Anterior Approach for Open Reduction of the Developmentally Dislocated Hip
Richard M. Schwend
DEFINITION
Developmental dysplasia or dislocation of the hip (DDH) is a disorder that may affect the development and stability of the hip joint during the critical period of growth, either in utero or after birth.
This may lead to dysplasia, subluxation, or frank dislocation of the hip joint.
ANATOMY
Growth of the hip joint is genetically and mechanically determined.
In the first trimester, the structures of the joint begin as a single mass of scleroblastema with a globular femoral head that becomes cartilage at 6 weeks.
By 8 weeks’ gestation, the start of the fetal period, vascular invasion leads to endochondral ossification.
The joint space develops by degeneration at 7 to 8 weeks, and the structure of the joint is well apparent by week 11.
A round and reduced femoral head influences the concave shape of the acetabulum to develop.
Acetabular growth depends on interstitial, appositional, periosteal new bone and secondary centers of ossification growth.
In the first two trimesters of fetal life, the acetabulum is a hemisphere with a depth 50% of its diameter. However, by the time of birth, the depth is only 40% of its diameter, which may contribute to instability at birth.
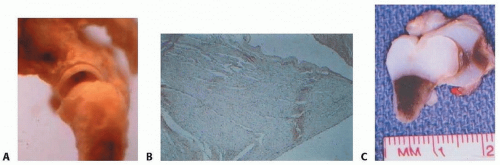
The acetabular labrum, which resembles an O ring (FIG 1A), contributes considerable mechanical stability and proprioceptive feedback (FIG 1B).
By 8 years of age, the acetabular shape is for the most part determined and thus surgical reduction is less advised, especially if the dislocation is bilateral.
There is continued growth into adolescence, with the triradiate cartilage fusing by 13 years in girls and 15 years in boys.
Closure of the triradiate cartilage may occur earlier in the dysplastic hip.
By adulthood, the acetabular depth is 60% of its diameter.
The proximal femur is formed initially as a single chondroepiphysis (FIG 1C), with the ossific nucleus typically appearing in infancy at 2 to 8 months of age.
There may be some side-to-side size discrepancy in appearance.
The greater trochanter nucleus appears at about 3 years in girls and 5 years in boys, with the lesser trochanter appearing by age 6 to 11 years.
The femoral head vascularity is mostly from the medial and somewhat from the lateral femoral circumflex arteries. Because it is an intra-articular dome-shaped structure, this blood supply is susceptible to injury.
PATHOGENESIS
Around the time of birth, capsular laxity, a normally shallow acetabulum, and abnormal mechanical forces, such as those seen in breech presentation, may cause the hip capsule to be lax and to dislocate.
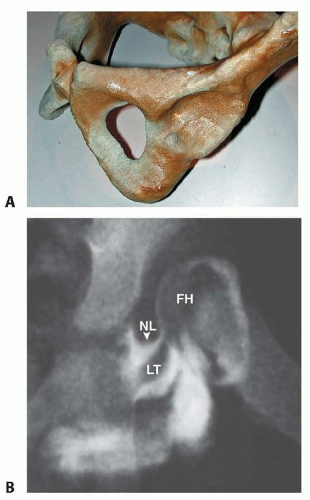
An absent or subluxated femoral head eventually leads to a flat, egg-shaped acetabulum, which is a consistent finding on three-dimensional computer modeling performed of the acetabulum (FIG 2A).
With time, the neolimbus, which is abnormally formed articular cartilage, can develop at the edge of the acetabulum. It can be a barrier to reduction (FIG 2B).8
A steep, maloriented growth plate; intra-articular obstructions; and stunting of periosteal new bone formation all in time contribute to further deformity.
Mechanical blocks to reduction include the anteromedial capsule, ligamentum teres, psoas tendon, neolimbus, transverse acetabular ligament (which is an inferior medial extension of the acetabular labrum), and intra-articular pulvinar tissue.
An inverted labrum is rarely a block to reduction.
The average unit load of human and animal joint cartilage is 25 kg/cm2.
Hips with acetabular dysplasia, and particularly with subluxation, have about 25% less contact area and more unit load (stress) per area of contact.
There is an inverse relationship between greater contact pressures and the onset of osteoarthritis.
NATURAL HISTORY
Newborn period
About 1 in 60 infants have instability at birth, with 60% of cases resolving in the first week of life and 88% by the first 2 months. Thus, about 1.5 in 1000 have a true dislocation.2
Muscle activity is considered important for recovery and is the basis of the Pavlik harness success.
Untreated acetabular dysplasia with subluxation or dislocation
The natural history of hip dysplasia when subluxation or dislocation is present is predictable. The long-term outcome is worse than with acetabular dysplasia without subluxation.13
The onset of symptoms and radiographic deterioration is directly related to the degree of subluxation and dysplasia.
Clinical symptoms, typically pain, may antecede the radiographic deterioration by 10 years.
If the hip is completely dislocated, limb length discrepancy and back and knee pain are common, whereas painful arthritis correlates with the presence of a false acetabulum and its adverse effect on the femoral head articular cartilage.
Acetabular dysplasia with no subluxation
The natural history of acetabular dysplasia is much less predictable when subluxation or dislocation is absent.13
During childhood, hips that are well centered improve their acetabular dysplasia, although not always to normal, whereas the hip that is radiologically eccentric typically does not improve.
If the center-edge angle in the mature hip is less than 20 degrees, the hip will likely develop arthritis sometime during the patient’s lifetime. However, it is difficult to determine how early in life the deterioration will occur.
Although hips with acetabular dysplasia can spontaneously improve, this improvement is not predictable or necessarily complete.10
A hip with a persistently upsloping lateral margin seen on an anteroposterior (AP) radiograph generally develops arthritis by late adulthood.11
PATIENT HISTORY AND PHYSICAL FINDINGS
Because 75% of DDH occurs in female infants with no other risk factures, clinical examination of all infants is the most important method of detecting hip dysplasia.
All newborn infants should receive a gentle and focused examination of the hips, including range of motion and Ortolani maneuver.
The physical examination of the newborn, rather than imaging studies, should determine the diagnosis of DDH and the need for treatment.
An Ortolani-positive hip is dislocated or subluxated and the examiner perceives that the hip partially reduces with abduction. After several months of age, the hip may appear stable on examination but may still be dislocated due to tightening of the soft tissue structures about the hip.
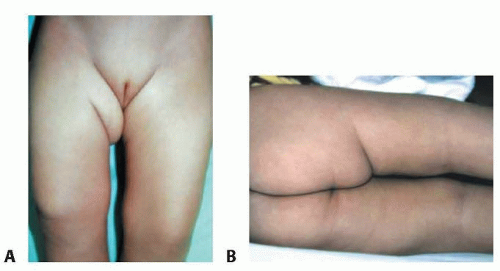
The child is examined for any abnormal skin creases (FIG 3). Proximal skin creases may indicate a dislocated hip or a short femur. The examiner should also note the
level of the popliteal skin crease, the position of the knee, and any lateral displacement of the hip.
A simple, high-pitched and commonly felt “hip click” is not a sign of instability or dislocation.
Hip instability decreases with time, whereas deformity, such as limited hip abduction, increases with time.
The young infant with a dislocated hip may have normal abduction until several months of age. There may be limited abduction in developmental coxa vara. Abduction may appear to be normal if both hips are dislocated.
The upper extremities, spine, and feet are always inspected to evaluate for possible generalized conditions such as arthrogryposis or neuromuscular conditions.
In the child of walking age, a delay of walking may be the first indicator that the hip is dislocated.
Dipping of the pelvis and shoulder (Trendelenburg gait), female profile (pelvic widening from the dislocation), and shortening of the thigh (Galeazzi sign) are classic signs of a dislocated hip in the older child.
The Galeazzi test may also be abnormal if the child has a congenital short femur.
Additional signs of Trendelenburg gait include side-to-side waddling, indicating weak hip abductors, or the examiner may see lurching, indicating weak hip extensors. The child may stand or walk with hyperlordosis. These are proximal compensations for a hip dislocation and the resulting inadequate muscle strength to support the pelvis.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Ultrasound is a useful imaging method up to 6 months of age (FIG 4A).
The two most common indications for ultrasound imaging are for screening the asymptomatic infant considered to be at high risk for hip dislocation (girls born breech have a 133/1000 risk of DDH) and for following an infant with proven DDH, especially during Pavlik harness treatment.
The AP radiograph is most useful in infants older than 6 months of age.
In children older than 3 years of age, the Shenton line is a reliable indicator of subluxation (FIG 4B).
The Von Rosen view in abduction and internal rotation shows the ability of the femoral head to reduce.
In the adolescent or adult hip, a standing AP pelvis view is obtained with measurement of the center-edge angle, as well as standing false-profile views of each hip joint (FIG 4C-E).
The normal center-edge angle on the AP pelvic radiograph is greater than 24 degrees.
Decision analysis model indicates that the most effective way to prevent hip arthritis by age 60 years is to do physical examination screening on the hips of all infants and to use ultrasound selectively on those infants with high risk factors.5
Intraoperative arthrography can show whether the femoral head is fully reducible with no medial pooling of contrast (FIG 4F).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree