Approach to the Patient with Knee Pain: Introduction
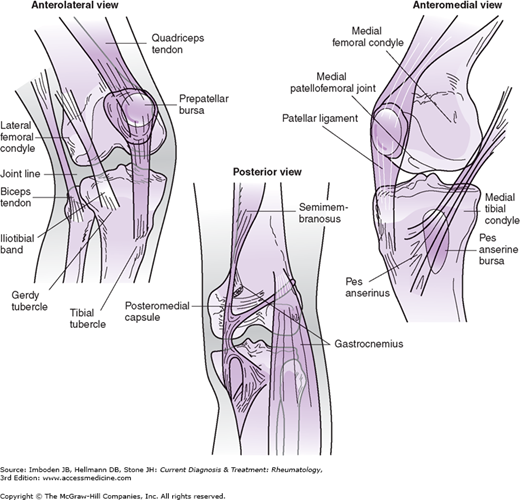
Knee pain is a common problem, accounting for 1.9 million visits to primary care practitioners and 1 million visits to emergency departments annually. By following a systematic approach in evaluating knee pain (which includes obtaining a thorough and directed history), focusing on specific questions, using the physical examination (sometimes with the assistance of diagnostic studies), and understanding knee anatomy (Figure 12–1), physicians are able to make the correct diagnosis and formulate an appropriate therapeutic strategy.
Overview of the Clinical Assessment
The first step in the evaluation of knee pain is a thorough history that includes the core elements outlined in Table 12–1. While obtaining a history, the following key questions should be addressed:
- Has there been an acute injury?
- Is a joint effusion present?
- Is there evidence of osteoarthritis?
- Are there mechanical symptoms?
- Is there evidence of systemic disease?
|
The answers to these questions help the clinician narrow the differential diagnosis and formulate a strategy for a directed work-up of the knee pain.
The history should also determine whether the pain is localized to a specific region of the knee, which also can be a helpful guide to the cause of symptoms. The examiner should take into account the age and sex of the patient, both of which can influence the differential diagnosis. Finally, the clinician should bear in mind that pain can be referred to the knee from other sites, most notably the ipsilateral hip. Every patient with knee pain should have a careful examination of the hip.
The general physical examination has 5 major components: observation of stance and gait, range of motion, palpation, examination for a knee effusion, and stability tests. After completing these general examinations and considering the patient’s history, the clinician can generate a differential diagnosis and focus the work-up accordingly (see specific injuries and conditions below).
Physical examination should start with observation of stance and gait. Can the patient bear weight on the affected leg? Is there a limp? Attention should be paid to medial or lateral translation of the knee upon heel strike. Angular (varus or valgus) deformities can identify bone and cartilage erosion with secondary stretching of the opposite collateral ligament. Varus alignment predisposes medial compartment arthritis. Following gait analysis, patients should be asked to perform a deep squat. Limitations in squatting may be related to patellofemoral or meniscal pathology.
Active and passive range of motion of the knee should be recorded. Normal knee extension is 0 degrees; normal knee flexion ranges from 115 to 160 degrees. It is helpful to compare with the contralateral side.
The skin overlying the anterior surface of the knee is typically cooler than the skin proximal and distal to the joint. The examiner can best detect a “warm” knee by using the dorsum of his or her hand to compare the temperature of the skin overlying the patella to the temperature of the skin “above and below” the knee (rather than comparing one knee to the other).
Palpation should be gentle but thorough to help localize the knee pain. Palpation around the patella can identify facet tenderness or insertional tenderness of the patella tendon and quadriceps tendon. Palpable defects along the quadriceps or patella tendon can indicate tendon ruptures. Injury along the collateral ligaments can best be identified with pain elicited along their course and at their attachments. Palpation of the joint line is done both medially and laterally to elicit pain that can be caused by meniscal injury. Tenderness at the tibial tubercle can indicate Osgood-Schlatter disease or patella tendon tears. Osteochondritis dessicans of the knee can also be diagnosed with a positive Wilson sign (pain with internal rotation and extension of the knee that is relieved with external rotation).
With the patient supine, an effusion is often visible as fullness in the suprapatella bursa and loss of the concavity that is usually present on the medial aspect of the knee. The effusion is confirmed by balloting the patella onto the femoral groove while compressing the suprapatellar and infrapatellar bursae. In the absence of fluid, the patella moves directly into the femoral condyles. With large effusions the patella will float above the condyles, so when the examiner quickly pushes down on the patella (balloting), a tap will be felt as the patella bumps into the condyles. Smaller effusions can be detected by compressing fluid from the medial compartment of the knee by applying a sweeping compression motion to the medial and superior aspects of the knee. If a small effusion is present, compression of the lateral aspect of the knee will generate a fluid wave that can be seen as a small bulge on the medial side.
Stability or provocative tests should be performed when the patient is relaxed. These tests can reproduce symptoms and thus can be uncomfortable. The examiner should determine the direction of instability of the knee: anterior cruciate ligament (ACL)/posterior cruciate ligament (PCL) tears produce anterior/posterior instability; collateral ligament injuries lead to varus/valgus instability as well as internal/external rotational instability. These tests are described in detail under specific disease entities.
Knee Pain that Follows Acute Injury
- Mechanism of injury often points to the diagnosis.
- “Popping sound” at the time of injury suggests an ACL injury.
- Plain radiographs may be indicated to rule out fracture.
- Instability suggests ligament injuries.
- Locking or catching suggests a meniscal tear.
Acute injuries can lead to fractures, patella dislocation, and internal derangements of the knee, including tears of the ligaments and meniscal cartilage (Table 12–2). Injuries also can cause acute traumatic bursitis as well as tendon strains and tears.
| Injury Mechanism | Joint Swelling | Characteristics | |
|---|---|---|---|
| ACL/PCL tears | Acute injury/trauma | Immediate | Instability |
| Meniscus | Deep squat or twisting | Delay (first 24 hour) | Pain with twisting |
| Patella dislocation | Trauma or twisting | Immediate | Pain with palpation of medial facet, lateral femoral condyle |
| Fractures | Trauma | Immediate | Unable to bear weight |
The mechanism of injury is extremely important in the diagnosis of knee injuries (Table 12–3). The injury can be acute or chronic. Most patients can recall the specific knee position during injury and the stresses incurred. Knee injuries can occur from contact forces as well as from falls and twisting injuries not involving contact. An audible ‘pop’ at the time of injury is characteristic of injury to the ACL. It is important to know whether the patient is able to walk following the injury, and whether the injury affects the range of motion of the knee. This information enables the clinician to determine the severity of the injury and the likelihood of intra-articular fractures. Injuries that prevent weight-bearing typically signify a fracture or other severe knee injury.
| Scenario | Concern |
|---|---|
| Fall from a height | Fracture |
| Twisting injury with foot planted | ACL with or without meniscal tear |
| Acute pain with deep flexion or twisting | meniscal tear |
| Lateral (valgus) blow to the knee | MCL injury |
| Medial blow (varus) blow | LCL injury |
| Anterior blow to the knee (dashboard injury) | PCL tear |
| Misstep with inability to straighten knee | Patella or quadriceps tendon rupture |
| Acute anterior pain and swelling with twisting motion | Patella dislocation |
| Gradual onset of discomfort and startup pain | Osteoarthritis or degenerative condition |
The patient should be in the supine position on a comfortable examination table. Since the injured knee may be swollen or locked and cannot be fully extended, a pillow can be placed behind the knee to relax it; another pillow can be placed behind the uninjured knee so that both knees can be inspected at the same angle. The uninjured limb should be examined first. Because there is little variation between right and left knees, the uninjured knee can serve as a good indicator for joint motion and laxity prior to injury.
After examining the uninjured knee, the injured knee should first be inspected for its skin integrity and any areas of ecchymosis. Loss of both active and passive range of motion can signify a chronic problem with contractures or a mechanical block, whereas loss of only active motion can signify pain or weakness. Location of pain should be noted during range of motion. For example, displaced meniscus tears can be painful during range of motion and can clue clinicians to the presence of medial or lateral injuries.
The presence and location of swelling is helpful in the evaluation of the acutely injured knee. The majority of acute knee swelling is secondary to hemarthrosis following intra-articular ligament tears, such as ACL tear and patella dislocation. An osteochondral fracture or peripheral tear of the meniscus can also produce a hemarthrosis. The swelling may take longer to occur if ice is applied to the knee immediately following injury. Immediate, brisk swelling should make the examiner suspicious of osteochondral fractures or ACL tears. When the effusion is drained, the presence of fat droplets signifies osteochondral fractures or nondisplaced intra-articular fractures. Swelling that occurs over the next 24 hours may represent meniscus tears or unstable cartilage injuries.
Patients who have difficulty with immediate weight-bearing should have orthogonal (anteroposterior and lateral) radiographs to rule out fractures. The Ottawa Knee Rules outline indications for obtaining radiographs to rule out fracture (Table 12–4). The Ottawa Knee Rules consist of 5 criteria; the absence of all 5 criteria rules out fracture with a sensitivity that approaches 100%.
|
MRI can be helpful in the evaluation of soft tissue injuries, such as ligament or meniscus injuries. MRI is 75–85% sensitive for detecting meniscal, ligamentous, or cartilage damage. The specificity, however, is lower because of frequent false-positives, particularly in older individuals. Abnormal MRI findings are common, even in asymptomatic knees. Therefore, MRI should be used to confirm a diagnosis rather than as the sole basis for a diagnosis.
Protected weight-bearing and brace for stabilization can be helpful following acute knee injuries and prior to definitive diagnosis and treatment. Fractures or severe ligament injuries should be referred to the specialists.
Most patients with injuries to collateral ligaments describe injuries on the side of the knee. A lateral blow to the knee leads to injury of the medial collateral ligament (MCL), whereas a medial blow leads to injury of the lateral collateral ligament (LCL).
When testing the MCL, the patient is asked to lie in a supine position with the hip abducted and the knee gently hanging off the edge of the examination table and flexed at 30 degrees. A valgus stress is applied through the examiner’s left hand, which supports the ankle. The examination is repeated at full extension. When examining the LCL, an adduction or varus stress is applied. The test is performed similar to the valgus stress test, only with a varus directed force and medial placement of the hand to counteract the stress. The test is performed at full extension and at 30 degrees of flexion.
MRI is rarely indicated for isolated MCL tears. It is uncommon to have meniscus injuries with MCL tears. However, the ACL can be injured with MCL tears, and these complex injuries should be evaluated by MRI. LCL injuries should necessitate MRI evaluation to determine the significance of injuries. MRI has 80% sensitivity and 90% specificity in the evaluation of acute collateral ligament injuries.
MCL injuries are commonly treated with immobilization and bracing. The majority of these injuries heal without the need for surgical stabilization. Grade III (more than 1 cm opening) injuries are treated with protected weight-bearing. LCL or lateral ligament complex injuries do not respond well to nonsurgical treatment and, when recognized, should be urgently referred to an orthopedic surgeon.
Typically, the history reveals a twisting injury while the foot is planted. A tear of the ACL can occur with either contact or non-contact mechanisms of injury. Patients commonly describe a ‘pop’ sound.
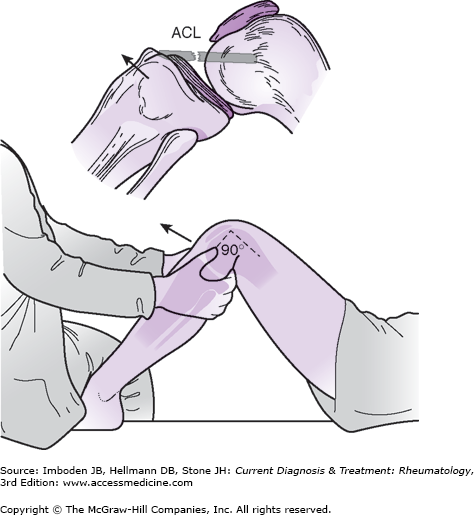
The Lachman or Ritchey test is a highly sensitive and specific method for assessing an ACL sprain or tear in the acute setting (Figure 12–2). It consists of an anteriorly directed force with the knee at 30 degrees of flexion; an increase in anterior translation of the tibia compared with the contralateral side constitutes a positive test and signifies injury to the ACL. The anterior drawer test is performed with the knee flexed at 90 degrees and the hip at 45 degrees (Figure 12–3). Difficulty with having the patient relax during the anteriorly directed force can limit the usefulness of this test. The pivot shift test is the most specific test for ACL tear but has low sensitivity for the awake patient. The sensitivity of the test is highly dependent on the examiner’s skill and the patient’s relaxation.
MRI is commonly needed to confirm the diagnosis. MRI of the ACL is 93% sensitive and nearly 100% specific. MRI also can identify associated injuries, such as meniscus tear and cartilage injuries, which can affect management.
The treatment of ACL tears varies on the basis of the needs and activity level of the patient. These injuries are best managed by consultation of an orthopedic surgeon or sports medicine clinician. The patient should be evaluated within 2–3 weeks following the acute injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree