhance mobilization of the STJ, and therefore permit easier access and realignment.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree