Anterior Cruciate Ligament Reconstruction: Single-Bundle Transtibial Technique
Introduction
Surgical reconstruction of the anterior cruciate ligament (ACL) is recommended for active patients.
Restores instability and normal knee kinematics
Improves function and return to active lifestyle
Benefits of bone–patellar tendon–bone (BPTB) autograft
Biomechanical strength
Accessibility and ease of graft harvest
Bone-to-bone healing
Rigid initial interference screw fixation
Track record of clinical success
Patient Selection
Indications
Younger than 40 years with an active, athletic lifestyle
Other considerations—Type of sports involvement, hours per week played, concomitant meniscal pathology, failure of nonsurgical care, ability to participate in postoperative physical therapy
Delay surgery until postinjury effusion has fully resolved and patient has attained full range of motion.
Contraindications
Open physes
Symptomatic preoperative patellar tendon disease or patellar malalignment
Relative contraindications—Degenerative joint disease, sedentary lifestyle, inability to comply with postoperative rehabilitation protocol
Preoperative Imaging
Radiography
Weight-bearing AP in full extension
Weight-bearing PA 45° flexion
Non–weight-bearing 45° flexion lateral
Merchant view
KT-1000 arthrometer (MEDmetric) used by authors to assist in physical examination diagnosis; anterior translations greater than 10 mm or side-to-side differences exceeding 3 mm are highly suggestive of ACL tear.
MRI
Use as an adjunct to history and physical examination to support diagnosis.
Sensitive and specific for ACL tears
Provides information about status of other intra-articular structures, such as the menisci, posterior cruciate ligament, medial collateral ligament, lateral collateral ligament, and chondral surfaces, as well as bone bruises
| Video 16.1 Anterior Cruciate Ligament Reconstruction: Single-Bundle Transtibial Technique. Eric J. Strauss, MD; Adam Yanke, MD; Bernard R. Bach, Jr, MD (19 min) |
Procedure
Room Setup/Patient Positioning
Supine position; waist of operating table is reflexed to reduce lumbar extension.
Examination under anesthesia
Lachman test
Varus/valgus knee stability
Pivot shift test; if positive, BPTB graft harvest can proceed before diagnostic arthroscopy.
Assessment of posterolateral corner
Tourniquet applied (rarely inflated)
Contralateral leg in gynecological leg holder
Surgical leg in arthroscopic leg holder with foot of table flexed completely to allow the surgical knee to flex to at least 110°
Special Instruments/Equipment/Implants
Standard arthroscopy instruments, including arthroscopic scissors and a basket
Graft harvest—No. 10 scalpel, forceps with teeth, two Senn retractors, an Army-Navy retractor, a metal ruler, 3/8- and 1/4-in curved osteotomes, mallet, Metzenbaum scissors
Graft preparation
Rongeur
10- and 11-mm sizing tubes
Kirschner wire (K-wire) driver with 0.062-in smooth K-wires
Two No. 5 sutures
Tibial tunnel
Tibial aiming device
11-mm acorn reamer
Chamfer reamer
Hand rasp
Femoral tunnel
7-mm offset aimer
10- and 11-mm acorn reamers
Notch preparation
Large shaver
Curved 7-mm osteotome
Large spherical burr
Graft passage—Satellite pusher
Graft fixation
14-in hyperflex nitinol wire
7- × 25-mm metal interference screw for femoral tunnel
9- × 20-mm metal interference screw for tibial tunnel
Surgical Technique
Graft Harvest
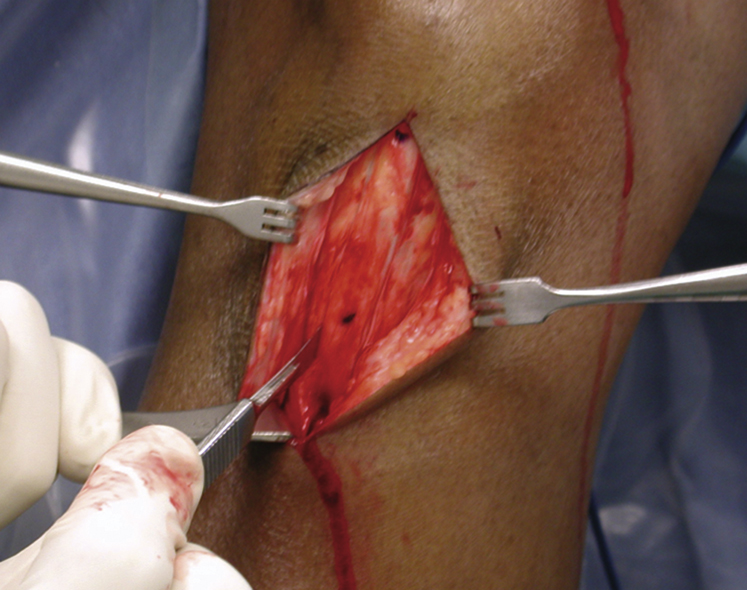
Figure 1Intraoperative photograph shows a central-third bone–patellar tendon–bone autograft harvest using a No. 10 scalpel blade starting on the patella and continuing into the patellar tendon.
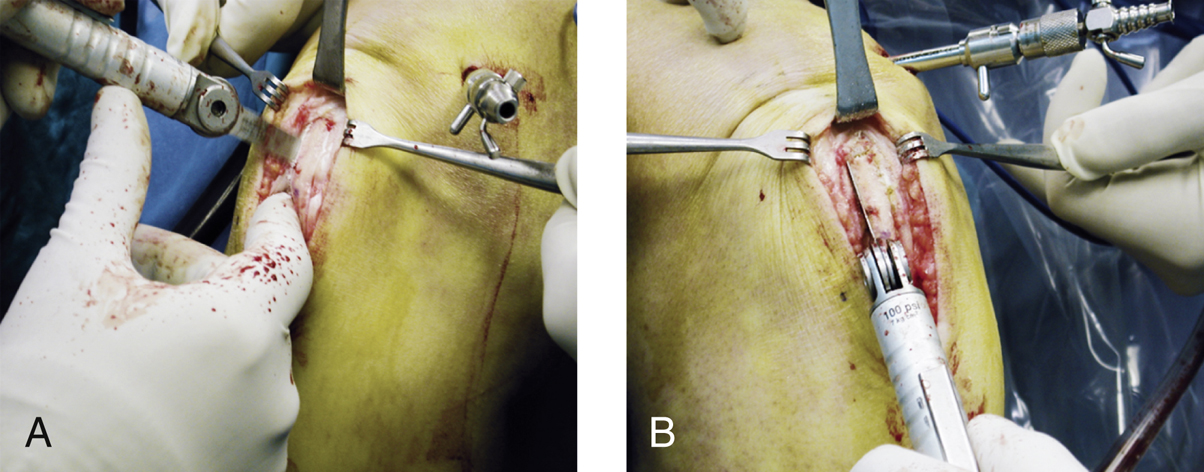
Figure 2Intraoperative photographs depict bone cuts made using an oscillating saw with a 10-mm (No. 238) blade. Cuts on the right side are made with the saw in the surgeon’s right hand (A) and those on the left are made with the saw in the surgeon’s left hand (B).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


