Aortic Arch and Pulmonary Artery Abnormalities
W. Robert Morrow
Anomalies of the aortic arch and pulmonary arteries constitute a diverse group of malformations. The range of possible deviations from normal morphology of the aortic arch and pulmonary artery is broad. Vascular rings are formed when one or more aortic arch anomalies, with or without a patent ductus arteriosus or ligamentum, produce a ring that completely encircles the trachea and esophagus, leading to symptoms of tracheal or esophageal constriction. A vascular sling, produced by an abnormal origin and course of the left pulmonary artery or left ductus arteriosus, does not encircle the trachea and esophagus completely but usually produces severe symptoms of tracheal and bronchial compression.
PATHOGENESIS
Most anomalies of the aortic arch can be described by postulating the regression of a segment of the arch that normally persists or, conversely, the persistence of a segment of the arch that normally regresses. In this concept, the normal left aortic arch develops by regression of the eighth segment of the embryonic right dorsal aorta. The remaining elements of the right aortic arch contribute to development of the right innominate artery and the primitive right subclavian artery. Normally, the right ductus arteriosus regresses, eliminating continuity of the right sixth aortic arch with the aorta. A double aortic arch is postulated to result from the persistence of both paired dorsal aortic arches.
A right aortic arch may form by one of two mechanisms, giving rise to a right aortic arch with or without mirror-image branching. A right aortic arch with mirror-image branching occurs when the left eighth dorsal aortic arch segment regresses. When regression of the left arch occurs between the left carotid artery and the left subclavian artery (left fourth primitive aortic arch), the latter arises from the descending aorta and courses posterior to the esophagus. In this situation, the ductus arteriosus arises from the descending aorta at the base of the left subclavian artery or from a retroesophageal diverticulum and produces a vascular ring completely encircling the esophagus and trachea. Regression may occur between the right carotid artery and the right subclavian artery, giving rise to an anomalous origin of the right subclavian artery from the descending aorta. A cervical aortic arch probably results from the persistence of the third primitive aortic arch, with regression of the contralateral arch between the carotid artery and the subclavian artery (fourth primitive arch).
An anomalous origin of the left pulmonary artery, unilateral absence of one pulmonary artery, and unilateral origin of one pulmonary artery from the ascending aorta result from the abnormal regression of the left proximal sixth arch. The unilateral origin of one pulmonary artery from the ascending aorta may result from a malalignment of the conotruncal ridges. With septation of the truncus arteriosus, one pulmonary
artery maintains connection with the ascending aorta, and the other is connected to the main pulmonary artery.
artery maintains connection with the ascending aorta, and the other is connected to the main pulmonary artery.
Aortic Arch Anomalies
Left Aortic Arch with Anomalous Right Subclavian Artery
Left aortic arch with anomalous origin of the right subclavian artery is the most common aortic arch malformation noted on postmortem examination. The incidence of this abnormality in the general population is approximately 0.5%. The left arch has a normal course to the left and anterior to the trachea, but the right subclavian artery arises as the last branch of the arch and courses posterior to the esophagus. Most patients with anomalous right subclavian artery are asymptomatic, and the abnormality is discovered incidentally at esophagography or at catheterization. Often, an anomalous right subclavian artery is seen in patients with tetralogy of Fallot and left aortic arch and, therefore, has a significant bearing on which systemic-to-pulmonary artery shunt is chosen for palliation of cyanosis. In addition, an anomalous right subclavian artery may be present in patients with coarctation of the aorta, and it often arises distal to the site of coarctation. In these patients, blood pressure in the right arm and legs does not reflect the coarctation gradient. It is necessary, then, to determine blood pressure in both arms and in the legs during the examination of patients with suspected coarctation.
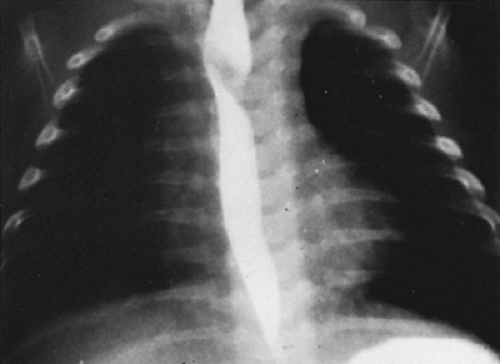
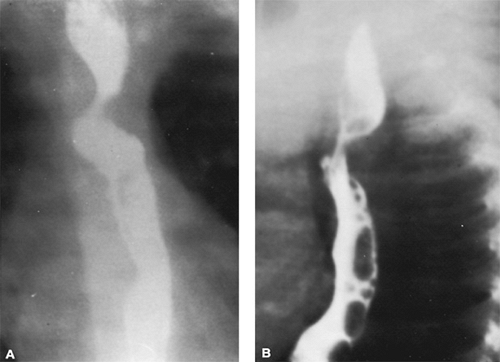
Although most patients with an anomalous right subclavian artery are asymptomatic, some older children and adults may experience dysphagia. Routine chest radiography does not demonstrate this anomaly, but barium esophagography is diagnostic. The oblique course of the anomalous vessel posterior to the esophagus in the anteroposterior projection and the posterior indentation of the esophagus in the lateral or left anterior oblique projection usually are diagnostic (Fig. 280.1). The diagnosis of an anomalous right subclavian artery may be made using two-dimensional echocardiography when the first branch of the aorta is to the right, but the normal bifurcation into a right carotid artery and right subclavian artery cannot be demonstrated. An anomalous right subclavian artery may be noted incidentally when aortography is performed in patients with congenital heart disease.
If symptoms of a vascular ring (e.g., stridor, wheezing, cough) are present in a patient with an anomalous right subclavian artery, an alternative diagnosis, such as laryngomalacia or tracheomalacia, should be considered. Rarely, an anomalous right subclavian artery in association with a left aortic arch, retroesophageal descending aorta, and right ductus arteriosus or ligamentum produces a symptomatic vascular ring. The retroesophageal descending aorta in these patients results in a large, rounded, posterior indentation on barium esophagogram, which usually is distinguished readily from the more shallow indentation produced by an anomalous right subclavian artery without a retroesophageal descending aorta. The diagnosis should be confirmed by magnetic resonance imaging (MRI).
Double Aortic Arch
The double aortic arch is the most common clinically recognized form of vascular ring. The ascending aorta divides anterior to the trachea into left and right arches, which then pass on either side of the trachea. Usually, the right arch is larger than is the left, and it passes posterior to the esophagus to join the descending aorta to the left of the midline. Uncommonly, the left arch is atretic. A complete vascular ring is formed by the arches on each side of the trachea and esophagus, with the ascending aorta anterior and the retroesophageal arch or descending aorta posterior. Usually, the ductus arteriosus is left-sided and is not an essential component of the vascular ring, but the length of the ductus arteriosus or ligamentum may affect significantly the severity of symptoms. Usually, associated congenital heart disease is not present, but it may occur in as many as 22% of patients. Cyanotic congenital heart disease, including tetralogy of Fallot and transposition of the great arteries, predominates.
Usually, patients with a double aortic arch are severely symptomatic in infancy, with stridor, dyspnea, cough, and recurrent respiratory infections. Infants feed poorly because of severe respiratory distress and may prefer to assume an opisthotonic posture. Life-threatening episodes of apnea with cyanosis may occur. The diagnosis of a double aortic arch, like almost all vascular rings, often is suggested by the presence of a right aortic arch on routine chest radiography. In patients with a double aortic arch, both arches sometimes are seen, and evidence of hyperinflation of either or both lungs caused by obstruction of the lower trachea and mainstem bronchi may be present.
Barium esophagography often demonstrates bilateral indentations of the esophagus in the anteroposterior projection (Fig. 280.2) but may show only a prominent right-sided indentation. When two indentations are seen, usually the right arch produces the larger and more superior indentation. In the lateral or left anterior oblique projection, a large posterior indentation is seen and represents the retroesophageal component of the arch. Also present is an anterior and more inferior indentation of the arch produced by posterior deviation of the trachea. Although surgery may be performed without additional imaging studies, confirmation of the diagnosis can be obtained by MRI, echocardiography, or angiography. MRI provides sufficient anatomic detail to perform surgery and may even demonstrate tracheal compression (Fig. 280.3).
Usually, stridor and respiratory distress are severe, and affected infants will die without early surgical intervention. The mortality rate from surgery is low, and usually eventual
long-term relief of symptoms is achieved. However, short-term postoperative tracheal obstruction is the rule, and some infants require prolonged intubation and aggressive attention to pulmonary toilet in the early postoperative period. Stridor may persist to some degree for months after surgery.
long-term relief of symptoms is achieved. However, short-term postoperative tracheal obstruction is the rule, and some infants require prolonged intubation and aggressive attention to pulmonary toilet in the early postoperative period. Stridor may persist to some degree for months after surgery.
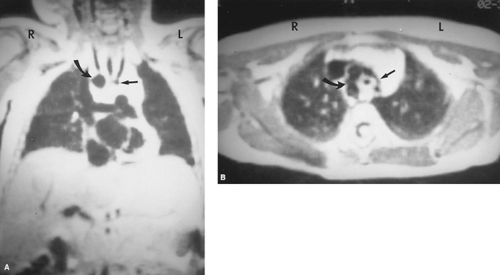 FIGURE 280.3. T1-weighted gated magnetic resonance imaging in a patient with a double aortic arch. A: Coronal images demonstrate both the major arch on the right (curved arrow) and the minor arch on the left (straight arrow). B: In the axial plane, the vascular ring is demonstrated partially, and the major arch on the right (curved arrow) and the minor arch on the left (straight arrow) are seen clearly. The position of the trachea in the center of this ring is seen as the small, dark, circular area of signal loss. (Courtesy of Dr. Gary Hedlund, The Children’s Hospital, Birmingham, AL.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|