Anterior Drainage of the Septic Hip in Children
Richard M. Schwend
DEFINITION
Septic arthritis of the hip affects children of all ages, from the newborn to adolescents. The principles of treatment include early and accurate diagnosis, prompt surgical drainage, appropriate antibiotic coverage, and judicial management of late sequelae. The worse outcomes occur when there has been a marked delay in the diagnosis.
ANATOMY
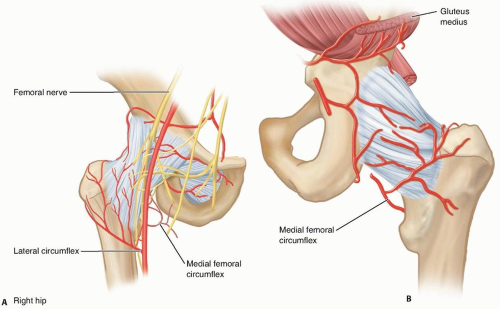
Synovial membrane with its rich blood supply lines the joint capsule.
Blood supply to the hip is from the medial and lateral femoral circumflex vessels (FIG 1).
Intra-articular retinacular vessels travel up the femoral neck and enter the femoral head. These vessels do not cross the proximal femoral physis.
Because the proximal femur is an intra-articular metaphysis, primary femoral osteomyelitis in this location can decompress into the hip joint.
Many muscles that are in close proximity to the hip joint, including iliopsoas, piriformis, and obturator internus and externus, may develop pyomyositis or an abscess; this can mimic septic hip arthritis.
PATHOGENESIS
Bacteria can enter the hip joint cavity directly via the hematogenous route to the subsynovial layer of the capsule or indirectly from the proximal femoral metaphysis and occasionally from adjacent acetabular infection.
Polymorphonuclear cells enter the joint cavity with plasma proteins and inflammatory fluid.
The resulting tense effusion can increase intracapsular pressure.
Articular cartilage destruction occurs from proteolytic enzyme degradation from cells of the synovial membrane and from interleukin-1 from monocytes, which releases proteases by chondrocytes and synoviocytes.
Animal studies show that proteoglycan matrix can be lost by 5 days and collagen by 9 days after an infection starts.4 Antibiotics do not completely prevent this degradation if treatment is delayed.
NATURAL HISTORY
Although most patients have excellent outcomes, the hip joint accounts for about 75% of published reports of poor outcome from septic arthritis.
Poor results occur more frequently in infants younger than 6 months of age, if there is a delay in treatment of greater than 4 days, and with associated proximal femoral osteomyelitis and infection with Staphylococcus aureus.6
Over the past several decades, there has been an increase in the incidence and the severity of musculoskeletal infections. Commonly, there is a spectrum of infections in which septic arthritis may occur with osteomyelitis, pyomyositis, and deep and superficial abscesses.
During this time, there has been an increase in the incidence of methicillin-resistant Staphylococcus aureus (MRSA) infections, leading to severe complications such as deep venous thrombosis, septic emboli, and life-threatening multisystem organ failure.11
The most severe sequelae are more often seen in newborns and infants.
A frequent scenario when there is a poor outcome is the failure to make the diagnosis of septic hip arthritis, either from not recognizing the serious nature of the condition or failure to promptly perform adequate surgical drainage and administer appropriate intravenous antibiotics.
PATIENT HISTORY AND PHYSICAL FINDINGS
The history should include a detailed timeline of events leading up to presentation.
In the most recent prospective studies evaluating clinical predictors for septic hip arthritis, a fever above 38.5° C was the strongest predictor.1, 8, 9
The severity of pain, particularly pain at rest and night pain, indicates inflammation.
Associated illnesses and infections, history of trauma to the hip, recent dental procedures, and underlying medical conditions or steroid use may lead to infection in a susceptible host.
Always ask about recent antibiotic treatment because this may mask many of the findings of septic hip arthritis and change the threshold for obtaining imaging studies and for performing hip aspiration.
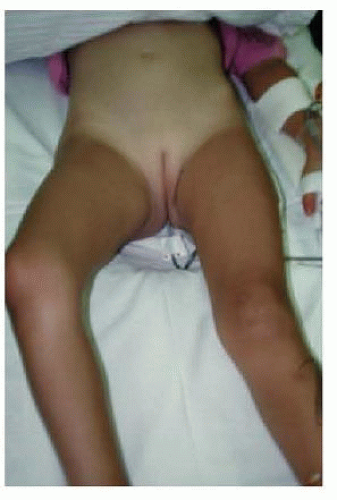
Conduct a visual inspection with the child lying supine on the table, noting whether the hip is in abduction, flexion, and external rotation (FIG 2).
A septic hip joint assumes this position of least intracapsular pressure.
Inspect for skin rash, erythema, warmth, swelling, and tenderness over overlying muscles and the hip joint.
The clinician should palpate the pelvis and lower extremities for local swelling and tenderness.
Examine the child walking. Antalgic limp indicates that the patient is unable to spend much time weight bearing on the hip joint. The child may have mild pain early or the pain may be so severe that the patient is unable to walk.
Observe the hip range of motion. Gradually, there is limited ability to move the hip joint as inflammation and pressure of the hip joint increase. Pain with hip extension and internal rotation suggests involvement of the psoas muscle.
Inspect and palpate the spine. Septic discitis in a young child can present as refusal to walk and can resemble septic hip arthritis.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Imaging and laboratory studies are determined by the clinical evaluation, probability of the findings being septic hip arthritis, and need to exclude other conditions.
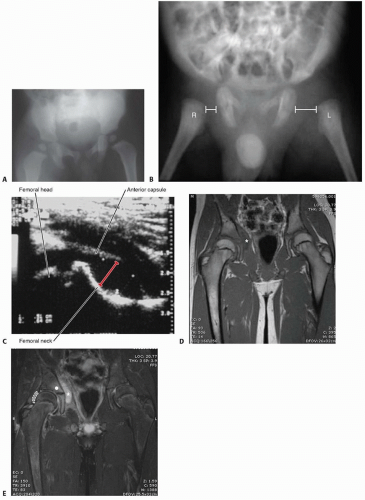
Plain radiographs (FIG 3A)
Key features include hip abduction, increased soft tissue density, widened medial joint space, osteopenia if the infection is long-standing, and femoral or acetabular osteolytic lesions.
A particularly worrisome finding in the neonate is a painful dislocated hip (FIG 3B). Bone lesions and destruction are typically delayed 1 to 2 weeks.
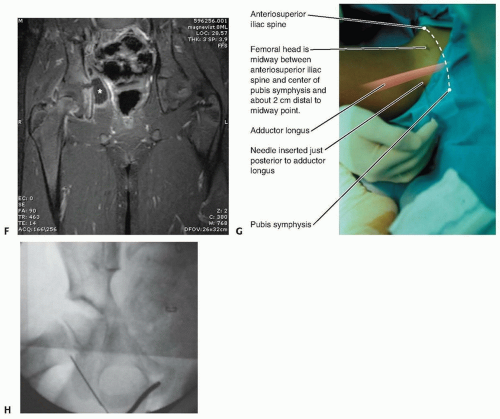
Ultrasound imaging (FIG 3C) is performed bilaterally, with images obtained along the axis of the anterior femoral neck. This is very specific for detecting intra-articular fluid in the hip.
Because the pelvis is deep and difficult to examine, magnetic resonance imaging (MRI) is an extremely useful imaging modality to examine the tissues surrounding the hip joint or within the pelvis (FIG 3D-F).
It is the preferred imaging technique if the hip joint moves better than would be expected for septic hip arthritis but the patient has symptoms within or near the pelvis suggesting myositis or an abscess.7, 13
MRI is useful if by 48 hours there is an inadequate response to treatment of septic hip arthritis, suggesting persistent hip joint infection, pelvic osteomyelitis, or infection in the muscles near the hip joint.
With the changing clinical spectrum of musculoskeletal infections, the severity of infections is increasing. MRI is becoming the preferred imaging modality to provide detailed anatomy, clinical classification, and clarify early surgical decision making.5
A bone scan is not generally recommended. If the patient has a septic hip arthritis, he or she should be in the operating room, not the nuclear medicine department.
White blood cell (WBC) count is always done but may not always be elevated in septic hip arthritis.
Blood culture is positive in 40% to 50% of cases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree