Anterior Cervical Diskectomy and Fusion
Patient Selection
Anterior cervical diskectomy and fusion was first described in the 1950s for treatment of cervical radiculopathy
Categorize symptoms and examination findings into axial neck pain, radiculopathy, and myelopathy, or a combination of the three
Indications for Treatment of Cervical Radiculopathy
Failure of a 3-month trial of nonsurgical methods to relieve radicular upper extremity pain with or without neurologic deficit
Presence of a progressive neurologic deficit
Neuroradiographic findings must be consistent with signs and symptoms
Indications for Treatment of Cervical Myelopathy
Progressive myelopathy
Moderate or severe myelopathy, even if stable and of short duration (<1 year)
Mild myelopathy that affects activities of daily living
Emphasize to patient that goal is to prevent neurologic worsening, although most of a patient’s neurologic function improves following decompression
Contraindications
Predominantly dorsal compression of neural elements
Isolated trauma to posterior elements that is not amenable to anterior approach
Relative contraindications: soft-tissue destruction or anomalies of the anterior cervical spine (eg, post radiation)
Preoperative Imaging
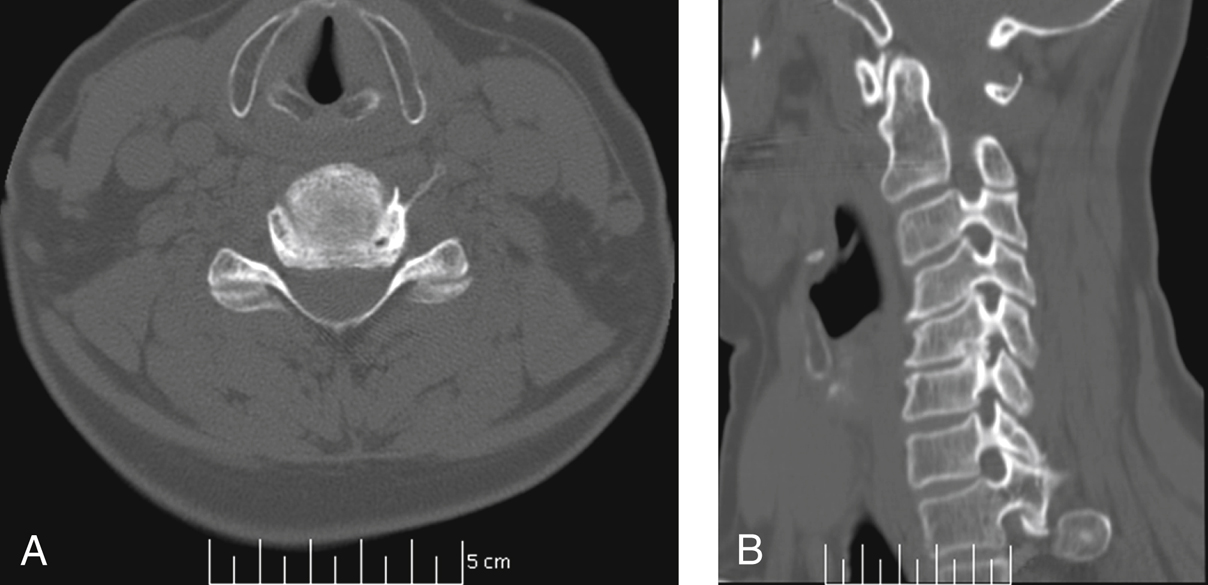
Figure 1CT scans used to evaluate a patient before anterior cervical diskectomy and fusion. A, An axial cut through the C5-6 interspace demonstrates foraminal stenosis on the left side from osteophyte formation. B, An oblique CT reconstruction demonstrates the specific areas of bony overgrowth into the left C5-6 foramen.
Plain radiography—AP and lateral; oblique views evaluate narrowing of neuroforamina; flexion-extension views evaluate instability and/or rigidity of sagittal plane deformity
MRI—Most sensitive for assessing the morphology of the neural elements and compression of spinal cord and/or nerve roots; less effective at detecting foraminal stenosis and demonstrating cortical margins
CT—Best for evaluating bony morphology (Figure 1)
Myelography—Useful when patient has existing hardware; demonstrates filling defects as a means of assessing neural compression, although cause of contrast blockade cannot be shown
Procedure
Room Setup/Patient Positioning
Supine position on standard table
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


