Essentials of Diagnosis
- Chronic inflammatory arthritis associated with skin and nail psoriasis.
- Symmetric polyarthritis or asymmetric oligoarthritis of peripheral joints (frequently with distal interphalangeal [DIP] joint involvement).
- Spondylitis and enthesitis may occur.
- Current or past history of psoriasis; family history of psoriasis.
- Dactylitis and characteristic nail dystrophy.
- Absence of rheumatoid factor.
- Radiographic findings of erosions, osteolytic destruction of the interphalangeal joints, and juxta-articular new bone formation.
General Considerations
Psoriatic arthritis is a chronic inflammatory arthritis associated with skin and nail psoriasis. It is one of the spondyloarthropathies, a group of inflammatory arthritides, characterized by arthritis of the axial skeleton (ie, the sacroiliac joints and spine), asymmetric oligoarthritis or symmetric polyarthritis of peripheral joints, enthesitis (inflammation at the insertion sites of tendons to bone), and the absence of rheumatoid factor. Unlike rheumatoid arthritis, psoriatic arthritis has a predilection for the DIP joints.
Psoriatic arthritis develops in approximately 20–30% (range 6–42%) of adults with psoriasis. The overall prevalence of psoriatic arthritis in the general population has been estimated to be 0.04–0.1%, but this may be an underestimate. In the United States, the incidence of psoriatic arthritis has been reported to be approximately 6–7 per 100,000 per annum. The mean age of disease onset ranges from 30 to 55 years, with men and women equally affected.
Pathogenesis
The etiology of psoriatic arthritis is unknown. Genetic susceptibility studies indicate associations with major histocompatibility alleles HLA-B27, HLA-B7, HLA-B13, HLA-B17, HLA-B57, and HLA–Cw*0602. Recent genome-wide association studies of patients with psoriasis and psoriatic arthritis have identified other susceptibility loci, including interleukin (IL)-23A, IL-23R, IL-12B, tumor necrosis factor-induced protein 3 (TNFIP3), TNFIP3 interacting protein 1 (TNIP1), IL-4, IL-13, and tumor necrosis factor receptor-associated factor 3-interacting protein 2 (TRAF3IP2). As in the pathogenesis of many other autoimmune disorders, an infectious trigger has been suspected. Group A streptococcal infections have been implicated in guttate psoriasis, and ribosomal RNA from this species has been detected in peripheral blood and synovial fluid of psoriatic arthritis patients. In addition, HIV is strongly associated with the development of psoriasis and psoriatic arthritis. Physical trauma (Koebner phenomenon) has also been implicated.
Psoriatic arthritis typically develops after or coincident with the onset of psoriasis. In 15–20% of cases, however, arthritis precedes the onset of psoriasis by as much as 2 years. An asymmetric oligoarthritis was once believed to be the usual clinical presentation of psoriatic arthritis, but recent evidence supports that symmetric polyarthritis is the most frequent presentation. Widespread destructive arthritis (arthritis mutilans) and mostly DIP joint involvement are observed less frequently but are more specific to psoriatic arthritis. The pace of joint destruction may occur over a period of months.
There may be a direct correlation between the severity of arthritis at the time of presentation and the subsequent disease course. Polyarthritis in the presence of elevated acute phase reactants, radiographic evidence of joint erosions, and inadequate response to initial pharmacotherapy predicts a more severe disease course. As seen in rheumatoid arthritis, psoriatic arthritis can significantly impact quality of life and physical function. Articular damage often develops, and destruction of single joints can occur rapidly.
Clinical Findings
The majority of patients with psoriatic arthritis have symmetric polyarthritis or asymmetric oligoarthritis of the hands and feet. Often the DIP joints become stiff, swollen, and tender in an asymmetric fashion. When present, involvement of the DIP joints helps distinguish psoriatic arthritis from rheumatoid arthritis, but sometimes results in confusion with osteoarthritis or gout. Other joints that are affected by psoriatic arthritis include the knees, hips, and sternoclavicular joints.
Regardless of the number of symptomatic joints at disease onset, most patients progress to additional joint involvement in the absence of effective treatment. There is ongoing destruction of joints, as evidenced clinically by the appearance of joint deformities and radiographically by the development of juxta-articular erosions, joint-space narrowing, and, in some cases, bony ankylosis. Arthritis mutilans describes the end stage of the destructive process, where loss of bony architecture allows complete subluxation and telescoping of the involved digit (“doigt en lorgnette” or opera-glass finger). This phenomenon is uncommon and is associated with long-standing, poorly controlled disease.
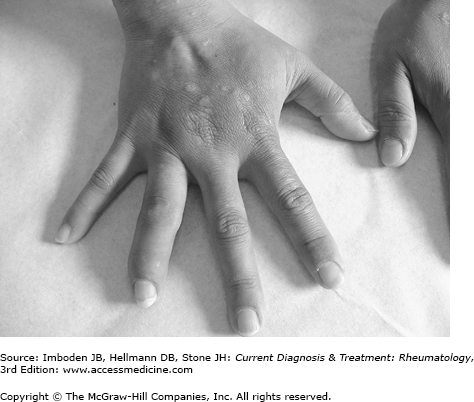
Dactylitis, or “sausage digit,” is the complete swelling of a single digit of the hand or foot (Figure 19–1). It is a distinctive feature of the spondyloarthropathies, and it is common in psoriatic arthritis, occurring in one-third to one-half of patients at some point during the course of the disease. Toes are more frequently involved than fingers. Dactylitis is associated with more severe radiographic joint damage.
Enthesitis is an inflammatory process occurring at the site of insertion of tendons into bone. This is a feature common to other spondyloarthropathies and occurs in up to 40% of psoriatic arthritis patients. On physical examination, there is a soft tissue swelling usually accompanied by tenderness to palpation and sometimes by overlying erythema and warmth as well. Common sites for enthesitis are the Achilles tendon, plantar fascia, and pelvic bones. Entheseal inflammation may evolve to destruction of the adjacent bone and joints.
All forms of psoriasis are associated with arthritis, although classic psoriasis vulgaris is seen most frequently. Typical psoriatic lesions are erythematous plaques that produce scaling with scratching. Interestingly, many patients with psoriatic arthritis have only mild to moderate skin disease, and there has been no consistent correlation between the degree of psoriasis and the extent of joint involvement. The psoriasis may be subtle. Therefore, careful examination of the entire skin surface must be performed when psoriatic arthritis is suspected, with particular attention to the hairline, scalp, external auditory canal, periumbilical area, and gluteal cleft.
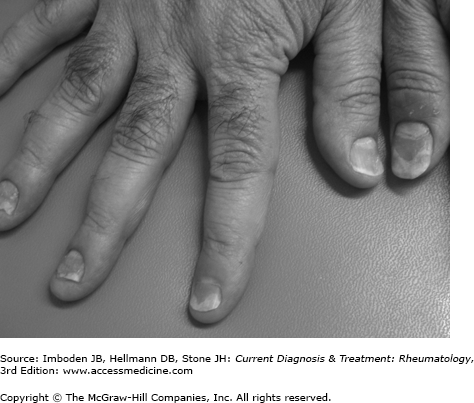
As with uncomplicated psoriasis, nail involvement is common in psoriatic arthritis (Figure 19–2). Psoriatic nail changes include ridging, pitting, onycholysis, and hyperkeratosis, and may represent the manifestation of psoriasis before the presence of more characteristic skin lesions. Nail changes on the affected finger virtually always occur when psoriatic arthritis affects a DIP joint.
Symptomatic involvement of the sacroiliac joints and axial skeleton is less common than peripheral joints. Inflammation of the sacroiliac joints (sacroiliitis) in psoriatic arthritis is usually unilateral and presents with pain and stiffness in the lower back or buttock. Tenderness can sometimes be elicited by direct palpation of the joints by applying firm pressure with the thumbs when the examiner places his or her palms over the patient’s iliac crest—the thumbs will tend to fall directly over the joints. Another maneuver that may detect sacroiliitis is the Gaenslen test, in which the patient (in either the supine or the lateral recumbent position) flexes one leg at the hip with the knee close to the chest and hyperextends the other leg over the examination table. This applies stress to the sacroiliac joints and is considered positive if pain is elicited at the sacroiliac joint. However, the reliability of physical examination findings for detection of sacroiliitis is poor, and noninflammatory processes may elicit positive findings. Plain radiography of the pelvis and Ferguson views that focus on the sacroiliac joints may aid in the detection of inflammatory disease of this joint.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree