Chapter 3 Aquatic Physiotherapy
Introduction
• Aquatic physiotherapy, despite perhaps being the most ancient therapy, is also a contemporary therapy for the modern world.
• A five-year plan published by the Government encompassing the period 2010–2015 emphasises the need for a more preventative, people-centred and productive National Health Service (DOH 2009).
• Modern aquatic physiotherapy involves people who otherwise are likely to be inactive or not regularly involved in exercise (Jackson et al 2004), is suitable for all (Epps 2009), focuses on the individual and can be exceptionally cost-effective (HyDAT, 2009, Maynard 2003).
• Thus aquatic physiotherapy can be argued to be extremely relevant to the future delivery of an efficient and effective health care service.
• Historically, early religious practices in many cultures emphasised the healing powers of water, for example, the Babylonians, the early Hebrews, and ancient Indians.
• The Greco-Roman civilisation made many claims of water treatment and the Romans centred their social lives on their baths. The collapse of the Roman Empire led to a decline in medical and social bathing.
• Immersion in water re-emerged briefly in the Middle Ages in Europe and then again in the 17th century in England (Alder 1983).
• By the mid 20th century many British doctors rejected spa treatment as being unscientific, but it continued to thrive in much of Europe (Kersley 1982).
• Despite the negative opinions of some regarding the benefits of water-borne treatment, from the 1930s onwards the Chartered Society of Physiotherapy (CSP), with the support of rheumatologists, began to train physiotherapists to use water baths as a treatment for rheumatism (Skinner and Thompson 1983).
• This was the beginning of modern aquatic physiotherapy, which can be defined as:
‘A physiotherapy programme utilising the properties of water, designed by a suitably qualified physiotherapist. The programme should be specific for an individual to maximise function, which can be physical, physiological, or psychosocial. Treatments should be carried out by appropriately trained personnel, ideally in a purpose built, and heated Aquatic Physiotherapy pool’ (ATACP 2009).
• Thus in contemporary health care provision aquatic physiotherapy should form an integral part of a rehabilitation programme and more broadly be considered as a part of the patient pathway.
• It may be used as the only form of treatment being offered at that time, or may form part an overall treatment plan, designed to be complementary to other aspects of a person’s planned treatment programme.
• Aquatic physiotherapy is often considered when all other forms of medical and physiotherapeutic intervention have failed.
• During the initial assessment of a patient consideration should be given to the inclusion of aquatic physiotherapy as a primary option in the management of a wide variety of conditions.
• Modern therapists need knowledge and skills to use this treatment safely and effectively (ATACP 2006). To ensure this, the ATACP run a foundation programme for chartered physiotherapists (ATACP 2010).
Assessment
• The main aspects of the assessment for aquatic physiotherapy are the same as many of the specialist areas within the physiotherapy scope of practice. For example a patient being assessed for a musculoskeletal problem would have the same tests performed for aquatic therapy as would be carried out prior to local soft tissue treatment, exercise or advice on land.
• A patient with a neurological condition would have the same assessment of balance, tone or function as they would prior to land treatment.
• It is recommended that the ‘SOAP’ note-keeping format is used, and that outcome measures appropriate to the condition are utilised.
• As an alternative the ‘Measure it Yourself Medical Outcome Profile’ (MYMOP) has the advantage of being non-condition-specific and easily used for most patient groups. It is a commonly used outcome measure across aquatic physiotherapy services in the United Kingdom (Paterson 1996).
• It is important to clinically reason why treatment in the pool should be the treatment of choice. Ask the question ‘Why water?’ (Can the patient be treated more effectively, more easily, or more appropriately in water than on dry land?).
• Without a sound knowledge of the physical properties of water, and the skills to utilise those properties to create effective treatment techniques this question is difficult to answer.
• A part of this chapter concentrates on the relevant physical properties, to assist the reader to be able to form reasoned decisions in this area.
• Knowledge of how a patient’s body build or presenting condition can alter their behaviour in water is also vital.
• It is also important to have a clear understanding of the physiological changes that occur when a human body is immersed in water, as these form a large part of the screening process to ensure that the patient is safe to enter the pool.
• In addition, the person’s ‘confidence’ in water needs to be assessed, both prior to and during the initial stages of treatment. Apart from asking the patient if they are happy in water, it is possible to observe clues such as the patient gripping onto the rails tightly, with a marked reluctance to let go, pulling themselves along the rail as they are laid back in water, or a reluctance to put their head or face near the water surface.
The physical properties of water
• The relevant properties physiotherapists need to be aware of to ensure that patients are appropriately referred and effectively treated in a pool are:
Hydrostatic pressure
• Hydrostatic pressure is created by the weight of water pressing down from above, and acts in all directions at right angles to any solid surface it is in contact with, e.g. the pool walls or patient’s body.
• It follows Pascal’s principle that this pressure is transmitted equally and undiminished in all directions through any fluid within a confined space (Brody and Geigle 2009).
i.e. the weight bearing down on a given spot.
– Pressure at the water surface is known as atmospheric pressure and equals 101 kilopascals (kPa).
– Pressure at 1 metre depth = 111 kPa
– Pressure at 2 metre depth = 121 kPa
– Pressure at 10 metre depth = 201 kPa
• In real terms this means that the human body standing in water up to their sternal notch will have a pressure of 120 g/cm2 being exerted on their calf region. This is equivalent to the application of a tight crepe bandage.
• There is 10 times more pressure on the ankles in water at 1 metre depth, than at the water surface.
• The main consideration therapeutically should be in relation to the physiological changes that occur in the patient’s body during immersion.
Relative density
• This is the density of any object or substance relative to the same volume of water at 4 °C (the temperature at which water is most dense).
• Water has a density of 1.000 kg/m3 – (I litre of water at 4°C weighs 1 kg).
• The average human body with air in the lungs has a relative density of 0.975, so will float with 2.5% of its volume out of the water (Brody and Geigle 2009).
• This relationship changes throughout life:
• Salt water has a density of around 1.024 kg/m3, so a body will float with a greater proportion out of the water.
• Anything less dense than water will float, while anything more dense will sink.
• Densities of different substances (kg/m3)
| Air | 0.00125 |
| Cork | 0.22 |
| Wood | 0.75 |
| Iron | 7.7 |
| Gold | 19.3 |
| Body Fat | 0.92 |
| Muscle | 1.058 |
| Rib bone | 1.383 |
| Tooth | 2.24 |
• As can be seen different parts of the body will behave differently in water due to their differing relative densities, the limbs will tend to sink while the trunk will tend to be more buoyant.
Buoyancy
• This is the ‘Upthrust’ effect of water acting on a body, and depends on both the relative density of the object, and the hydrostatic pressure forces being exerted upon it.
• It is governed by Archimedes’ principle. This states that ‘When a body is wholly or partially immersed in a fluid at rest it will experience an apparent weight loss equal to the weight of the fluid displaced.’
• In other words if you get into a pool of water and the water level rises by 1 inch, if you could weigh that inch of water you would know how much apparent weight relief you were experiencing.
• As a guide for a person standing, immersion to the anterior superior iliac spine gives 50% weight relief, to the xiphisternum 70% weight relief and to C7 90% weight relief (Harrison and Bulstrode 1987).
Centre of buoyancy (COB)
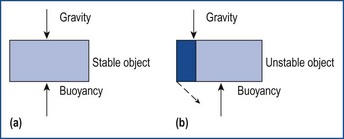
• This is the single point in an immersed object around which the buoyancy (upthrust) forces act.
• This point is the centre of gravity of the shape of the displaced fluid (i.e. its centre of gravity), and is therefore not a fixed point.
• This point moves as the attitude of the immersed body changes.
• In a body at rest it is slightly superior and anterior to the centre of gravity.
Metacentre (turning forces in water)
• The metacentre is the midpoint at which a body can be held in perfect balance.
• The term ‘metacentre’ is not really important, but the effects it has are.
• It is the naval term given to the resultant restoring or stabilising torque (twisting force) when the forces of gravity and buoyancy acting on an immersed object are not in the same vertical plane.
• For the human supine in water with arms at the side, the body will be stable side to side (forces of gravity and buoyancy in line).
Some factors that alter stability in water
‘Shape’ of the patient
• A person of very slight build will have the centre of buoyancy close to that of the centre of gravity. So in standing will tend to be more stable.
• The same applies to the more heavily muscled patient, they will tend to be ‘leg heavy’ with the legs sinking till they rest on the pool floor.
• A person with a large amount of adipose tissue around the abdomen will have a COG that is higher and more anterior, so they will have a tendency to rock backwards more, with legs that float up more readily.
• A person with physical deformity such as a lateral scoliosis will tend to roll in the water when supine due to the alteration of the position both of the centres of gravity and buoyancy.
• A person with osteoporosis in the lower limbs will float with the legs high, and may even lay with their face immersed when supine unless some sort of buoyancy is applied around the neck/head area.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree