(1)
Department of Orthopedic Surgery Academic Medical Centre, University of Amsterdam, Amsterdam, The Netherlands
Abstract
Ankle impingement syndromes are pain syndromes. Anterior ankle impingement is characterized by anterior ankle pain on activity. On investigation, there is recognizable tenderness on palpation at the anteromedial and/or anterolateral joint line. In case of radiological spurs or osteophytes, the diagnosis is anterior bony impingement. The anteromedial impingement view (AMI view) is recommended for detection of anteromedial osteophytes. Arthroscopic treatment with removal of osteophytes provides 83 % good/excellent result at 5–8 years follow-up (grade 0–I lesions). Arthroscopic removal of osteophytes secondary to arthritis (grade II lesions) gives good/excellent in 50 % of the cases.
Ankle impingement syndromes are pain syndromes. Anterior ankle impingement is characterized by anterior ankle pain on activity. On investigation, there is recognizable tenderness on palpation at the anteromedial and/or anterolateral joint line. The anteromedial impingement view (AMI view) is recommended for detection of anteromedial osteophytes.
Arthroscopic treatment with removal of osteophytes gives 83 % good/excellent result at 5–8 years follow-up (grade 0–I lesions).
The anterior joint capsule does not attach at the location where the osteophyte occurs.
The cause of the pain is compression of synovial tissue between the tibial osteophyte and the talar neck in the dorsiflexed position.
Osteophytes reduce the anterior space, thus making it easier for the synovial tissue to get compressed.
Removal of secondary osteophytes (osteoarthritic osteophytes) has a worse prognosis than removal of osteophytes without joint space narrowing. These osteophytes without joint space narrowing are not a manifestation of osteoarthrosis, and subsequently, a “normal” joint remains after removal of these spurs.
Distraction results in tightening of the anterior capsule which makes it more difficult to identify the osteophytes.
7.1 Introduction
Chronic anterior ankle pain is commonly caused by formation of talotibial osteophytes at the anterior part of the ankle joint. Morris (1943), McMurray (1950), and later Biedert (1991) named this condition “athlete’s” ankle or “footballer’s” ankle. In subsequent studies, this entity has been described to occur in other athletes, such as runners, ballet dancers, high jumpers, and volleyball players. Since then the term “footballer’s” ankle has been replaced by the anterior ankle impingement syndrome.
The pain from impingement lesions is caused by catching of the synovial tissue between part of the talus and part of the ankle mortise. Osteophytes or ossicles facilitate this process, since they limit the arc of motion.
A differentiation has been made between soft tissue impingement and bony impingement lesions (Biedert 1991; Cutsuries et al. 1994; Ferkel and Fasulo 1994).
In general, osteophytes are the secondary manifestation of osteoarthritic changes (Hermodsson 1983; Van Dijk et al. 1995). However, repetitive minor trauma in the ankle, as seen in athletes, can induce spur formation (McMurray 1950).
In a patient with anterior ankle impingement, recognizable tenderness on palpation is the most important clinical finding. When standard X-rays cannot disclose the cause of an anterior impingement, special X-rays have been developed to disclose medially located bony spurs (Tol et al. 2004). When conservative treatment fails, operative treatment consists of removal of bony and/or soft tissue impediments.
7.2 Etiology
McMurray attributed to the knowledge about the formation of the talotibial osteophytes. According to him, repeated capsular-ligamentar traction by repetitive kicking with the foot in full plantar flexion (i.e., traction spurs) (McMurray 1950) induces this osteophyte formation. Traction to the anterior ankle capsule, during plantar flexion movements, was supposed to be an important etiological factor (McMurray 1950; Biedert 1991; Cutsuries et al. 1994; Ferkel and Scranton 1993; Ogilvie-Harris et al. 1993). This hypothesis is supported by the fact that these spurs are frequently found in athletes, who repetitively force their ankle in hyperplantarflexion actions, resulting in repetitive traction to the anterior joint capsule (Handoll et al. 2001). It assumes however that the capsular attachment is located at the anterior cartilage rim at the location where spurs originate.
A recent study demonstrated that the anterior joint capsule does not attach at the location where the osteophyte occurs. The anterior joint capsule attaches onto the tibia on an average of 6 mm proximal to the joint level (Tol and Van Dijk 2004) (Figs. 7.1 and 7.2). On the talar side the capsule attaches likewise approximately 3 mm from the distal cartilage border. The distance of capsule attachment to the location where the bony spurs are most frequently localized is thus relatively large. Based on these anatomic observations, the hypothesis of formation of talotibial spurs due to recurrent traction to the joint capsule (traction spurs) is not very plausible. This is supported by observations during arthroscopic surgery (Tol and Van Dijk 2004). In patients with bony impingement, the location of tibial spurs is reported to be at the joint level and always within the confines of the joint capsule (Tol and Van Dijk 2004; Tol et al. 2001). On the talar side, the typical osteophytes are found proximal to the talar neck notch. Tibial and talar osteophytes can easily be detected during an arthroscopic procedure with the ankle in forced dorsiflexion. The capsule does not need to be detached to locate these osteophytes.
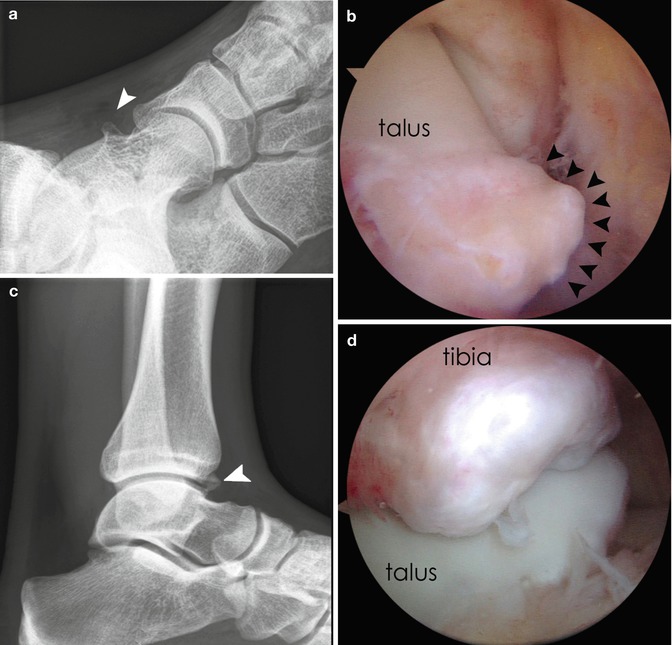
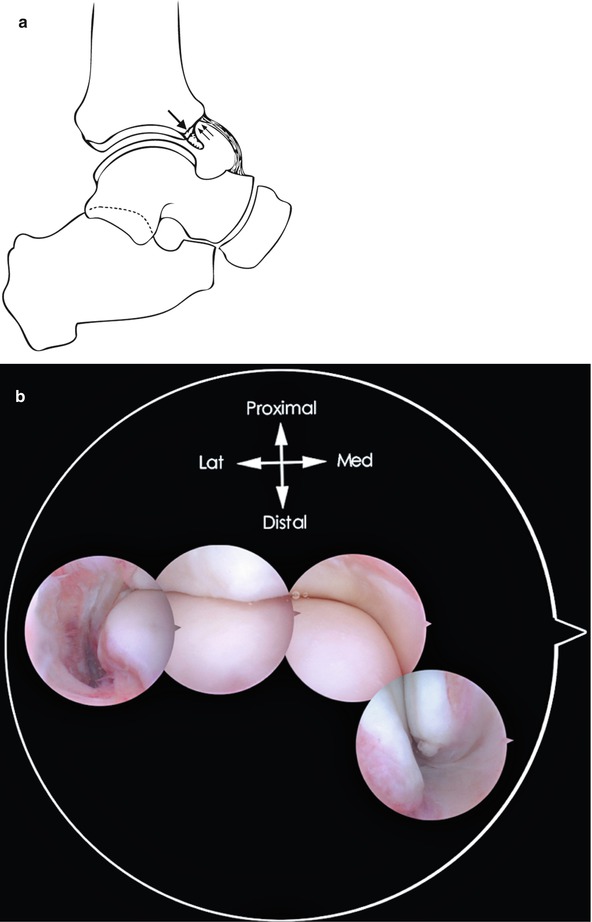
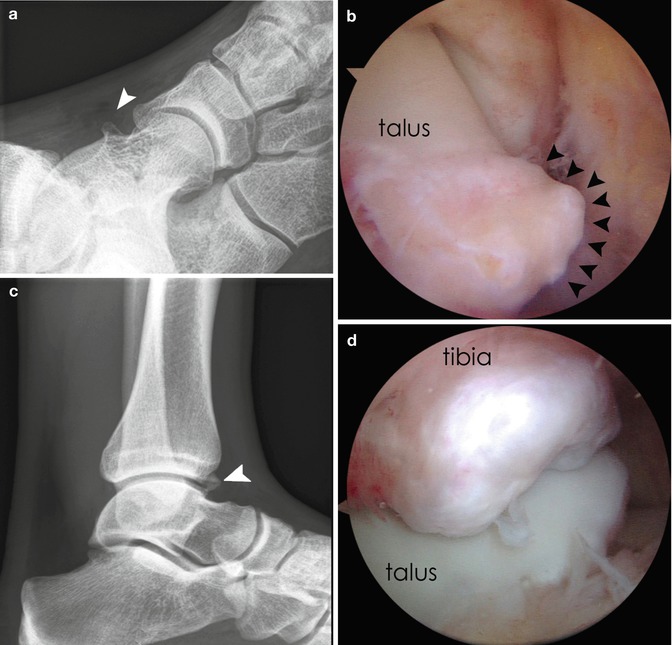
Fig. 7.1
Recent studies have demonstrated that the anterior joint capsule does not attach at the location where the osteophyte occurs. The anterior joint capsule attaches onto the tibia on average of 6 mm proximal to the joint level. The same is true for most of the talar osteophytes. (a) Anteromedial impingement view demonstrating the talar osteophyte (arrowhead). (b) Arthroscopic view with scope in the anterolateral portal. The anteromedial osteophyte is clearly visible (arrowheads). Behind the osteophyte we see the medial malleolus. (c) Lateral X-ray showing an osteophyte on the distal tibia (arrowhead). (d) Arthroscopic view with the scope in the anterolateral portal showing the osteophyte on the distal tibia. Below the osteophyte the talar cartilage is visible
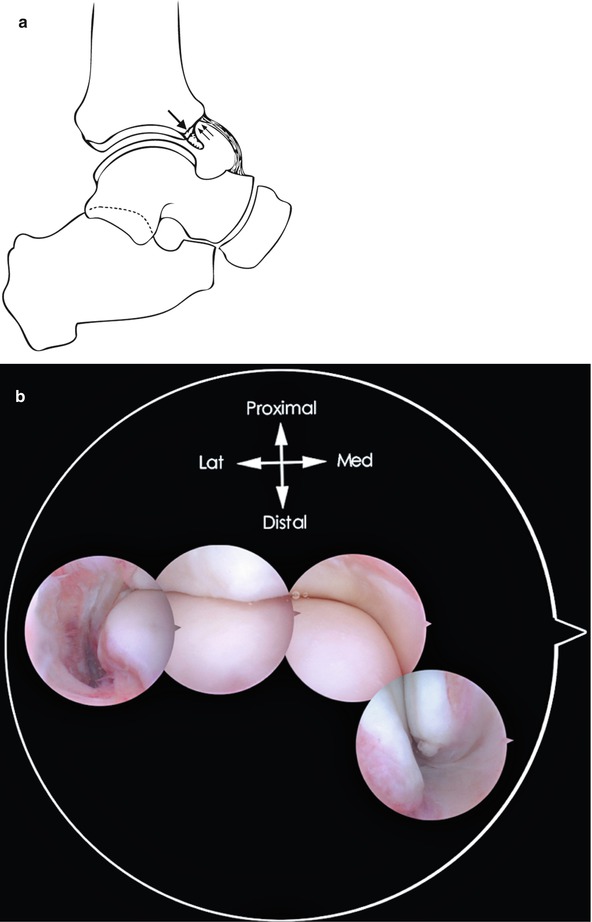
Fig. 7.2
(a) Schematic drawing to show the attachment of the anterior joint capsule and the location of the osteophyte on the distal tibia. (b) Composition picture of arthroscopic view, showing the anterior aspect of the medial malleolus and the distal tibia which is covered with hyaline cartilage. It is this anteriorly located cartilage that undergoes the transformation to osteophyte. The anterior joint capsule attaches more proximal. On the tips of the medial malleolus, a small ossicle is visible
O’Donoghue (1957) considered the osteophytes to be related to direct mechanical trauma associated with the impingement of the anterior articular border of the tibia and the talar neck, during forced dorsiflexion of the ankle joint. Here, bone formation is considered to be a response of the skeletal system to intermittent stress and injury, as evidenced by Wolff’s law of bone remodeling (Williams and Brandt 1984). According to Hawkins (1988), runners, dancers, and high jumpers are prime examples of athletes who are predisposed to sports-related repeated trauma. Even though this etiological factor is widely cited (Cutsuries et al. 1994; Ferkel and Fasulo 1994; Ogilvie-Harris et al. 1993; Hawkins 1988), experimental evidence-based support is scarce.
Along the distal tibia, the width of the non-weight-bearing cartilage rim extends up to 3 mm proximal to the joint line (Fig. 7.3). It is this non-weight-bearing anterior cartilage rim that undergoes the osteophytic transformation (Ferkel and Fasulo 1994; Tol and Van Dijk 2004). It has been postulated that chondral and bone cell stimuli initiate a repair reaction with cartilage proliferation, scar tissue formation, and calcification (Fig. 7.4). Additional damage by ankle sprains—recurrent instability—or forced dorsiflexion movements will further enhance this process (Biedert 1991). Recent studies have demonstrated that chronic ankle instability is indeed correlated with osteophytic formation in the medial ankle compartment (Van Dijk et al. 1996; Krips et al. 2000). After an ankle fracture, spur formation is a regular finding (Stufkens et al. 2009). Another etiological factor in the development of spurs is recurrent microtrauma. In soccer players it was demonstrated that spur formation is related to recurrent ball impact, which can be regarded as repetitive microtrauma to the anteromedial aspect of the ankle (Tol et al. 2002). Repetitive trauma to the anteromedial cartilage can probably be precluded by prevention of recurrent ankle sprains.
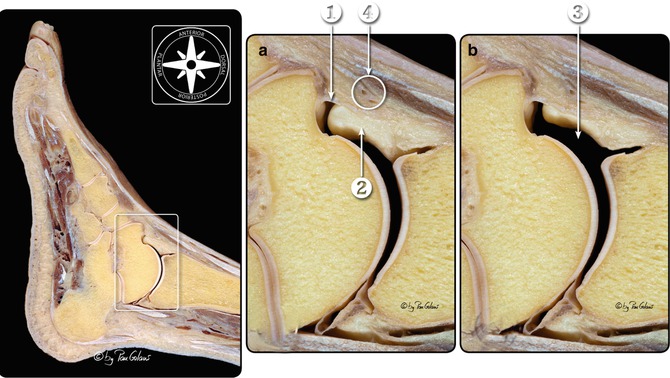
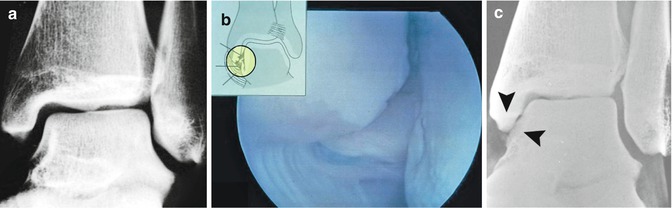
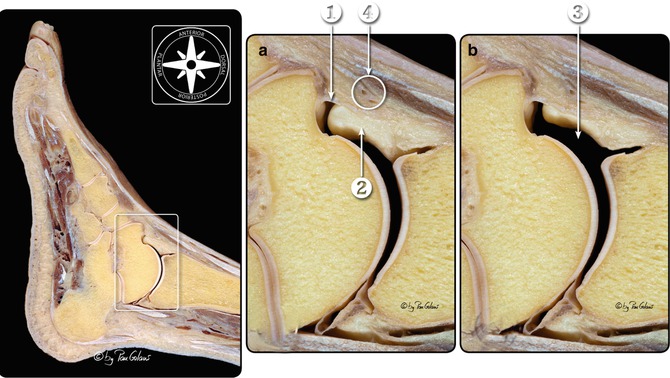
Fig. 7.3
Sagittal section of the foot and ankle. (a) The insertion of the anterior joint capsule is shown on the talar neck and the distal tibia. The space between the joint capsule and the joint is filled with fat tissue which is attached to the joint capsule. This fat mass is comparable to corpus Hoffa. The hyaline cartilage in the distal tibia is clearly extending to the anterior surface of the distal tibia. (b) Situation after filling the anterior joint space with saline (modified by image editing software). The anterior capsule moves away from the joint through the pressure of the fluid. The layer of fatty tissue is extended and compressed against the joint capsule. This creates an anterior “working area.” Note that the anterior part of the distal tibia is covered with hyaline cartilage. 1. Capsule joint. 2. Anterior “working area.” 3. Fat pad tissue (intracapsular but extrasynovial). 4. Anterior neuromuscular bundle (With kind permission of © Pau Golanó 2013)
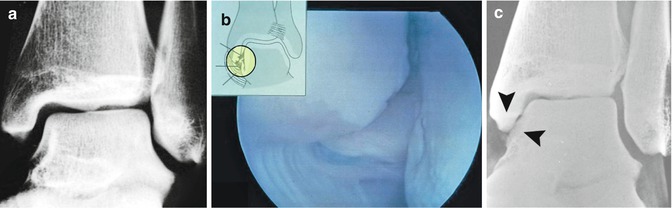
Fig. 7.4
(a) 4 days after supination trauma of the left ankle. The trauma resulted in a rupture of the ATFL and CFL. X-ray shows no abnormality. Surgery was performed with suturing of the ruptured lateral ligaments. (b) Arthroscopic view of the tip of the medial malleolus and medial talar facet 5 days after supination trauma. Damage to the tip of the medial malleolus and medial talar facet is seen and is the result of a “kissing lesion” with compression during the supination trauma between medial malleolus and medial talar facet. The inset shows the outside view. (c) 7 years after trauma, showing calcification and osteophyte formation on the medial talar facet and tip of the medial malleolus (see arrowheads)
In the anterior ankle impingement syndrome, the cause of pain is hypothesized to be not the osteophyte itself but the inflamed soft tissue that is caught between the osteophytes (Tol et al. 2001) (Figs. 7.5 and 7.6). The tibial and talar spurs typically do not overlap each other (Berberian et al. 2001). Histopathological analysis of arthroscopic resected soft tissue reveals synovial changes and chronic inflammation (Ferkel et al. 1991). In cadaver specimens, a triangular soft tissue synovial fold, subsynovial fat and collagen tissue, was found along the entire anterior tibiotalar joint line (Fig. 7.3). This soft tissue component gets squeezed between the anterior distal tibia and the talus during forced dorsiflexion movements. Recurrent trauma to this soft tissue may lead to hypertrophy of the synovial layer, subsynovial fibrotic tissue formation, and infiltration of inflammatory cells. Talar and tibial osteophytes decline the anterior space, and compression of this soft tissue component is more likely to occur. It is therefore important to remove these osteophytes, restoring the anterior space and reducing the chance that symptoms recur.



Fig. 7.5
In the anterior ankle impingement syndrome, the cause of pain is hypothesized not to be the osteophyte itself but the inflamed soft tissue that is caught between the osteophytes. (a) Lateral X-ray in a patient with anterior ankle impingement syndrome demonstrating small osteophytes. (b, c) Arthroscopic view. Arthroscope in the anteromedial portal showing the osteophytic rim on the distal tibia. The synovitis is shown in the anterior recess (between 9 and 10 o’clock position). In dorsiflexion this richly vascularized and innervated synovial tissue can be squeezed between the osteophyte and the talar neck (not shown)

Fig. 7.6
(a–c) AP, lateral, and AMI view of patient with anteromedial impingement. The osteophytes on the anterior medial malleolus and medial talar neck are clearly seen on the AMI view (c). (d) Arthroscopic view of the anteromedial part of the joint. The scope is in the lateral portal. The synovitis is clearly seen blocking the view on the distal tibia and on the medial malleolus. The talar neck osteophyte is clearly visible
7.3 Clinical Presentation
The typical patient with an anterior ankle impingement is a relatively young athlete with a history of recurrent inversion sprains (Scranton and McDermott 1992). The patient presents with anterior ankle pain, swelling after activity, and (slightly) limited dorsiflexion (Cutsuries et al. 1994). Since anterior impingement is a clinical diagnosis, the diagnosis is based on findings during physical examination. Recognizable local tenderness on palpation is present on the anterior joint line, and osteophytes can be palpable with the ankle joint in slight plantar flexion.
A differentiation is made between anteromedial and anterolateral impingement (Fig. 7.7). On palpation of the anterior joint line, the patient is asked whether this recreates the pain. Since the middle section is covered by neurovascular structures and tendons, this part of the joint is difficult to access by palpation. If a patient with a clinical anterior impingement syndrome experiences pain predominantly located anteromedially when palpated, the diagnosis is anteromedial impingement. If tenderness on palpation is predominantly located anterolaterally, the diagnosis is anterolateral impingement. Forced hyperdorsiflexion can provoke the pain, but this test can be false negative.


Fig. 7.7
Anterior view of a right ankle indicating the three different anterior regions. The central part of the joint is located between the medial border of the anterior tibial tendon and the lateral border of the peroneus tertius tendon. Medial to the central part, at the level of the joint line, is the anteromedial region. Lateral to the central part, also at the level of the joint line, is the anterolateral region. The black lines depict the contour of the ankle joint. The redlines depict the underlying neurovascular bundle and extensor tendons
7.4 Additional Radiographs
Standard anteroposterior (AP) and lateral radiographs are used to detect the presence of osteophytes (Van Dijk et al. 1997a, b). In patients with anterior talar and/or tibial spurs, these spurs are regarded to be the cause of the anterior impingement syndrome. Due to their location, they lead to a “kissing” phenomena and concomitant pinching of hypertrophic synovial tissue (Fig. 7.6). Because of the anteromedial notch (Tol and Van Dijk 2004), anteromedial osteophytes are undetected by standard radiographs in the majority of patients with anterior impingement complaints (Tol et al. 2002). In a cadaver study, it was shown that anteromedial tibial osteophytes up to 7.3 mm in size, originating from the anteromedial border, remain undetected due to superposition or overprojection of the more prominent anterolateral border of the distal tibia (Tol et al. 2002). Medially located talar osteophytes remain undetected due to overprojection of superposition of the lateral part of the talar neck and body (Tol et al. 2002) (Fig. 7.8).


Fig. 7.8
A 43-year-old patient presenting with anteromedial left ankle pain during running. (a) Anteromedial impingement (AMI) view showing an osteophyte at the medial border of the distal tibia (arrowhead). (b) In this standard lateral radiograph, the medially located osteophyte on the anterior distal tibia remains undetected
Detection of these osteophytes is important for preoperative planning. Several authors have stated that surgical distinction between normal bony and soft tissue variants and pathologic conditions is difficult, because of subtle variations in joint anatomy (Ferkel 1996; Ray et al. 1994; Vogler et al. 1994). Especially in patients with accompanying synovial reflections, overlying the concealed osteophytes (Ray et al. 1994), anteromedial bony spurs are poorly visualized arthroscopically and can therefore be missed easily. Radiographic classification of spur formation correlates with the surgical outcome (Ferkel and Fasulo 1994; Van Dijk et al. 1997a, b; Scranton and McDermott 1992). An oblique radiograph was introduced to detect medially located tibial and talar osteophytes. In this oblique anteromedial impingement (AMI) view, the beam is tilted a 45-degree craniocaudal direction with the leg in 30-degree external rotation and the foot in plantar flexion in relation to the standard lateral radiograph position.
The sensitivity of lateral radiographs for detecting anterior tibial and talar osteophytes is 40 and 32 %, respectively (specificity 70 and 82 %) (Tol et al. 2004). When the lateral radiograph is combined with an oblique AMI radiograph, the sensitivity increases to 85 % for tibial and 73 % for talar osteophytes. This increase is due to the high sensitivity of the oblique AMI radiographs for detecting anteromedial osteophytes (93 % for tibial and 67 % for talar osteophytes). A lateral radiograph is insufficient to detect all anteriorly located osteophytes, and an oblique AMI radiograph is a useful adjunct to routine radiographs and recommended to detect anteromedial tibial and talar osteophytes (Figs. 2.8 and 7.8).
7.5 Preoperative Considerations
1.
The cause of the pain is compression of synovial tissue between the anterior margin of the tibia or fibula and the talar neck in the dorsiflexed position (Fig. 7.9).


Fig. 7.9
Arthroscopic view of anterior compartment of the ankle. Synovitis as cause of anterior impingement
2.
Osteophytes reduce the anterior space, thus making it easier for the synovial tissue to get compressed.
3.
The rationale for removing osteophytes in a patient with anterior ankle impingement is to restore the anterior space, thereby reducing the chance that the synovial tissue gets squeezed again and that symptoms recur.
4.
Removal of secondary osteophytes (osteoarthritic osteophytes) has a worse prognosis than removal of osteophytes without joint space narrowing. These primary osteophytes are not a manifestation of osteoarthrosis, and subsequently, a “normal” joint remains after removal of these spurs.
5.
Over 90 % of osteophytes are situated well within the attachment of the joint capsule. On the talar site, the typical osteophyte is found proximal to the talar neck notch. Both tibial and talar osteophytes can easily be detected during an arthroscopic procedure with the ankle in forced dorsiflexion. The capsule does not have to be detached to locate and remove these osteophytes.
6.
7.
In the forced dorsiflexion position, the talus is concealed in the joint which protects the weight-bearing cartilage of the talus from potential iatrogenic damage.
8.
Osteophytes are covered by scar tissue and synovial folds. They can easily be missed during arthroscopy. Preoperative planning with correct visualization of the location and size of the osteophytes is of vital importance. Remember that when the X-ray shows no spurs, during arthroscopy, you are not prepared to take away any bone.
9.
In anterolateral impingements, the arthroscope remains introduced through the anteromedial portal, while the anterolateral portal is the working portal. In anteromedial impingement, the arthroscope is introduced through the anterolateral portal, while the anteromedial portal now is your working portal.
10.
To determine the size of the osteophytes during an arthroscopy, the surgeon has to identify the normal contour of the distal tibia proximal to the osteophyte. To achieve this, you need to shave away the tissue just superior to the osteophyte.
11.
In case of medial malleolar osteophytes, an overcorrection of the tip of medial malleolus is generally pursued by shaving some of it away after resection of the osteophyte.
7.6 Preoperative Planning
The size of spurs is measured on the lateral radiograph. In this projection both malleoli are positioned perpendicular to the surface of the film, and therefore the foot has to be placed in a sagittal angle that can be well over 45°. In this projection, it is the anterolateral part of the distal tibia that is visualized. If an osteophyte is present, it is located anterolateral. The most obscure part of the anterior distal tibial rim is the medial part where the anteromedial tibia border and the anterior rim of the medial malleolus connect. Medial osteophytes of up to 7 mm are undetected on the lateral X-ray. These anteromedially located osteophytes can be detected by means of the so-called AMI view. In this oblique anteromedial impingement (AMI) view, the beam is tilted in a 45-degree craniocaudal direction with the leg in 30° of external rotation and the foot in plantar flexion. The sensitivity of lateral radiographs for detecting anterior tibial and talar osteophytes was 40 and 32 %, respectively (specificity 70 and 82 %) (Ray et al. 1994). When the lateral radiograph was combined with an oblique AMI radiograph, the sensitivity increased to 85 and 73 %, respectively. This increase was due to the high sensitivity of the oblique AMI radiographs for detecting anteromedial osteophytes (93 % for tibial and 67 % for talar osteophytes). A lateral radiograph is only sufficient to detect anterolateral osteophytes. An oblique AMI radiograph is a useful adjunct to routine radiographs and recommended to detect anteromedial tibial and talar osteophytes (Tol et al. 2004).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








