Anterior Interbody Arthrodesis with Instrumentation for Scoliosis
Janay E. Mckie
Daniel J. Sucato
DEFINITION
Thoracic scoliosis and thoracolumbar-lumbar scoliosis are typical curves seen in idiopathic scoliosis and can be treated anteriorly.
Anterior arthrodesis refers to the fusion of the anterior part of the vertebral bodies, usually with instrumentation for these curve patterns.
ANATOMY
Thoracic idiopathic scoliosis usually has an apex at T8 or T9. It is most commonly a right convex curve pattern and has axial plane rotational deformity as well as hypokyphosis.
Thoracolumbar-lumbar scoliosis has an apex of the curve at T12 or below and is most commonly a left-sided curve, with or without a compensatory thoracic curve.
The vertebral bodies are nearly normal in their shape, although some distortion of the vertebral body and pedicles is seen, with thin, long pedicles on the concavity and shorter, wider pedicles on the convexity.
PATHOGENESIS
The cause of idiopathic scoliosis is not yet known.
NATURAL HISTORY
Idiopathic scoliosis progresses with continued growth of the spine, especially during the peak growth periods and when the curve magnitudes are “large” at the completion of growth.
Thoracic curves tend to progress at skeletal maturity when the curve is greater than 45 to 50 degrees.
Thoracolumbar-lumbar curves tend to progress when the curve is greater than 35 to 40 degrees at the time of skeletal maturity.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patients with thoracic scoliosis and thoracolumbar scoliosis should be evaluated for their perception of spine and body deformity to include asymmetric shoulder elevation, trunk shift, waistline asymmetry, and rib or flank prominence.
Pain in the axial spine and pain radiating into the lower extremities should be ascertained with a good history; such symptoms warrant a magnetic resonance imaging (MRI).
Neurologic symptoms such as paresthesias, hyperesthesia, or bowel or bladder symptoms are relevant and require further imaging with an MRI.
Physical examination should assess the trunk imbalance in the coronal plane, which can be seen with isolated thoracic or thoracolumbar-lumbar curves.
The Adams forward bend test characterizes the axial plane deformity seen in scoliosis and is used to assess rotational deformity of the thoracic rib prominence or the flank prominence. The rotational deformity of the thoracic and lumbar spine is graded using a scoliometer with the patient bending forward. The rotational deformity seen in scoliosis can be very prominent and the most obvious deformity seen by patient and families.
Cutaneous manifestations of dysraphism should also be analyzed.
IMAGING AND OTHER DIAGNOSTIC STUDIES
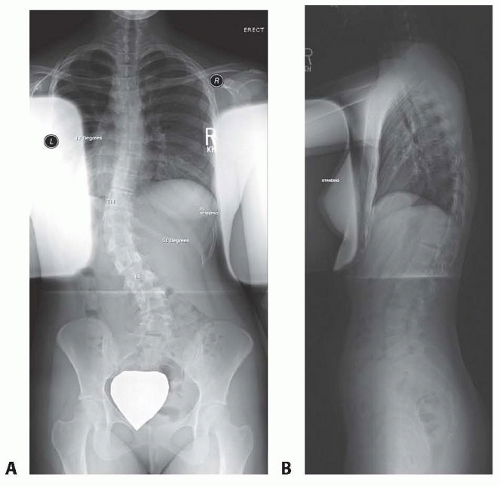
Anteroposterior (AP) and lateral radiographs of the spine should be obtained to review the coronal and sagittal plane deformities, respectively (FIG 1).
On the AP radiograph, the coronal plane deformity is measured using the Cobb method. Truncal imbalance can be measured using the Floman method (bisecting the distance between the lateral rib margins and comparing this point to the center sacral vertical line [CSVL]).
The decompensation of the head relative to the pelvis is measured by the distance between the C7 plumb line and the CSVL.
The Risser sign should be evaluated by assessing the ossification of the iliac apophysis, giving it a grade between 0 and 5.
The triradiate cartilage status should be assessed as either open or closed.
The lateral radiograph is used to measure thoracic kyphosis (measured from T5 to T12) and lumbar lordosis (from L1 to S1) as well as the sagittal balance (comparing a C7 plumb bob line to the front edge of S1).
Supine best-bend radiographs can be used to determine the flexibility of the spine and are especially useful to determine whether the thoracolumbar-lumbar curve is flexible when a primary thoracic curve is present or if the thoracic curve is flexible and compensatory when the primary thoracolumbar-lumbar curve is present.
DIFFERENTIAL DIAGNOSIS
Idiopathic scoliosis should be differentiated from other types of scoliosis in which congenital abnormalities are not seen in ambulatory patients. This list includes, but is not limited to, neurofibromatosis, Marfan syndrome, type 3 spinal muscular atrophy, scoliosis associated with syringomyelia, or tethered cord.
NONOPERATIVE MANAGEMENT
Adolescent thoracic and thoracolumbar scoliosis can be treated with bracing when curve magnitudes are between 25 and 45 degrees during peak growth periods.
Bracing is used for these curve magnitudes to prevent curve progression and is indicated in Risser grade 0 to 2 patients.
Nonoperative management is primarily indicated when the cosmetic appearance of the patient is acceptable to him or her.
SURGICAL MANAGEMENT
Surgical indications for thoracic idiopathic scoliosis are curves exceeding 45 to 50 degrees with unacceptable cosmetic deformity.
Surgical indications for thoracolumbar-lumbar curves are curves exceeding 40 to 45 degrees with unacceptable cosmetic deformity with a compensatory thoracic curve.
Preoperative Planning
A careful physical examination as noted earlier is necessary to ensure that there are no neurologic signs or symptoms, which would indicate neural axis abnormalities. If these are present, MRI of the neural axis is indicated.
Radiographic imaging should be used to ensure the curve is characteristic of an idiopathic curve. For thoracic curve patterns, this should demonstrate apical lordosis. The atypical curves, such as left-sided thoracic curves or those with significant decompensation despite minimal rotational deformity, or patients who have excessive thoracic kyphosis should be further evaluated with an MRI.
The AP radiograph, the lateral standing radiograph, and the supine best-bend radiograph should be used to determine the Lenke classification.
Specific detailed analysis of the compensatory curves should be performed to fine-tune a surgical plan to ensure that postoperative decompensation does not occur. This is especially important to determine the flexibility of the lumbar curve and the lumbar modifier for primary thoracic curves as well as the flexibility of the compensatory thoracic curve for primary thoracolumbar-lumbar curves.
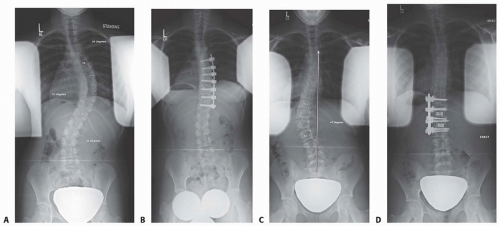
Anterior fusion levels for thoracic scoliosis are, in general, proximal end vertebra to distal end vertebra. Occasionally, a parallel disc is noted at the distal segment. It is controversial whether this disc should be included in the fusion levels. When the curve is relatively small (50 to 60 degrees) and flexible (>50% flexibility index) and the patient is skeletally mature (triradiate cartilage is closed and Risser grade 1 or higher), inclusion of the parallel disc is not often necessary (FIG 2A,B).
Anterior fusion levels for thoracolumbar-lumbar curves in general are proximal end vertebra to distal end vertebra. When the disc below the planned lowest instrumented vertebra is reversing and opening into the fractional lumbosacral curve, then disc wedging is not seen postoperatively. However, a disc below the lowest instrumented vertebra that is parallel preoperatively will often be wedged postoperatively (FIG 2C,D).
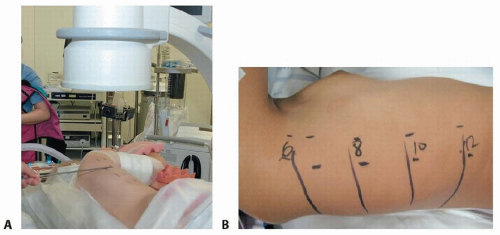
Positioning
Positioning for anterior surgery for either the thoracic or thoracolumbar curves is fairly similar. Patients are placed in the lateral decubitus position with the convex side of the curve up.
An axillary roll is used for safe upper extremity neurologic function (FIG 3).
An inflatable beanbag is used to position the patient, and body positioners can be added for further patient stabilization.
For thoracolumbar-lumbar curves, a table that can be flexed allows for greater access to the abdomen and spine. It should be centered over the apex of the curve.
For thoracic scoliosis surgery, the patient can be placed on a flat radiolucent table.
Approach
The anterior approach is used for thoracic scoliosis.
TECHNIQUES
▪ Open Thoracic Anterior Instrumentation and Arthrodesis
A curved incision is made over the proximal rib corresponding to the proximal fusion level (ie, commonly T5 with the fifth rib). The incision is carried through the thoracic and abdominal musculature to the periosteum of the rib.
Subperiosteal dissection of the rib is performed circumferentially, and the rib is cut posteriorly and anteriorly.
The parietal pleura is incised in a longitudinal fashion over the vertebral bodies across the intended levels of instrumentation and fusion.
The segmental vessels can be temporarily ligated and spinal cord monitoring should be observed during temporary ligation.
Permanent ligation can be performed after 20 minutes of normal spinal cord monitoring.
Discectomy is performed (see the section on the thoracoscopic technique).
Instrumentation is placed (see the following text).
For the remaining procedures, see details under the thoracoscopic approach.
▪ Thoracoscopic Anterior Instrumentation and Arthrodesis
Positioning, Preparation, and Draping
After true lateral positioning is confirmed, fluoroscopy is used to mark the skin for the proximal end vertebra and distal end vertebra on the AP view. The skin markings are made to identify the angle of the proximal end vertebra on the AP view (TECH FIG 1).
The anterior and posterior edges of the vertebral bodies are then marked using the lateral fluoroscopy view.
The chest and flank are prepared and draped in the normal sterile fashion.
Thoracoscopic Portal and Guidewire Placement
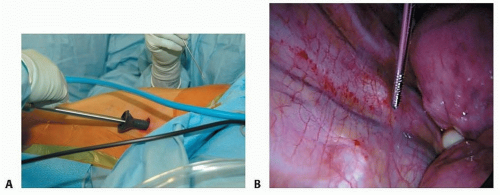
An anterior portal is placed, bisecting the distance between the proximal and the distal intended instrumented vertebra, in the anterior axillary line. This portal is used for placement of the camera (TECH FIG 2A).
A guidewire is then placed directly over the vertebral bodies over the intended second most proximal portal and is visualized
with the thoracoscope placed in the anterior portal (TECH FIG 2B).
After good placement of the guidewire (directly over the rib head), the portal is placed with a transverse incision centered over the rib. This portal can be used for visualization with a thoracoscope to place the remaining portals.
The most proximal posterolateral portal is placed after the intended second posterolateral portal to ensure exact location of the proximal portal. The proximal portal position is most important because the most proximal two screws are often placed in small vertebral bodies and have significant coronal angulation, and retraction of the scapula makes this portal difficult.
The remaining portals are placed in the posterolateral line.
The portals will house the camera, a fan retractor to retract the lung, a suction device, a working portal, and then a free portal.
Discectomy Technique
The pleura is incised in the midvertebral line in a longitudinal fashion, keeping the segmental vessels intact (TECH FIG 3A).
The segmental vessels are then ligated two or three at a time (normotensive anesthesia is used for anterior surgery).
The parietal pleura is retracted anteriorly, all the way to the opposite side, and access to the anterior longitudinal ligament and the contralateral annulus is allowed (TECH FIG 3B).
Posterior retraction allows for identification of the rib heads (TECH FIG 3C).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree