Answers
Case 1 answers
1. The critical feature is the asymmetrical visible swelling below the joint. A ‘swollen knee’ and limp could indicate one of several common inflammatory or traumatic diagnoses. The earlier football injury is a ‘red herring’, which should not mislead, because parents often ascribe the onset of tumour symptoms to a knock sustained in sport.
2. The X-ray shows a sclerotic tibial lesion with calcification extending into the soft tissues. This lesion arises from the tibial metaphysis and on biopsy is an osteosarcoma.
3. Treatment for osteosarcoma was revolutionized by the advent of effective chemotherapy in the 1980s. Many children and adolescents will receive ‘neoadjuvant’ chemotherapy, often including methotrexate. Neoadjuvant treatment involves chemotherapy both before and after definitive surgery. Increasingly ‘limb salvage’ surgery will allow an affected limb to be saved, although amputation is still performed in about 20% of patients.
Case 2 answers
1. The X-rays show a Charnley hip replacement. A trans-trochanteric approach to the hip was made at the original surgery and wires inserted to reattach the greater trochanter to the femur. There is wear of the high-density polyethylene cup as the prosthetic femoral head should lie in the centre of the cup, but it has migrated proximally. The joint is becoming unstable as a result of the wear.
2. Exclude infection and check his erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) level and white count. An aspiration arthrogram will also help to exclude infection within the hip joint and can also demarcate prosthetic loosening.
3. Revision of the hip replacement is indicated if his symptoms are troublesome and if he is fit for surgery.
Case 3 answers
1. The postero-anterior X-ray shows an adolescent idiopathic scoliosis. Note that the film has been taken as the patient stands and is shown with her heart on the left so that one is looking at the spinal deviation from behind. The direction to which the convexity of the curve points indicates the side of the curve; right thoracic and left lumbar curves are a common combination.
2. The child should be examined from behind to observe her shoulders for asymmetry of height, scapular protrusion that may suggest an underlying rib hump, and the pelvis for symmetry of height of the iliac crests. A forward bending test is then performed because the rotational component of the scoliosis increases with spinal flexion. A ‘postural’ curve will disappear, whereas a significant ‘structural’ curve, such as occurs in adolescent idiopathic scoliosis, will highlight rib cage elevation, deformity and asymmetry. The child should be assessed neurologically and this should be normal in adolescent idiopathic scoliosis. Curve magnitude and location of the apical vertebra are obtained from X-rays using Cobb’s angle (see text on spinal deformity, Chapter 26). In general, for angles of less than 20° curves are kept under observation, bracing is used for those between 20° and 45°, and surgery for curves greater than 45°. MRI of the thoraco-lumbar spine is an essential preoperative requisite to exclude any co-existing spinal skeletal or neurological anomaly.
Case 4 answers
1. This is Perthes’ disease – perhaps better termed a ‘condition’ – which represents an avascular necrosis of the capital (upper femoral) epiphysis; the X-ray shows collapse of the capital epiphysis.
2. The prognosis will depend on the extent of involvement of the femoral head, the child’s age at presentation and the sex of the child. The younger the child is at presentation, the better the outlook, and boys have a better prognosis than girls. A 7-year-old boy presenting for the first time with whole head involvement would be expected to have a better outcome in terms of sphericity of the femoral head at maturity than a 9-year-old girl presenting for the first time with a similar extent of necrosis.
Case 5 answers
1. This is a slipped upper (capital) femoral epiphysis (see X-ray). This usually affects children between the ages of 10 and 15 years. It may be classified according to the time that the patient had their symptoms (acute, chronic, acute on chronic), the severity of the slip (mild, moderate and severe) or whether the patient could bear weight on the affected leg with or without walking aids or not (stable or unstable).
2. He should be admitted to hospital, placed on bed-rest and have the slip stabilized on the next convenient operating list.
3. The likelihood of developing a slip in the contralateral hip is about 30%, and the boy and his parents should be made aware of this. There is some controversy as to whether or not the opposite side should be stabilized prophylactically at the time of fixation of the symptomatic side. This will depend on the surgeon’s, patient’s and family’s views.
Case 6 answers
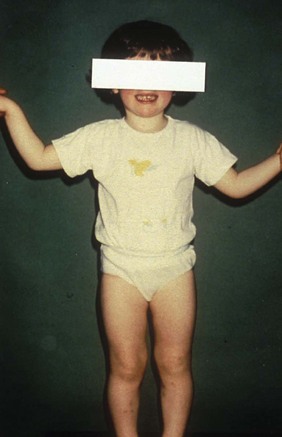
1. Assess limb alignment with the child standing. Check limb length and the child’s torsional profile (see Chapter 1 on Physical examination) because external femoral torsion and internal tibial torsion can exacerbate the appearances of bow legs.
2. The toddler has physiological bow legs (genu varum).
3. This is a physiological condition often seen in toddlers and normally resolves by about the age of 2 years. It is important to ensure that the deformity is symmetrical because unilateral bowing may be an indication of a structural abnormality in the lower limb, which would require further investigations.
4. Take the parents’ concerns seriously and allow time to discuss the condition with them. If the lower limbs are symmetrical in alignment and length, it is highly likely that the appearances are physiological and there is no underlying structural reason for the appearances. Thus further imaging is not required and the parents can be reassured that the appearances can be expected to improve over the next 12 months or so (see figure). No treatment is required; special shoe wear and exercises are of no proven benefit.
Case 7 answers
1. The differential should include habitual toe walking, congenitally short gastrocnemii and diplegic cerebral palsy.
2. In broad terms the motor cortex, cerebellum and basal ganglia. A lesion of the motor cortex will produce spasticity, a lesion of the cerebellum results in ataxia and that of the basal ganglia will produce dyskinesia.
3. This boy has diplegic cerebral palsy because he was born prematurely, had a delay in walking, walks on tiptoes, and has increased tone and brisk reflexes in the lower limbs. If he were a habitual toe-walker he would have normal muscle tone and calf muscle length, and if he had congenitally short gastrocnemii he would have normal tone but a restriction in ankle dorsiflexion.
Case 8 answers
1. Duchenne muscular dystrophy (DMD). This is the commonest inherited disease of muscle and is an X-linked recessive condition that can also arise spontaneously in about 15% of cases. Other conditions to consider are spinal muscle atrophy and other muscle dystrophies.
2. Plasma creatinine kinase concentration is often greatly increased in DMD. DNA analysis of peripheral blood can also show deletion of the dystrophin gene on the X chromosome.
3. The muscle weakness is progressive and many children lose the ability to walk between the ages of 8 and 12 years. As they become wheelchair-dependent they often develop contractures at the hips, knees and ankles and a neuromuscular scoliosis. Pulmonary function deteriorates in their second decade; this is often made worse by the scoliosis and patients have difficulty in clearing secretions. Patients usually succumb to respiratory failure or infection at around 20 years of age.
Case 9 answers
1. Calcaneovalgus. The foot is deviated away from the midline (valgus) and the heel is excessively dorsiflexed (calcaneus; the opposite is equinus).
2. The calcaneovalgus may be an example of a ‘packaging disorder’ where the foot has been moulded into its shape by the pressure from the uterus. The foot will respond readily to passive stretching and there should be an excellent outcome. The foot posture may also result from a neurological disorder affecting the baby.
3. You must examine the baby’s hips for stability and their spine. The photograph shows the baby’s back and there is a meningocele. This is an example of spina bifida, which produces a lower motor neurone lesion. The tibialis anterior (L4) is working and is dorsiflexing the ankle. The excessive dorsiflexion (calcaneus) has arisen because the posterior calf muscles (L5, S1, 2) are paralysed and there is an unopposed action of tibialis anterior.
Case 10 answers
1. This is clubfoot or talipes equinovarus. Equinus indicates a plantarflexed position at the ankle, and varus a deviation towards the midline.
2. As a matter of routine you should examine the hips to exclude instability, and the spine to exclude spinal dysraphism as a cause of a neurological clubfoot. In the latter case there may be a hairy patch or sacral dimple overlying the lower spine.
3. The feet should be examined to assess their stiffness. A programme of passive stretching of the feet begins shortly after birth, and plaster casts are used to hold the position of the feet. In the past, about 50% of feet might have been operated on because of a deformity resistant to stretching, but recently a more conservative (Ponseti) approach has become more widespread.
4. There will be permanent thinning of the calf muscles on the affected side and a difference in shoe size because the foot on the affected side is usually smaller. If treatment is successful in producing a plantargrade and reasonably flexible foot, these features are not likely to affect function greatly.
Case 11 answers
1. The grandmother is right; although growing pains do not have any connection with growth itself, they do occur in young growing children. The cause is unknown, but the above history is typical. The peak incidence is between 4 and 8 years of age and is thought to be muscle fatigue in the thighs and calves.
2. Observe the child’s gait, examine their legs and spine carefully and include a neurological assessment. The diagnosis is made from the history and the absence of any objective abnormal physical findings. Remember referred pain, though. Obtain X-rays only if there is loss of movement at a joint or tenderness in a specific area. A bone scan might be indicated to exclude an osteoid osteoma, a benign bone-forming tumour that can produce bone pain, but this is likely to affect only one limb whereas ‘growing pains’ are usually symmetrical.
3. The condition resolves spontaneously, and the frequency and intensity of the pains abate. Inform the parents and child that the condition is self-limiting, but that the child should be reviewed if pains persist, particularly at night, and/or affect one limb only. Bone tumours are rare and musculoskeletal infection is not as common as it was, but worsening night pain affecting one limb or limb segment should be considered as a ‘red flag’ symptom. The laboratory results are all normal for a child of this age. Remember that the apparently raised alkaline phosphatase levels are actually a reflection of a healthy growing skeleton. Pregnancy is another physiological circumstance where the alkaline phosphatase is increased.
Case 12 answers
1. Examine her abdomen and spine; remember referred pain.
2. Irritable hip, septic arthritis of the hip, osteomyelitis of the proximal femur or pelvis, and Perthes’ condition.
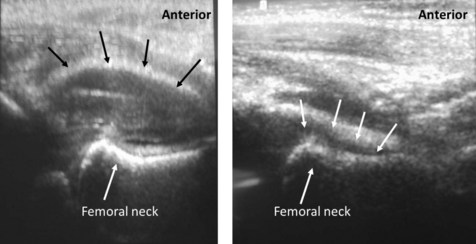
3. Check her temperature. X-ray the right hip and femur to exclude a fracture. If there is no fracture or hip pathology such as Perthes’ condition on the plain X-ray, obtain an ultrasound image of the hip. Take blood for estimation of CRP or ESR and white cell count to exclude infection. Obtain urine for culture. If the investigations show that she is afebrile, has a normal or only slightly raised CRP or ESR and white cell count, but that she has an effusion of the right hip demonstrated on ultrasound imaging, the diagnosis is an irritable hip. The illustration shows an ultrasound image of the affected hip on the left, with a normal hip ultrasound image for comparison on the right. The black arrows outline the distended hip capsule due to the effusion. It is not necessary to admit her to hospital because in most cases the pain settles over 48–72 hours and the child starts to walk again. Irritable hip may be associated with a recent viral infection or be an early sign of Perthes’ condition. The parents should be told that if the child becomes unwell or starts to develop a fever they should return to hospital promptly. This is to re-evaluate her, because missed septic arthritis of the hip can have a disastrous outcome.
Case 13 answers
1. True leg-length discrepancy is the difference in overall length when measured from the anterior–superior iliac spine to the medial malleoli when the legs are placed symmetrically. Apparent leg-length discrepancy is the difference in leg length when measured from the xiphisternum or umbilicus to the medial malleoli.
2. The discrepancy can also be assessed clinically by placing blocks under the short leg and assessing when the pelvis is level. Radiological imaging is obtained from a CT scanogram of the lower limbs. The image can be digitized to give lengths of the thigh and shin segments. An X-ray of the left wrist is taken to assess the child’s bone age, which may be different from their chronological age.
3. A discrepancy predicted to be 3.5 cm at skeletal maturity is best managed by an epiphyseodesis (surgical destruction of a growth plate) of the long leg. This may involve the distal femoral or proximal tibial growth plates, or both, depending on the discrepancy and the amount of residual skeletal growth left. The distal femoral plate grows at about 3/8″ (1 cm) and the proximal tibial plate at 2/8″ (0.7 cm) per year. Girls stop growing at about 14 years and boys at about 16 years of age. Knowledge of the child’s bone age helps to predict when skeletal maturity will occur and one can then calculate when the growth arrest at a physis should be made.
Case 14 answers
1. Access for skin hygiene can be hampered by the flexed position of the fingers, thumb and wrist, and the skin can become macerated in the wrist and palm creases. The posture of the hand is not functional for putting on and removing clothing, and the hand cannot rest on a flat surface. The patient may also feel self-conscious about the posture of his hand.
2. If there is excessive muscle tone from the upper motor neurone lesion, but adequate muscle length, an injection of botulinum toxin into the wrist and finger flexors may help. Botulinum toxin inhibits the action of acetylcholine at the neuromuscular junction. The pharmacological effect wears off after about 3 months. If there is shortening of the flexors and a fixed contracture of the wrist, surgical lengthening of the flexors and a wrist fusion are likely to improve posture, hygiene and cosmesis, but not necessarily hand function. Hand orthoses are poorly tolerated. The clinical photograph shows the postoperative appearance of the hand and wrist.
Case 15 answers
1. A painful red bunion occurs when the forefoot is chronically forced into shoes too tight for the forefoot. There is usually evidence of ‘hallux valgus’ deformity on X-ray. Hallux valgus is a common condition that is most evident in people with evidence of joint or soft-tissue laxity. This is not pathological, and may affect up to 10% of the population, women more than men. The intermetatarsal ligaments stretch and the forefoot splays outwards on standing. This makes the condition painful on compressing the forefoot within tight fashion shoes, but is often not painless when barefoot or in trainers.
2. If correctible passively, there is a good chance of improvement with footwear advice. Sometimes a moulded instep orthosis can also help by allowing the forefoot to take its original shape within the shoe. If pain persists, excision of the bunion with an osteotomy to correct the underlying ‘metatarsus primus varus’ (first metatarsal in varus) is performed in younger people. Older patients with low demand may have an excision arthroplasty with excision of the base of the proximal phalanx (Keller’s procedure). Osteoarthritis of the first metatarsophalangeal joint may also respond to this operation, or to an arthrodesis.
Case 16 answers
1. Cardinal radiographic features of osteoarthritis are:
2. Non-surgical treatments include analgesia and use of a stick. For most patients, the stick should be held in the opposite hand to off-load the painful hip when weight-bearing on the painful side. Very occasionally a patient with a waddling-type gait may find relief by holding the stick in the hand on the affected side hard against the affected leg during stance.
3. In many patients without a significant inflammatory component, and in whom there is no joint collapse, pain may not be a major complaint. Instead it may be possible to identify a gradual deterioration in walking distance and a gradual reduction in work-related and recreational activities. Inability to tie or put on shoes reflects stiffness of the hip joint. Capsular contracture is part of the pathology of osteoarthritis.
Case 17 answers
1. Waddell’s inappropriate back pain signs include, as well as the positive ‘long sit’, pain in the low back on applying pressure to the top of the head (crown pressure sign), pain in the low back when the patient is asked to place their hands flat against their upper thighs and the pelvis is rotated on the hips, without any back movement (trunk rotation sign), back pain when the knee and hip are flexed together, and exaggeration of pain on attempted straight-leg raise.
2. Further investigations should be resisted. Plain X-rays will show some degenerative changes, which are normal in middle age. MRI findings will either be normal or show minor abnormalities of doubtful significance. It is highly unlikely that an operable lesion will be identified or that a reputable surgeon would consider surgery. It is important not to over-medicalize such patients.
3. The first task of management is to explain that there is no pathological or anatomical abnormality that requires or will respond to invasive intervention. The patient has to be told that the pain is mechanical in origin and that the first line of management is physical rehabilitation, coupled with education about the nature and origin of the pain. Emphasis should be placed on regaining physical fitness and avoidance of activities that are likely to aggravate the pain. It is important to refer the patient to a physiotherapist or other therapist who regularly deals with patients with back pain and who is prepared to be involved over a significant period of time. Often a fitness trainer with an interest in this type of client is an alternative approach. If these approaches do not succeed, formal pain management, including cognitive behavioural therapy, should be considered.
Case 18 answers
1. The abnormality in the patient’s spinal canal produces a ‘trefoil’ outline. This is usually due to an arthritic (spondylitic in the spine) process that produces osteophytic overgrowth impinging on the canal, known as spinal stenosis.
2. This tends to pinch the spinal nerves. Below the cord (L1/L2), the cauda equina is compressed. Sometimes individual nerve roots are also compressed as they pass through their own exit foramina. It is thought that a ‘double’ compression, occurring at two levels, may be required to block microvascular blood supply to the nerve roots, leading to pain in the muscle supplied by one or more affected nerve roots. The symptoms are known as ‘claudication’ after the Roman emperor Claudius, who walked with a limp.
3. The diagnosis can be confirmed by excluding the other major cause of claudication – ‘intermittent’ or vascular claudication. This may require a vascular referral. A CT or MRI scan of the lumbo-sacral spine will confirm spinal stenosis. The side and level of maximum stenosis can often be identified, and this ought to correlate with the symptoms.
4. Sometimes caudal epidural steroid injections may help, but to be curative treatment is usually surgical. Decompression of the posterior elements (laminectomy) together with nerve root foraminal decompression is the commonest procedure.
Case 19 answers
1. Tennis elbow (lateral epicondylitis) is a painful overuse condition in which the common extensor tendon origin becomes inflamed and painful. The diagnosis is made by a suitable history of overuse (e.g. in tennis) of the extensor muscles of the forearm. The common extensor origin is tender, and forced extension of the wrist and digits against resistance increases the discomfort. This is usually self-limiting, and a period of rest and perhaps anti-inflammatory medication is all that is required to allow the symptoms to settle. Occasionally the condition becomes chronic. Ultrasound treatment, steroid injection and common extensor surgical release have been tried. A similar condition affects the common flexor origin (golfer’s elbow). The diagnosis is made in the same way.
2. Extensor digitorum communis, extensor digiti minimi, extensor carpi ulnaris, extensor carpi radialis brevis. (Brachioradialis and extensor carpi radialis longus originate from the supracondylar ridge.)
Case 20 answers
1. The most likely diagnosis is de Quervain’s disease. In this condition there is a pathological thickening within the wall of the sheath through which the tendons of extensor pollicis brevis and abductor pollicis longus pass to the thumb. This constricts the sheath causing pain when the thumb is moved. The thickening may be visible and palpable. Although this condition is often called stenosing tendovaginitis, it is not due to inflammation of the lining of the sheath. Anatomical variations such as sub-compartments of the sheath and multiple tendons are common and may be predisposing factors. The condition is most often seen in perimenopausal women and sometimes in the postpartum period, indicating that hormonal factors may be involved. It is not thought to be caused by work or repetitive movements, but when the condition is present such activities may provoke pain.
2. In Finkelstein’s test the thumb is passively adducted across the palm and the wrist is deviated in an ulnar direction. When the test is positive the discomfort that it provokes is accurately localized to the first dorsal compartment of extensor retinaculum of the wrist, which lies just proximal to the tip of the styloid process (see photograph overleaf).
3. The main differential diagnosis is osteoarthritis at the base of the thumb metacarpal, which is common in women in the same age group. The joints that are affected are the trapezio-metacarpal or scapho-trapezio-trapezoid joints (see Anatomy section, Chapter 1). When both joints are involved the condition is called pan-trapezial osteoarthritis. Osteoarthritis can be distinguished from de Quervain’s disease by physical examination. In osteoarthritis the discomfort is located distal to the radial styloid process. The pain is aggravated by compressing the joint by gripping the thumb ray and then twisting it (the grinding test, which should be done gently). X-rays will confirm the diagnosis.
4. Splinting the thumb will give temporary relief. A simple wrist splint is ineffective because it still allows the painful movements of the thumb. Most patients find that a splint is cumbersome and limits the ability to do daily tasks. The uncomfortable area may be infiltrated with a mixture of steroid and local anaesthetic, injected around the tendons. Surgical treatment involves releasing the tendons in the first dorsal compartment. Care must be taken to release all sub-compartments and it is particularly important that the incision does not damage the terminal branches of the radial nerve. The symptoms from the resultant neuroma may be considerably more disabling than the original condition.
Case 21 answers
1. Carpal tunnel syndrome. This is a fairly common condition in the later stages of pregnancy. The symptoms result from increased pressure on the median nerve in the carpal tunnel, beneath the flexor retinaculum at the wrist. Although unpleasant tingling (paraesthesia) usually occurs in the median nerve distribution, this is not invariable, and the whole hand may be affected. Symptoms are characteristically worse during the night or when holding the hands elevated, for example holding a phone or newspaper. Physical signs are usually absent. Wasting of the thenar muscles is not usually seen in this particular group, although it may occur in older women with carpal tunnel syndrome. Before wasting develops there may be weakness of abduction of the thumb. Phalen’s test involves holding the wrists flexed for 60 seconds. It is positive if the tingling is reproduced. Tapping on the median nerve at the base of the palm may again cause tingling (Tinel’s test). These tests are not particularly sensitive or specific, and the diagnosis should not be based solely on their presence or absence. Motor and sensory nerve conduction tests are more reliable and usually demonstrate slowed conduction in both motor and sensory fibres of the median nerve in the wrist.
2. When it occurs during pregnancy the condition is believed to be associated with increased fluid retention. Similar symptoms can occur when there is a space-occupying lesion within the carpal tunnel, for example a ganglion or proliferative synovium associated with rheumatoid arthritis. Most cases occur in middle-aged women without a clear cause and in these cases the condition is termed idiopathic carpal tunnel syndrome. Carpal tunnel syndrome may occur in endocrine disorders such as diabetes mellitus and hypothyroidism.
3. In most cases the symptoms resolve within a few weeks of childbirth.
4. Because the condition is likely to resolve, conservative treatment is preferred in pregnant patients. Wearing a splint on the wrist prevents the wrist going into flexion, which can trigger symptoms. An injection of steroid and local anaesthetic into the carpal tunnel may be helpful in resistant cases. Surgical release of the flexor retinaculum is rarely needed in this group, although it is usually the treatment of choice in older women with idiopathic carpal tunnel syndrome.
Case 22 answers
1. This is the typical appearance of Dupuytren’s disease, a proliferative disorder of the palmar and digital fascia of unknown cause. It is equally common in those who do not do heavy manual labour. There is often, but not always, a strong family history of the condition. It occurs in those of northern European origin and is quite rare in other racial groups. It is more common in men and becomes more common with age. In many cases the condition is mild, with slight nodularity in the fascia that does not interfere with function.
2. Dupuytren’s disease has been shown to be more common in people with a heavy alcohol intake, particularly those with alcoholic liver disease. However, it is a very common condition and its presence does not necessarily indicate that the person is a heavy drinker.
3. Dupuytren’s disease is very common in both type 1 and type 2 diabetics. The contractures tend to be milder in diabetics and the condition is more diffuse. There is a less clear association with epilepsy, which has not been clearly confirmed in all studies. Associated fibrotic conditions should be identified, such as Garrod’s pads (swellings over the proximal interphalangeal (PIP) joints of the fingers), Ledderhose’s disease (involvement of the plantar fascia) and Peyronie’s disease (fibrosis of the corpus cavernosum of the penis).
4. In many cases without significant contractures, simple advice is all that is required. Excision of early nodules in an attempt to prevent later contractures may have exactly the opposite effect by causing an increase in proliferative activity in the area of the scar. No regimens of splintage or exercise have been shown to be effective. Surgery is reserved for contractures that are interfering with function but no operation can cure the patient of Dupuytren’s disease, because it is programmed into that patient to form proliferative tissue in the fascia, either in the area of previous excision (recurrent disease) or elsewhere (extension of the disease). A strong family history, extensive palmar involvement and evidence of fibrotic disease elsewhere indicate a high likelihood of recurrence.
Case 23 answers
1. This is an ingrowing toenail. Infection of the lateral nail-fold has caused granulation tissue to form over the nail-plate.
2. Antibiotics on their own are not likely to resolve the condition and usually are indicated only if there is a surrounding cellulitis or lymphangitis. A wedge of the lateral nail-plate can be removed under local analgesia and this gives an opportunity for the granulation tissue to resolve. The nail-plate will regrow after wedge excision and is associated with about a 30% likelihood of the infection and granulation tissue recurring. Definitive treatment is ablation of the lateral part of the germinal matrix of the nail-bed using liquefied phenol BP or surgical excision of the nail-bed. The advantage of phenol over surgical excision is that it can be done in the presence of infection as phenol is an antiseptic agent.
Case 24 answers
1. Her red flag features included: older age, thoracic back pain, previous cancer history, non-mechanical pain and neurological picture (i.e. five relevant red flags).
2. There is a high chance of her clinical features being due to a metastatic cancer deposit, even though her breast cancer was diagnosed and treated 10 years earlier. After breast cancer, metastases can appear much later.
3. Because back pain in patients with cancer may signify a pathological fracture of a vertebra, manipulative treatment of the back pain is strongly contraindicated because it may lead to spinal cord damage.
4. Plain radiographs may show vertebral body collapse, but MRI and CT show much more detail, especially helping to differentiate between extradural soft-tissue metastasis and cord compression due to vertebral body fracture with collapse, i.e. a mechanical problem demanding a mechanical solution.
5. Initially, systemic steroids (dexamethasone) may be used to reduce oedema of the cord. If the spinal cord dysfunction is mild and the cord compression is due to extradural soft-tissue tumour, radiotherapy and chemotherapy may suffice. If there is mechanical bony compression of the cord, surgical decompression is best with instrumentation to stabilize the pathological fracture. The surgical procedure will be planned according to the position of the pathology; in this case it is mostly anterior so, ideally, the surgical procedure would be anterior thoracotomy with removal of the diseased vertebral body and interbody fusion using instrumentation and bone grafting. In cases with a poorer prognosis, the decompression can be carried out posteriorly with supporting instrumentation. Radiotherapy would be used as an adjunct. Treatment is palliative rather than curative with rehabilitation according to the degree of disability. Bone pain can be controlled by bisphosphonates. Diamorphine may be required.
Case 25 answers
1. The X-ray shows an osteochondroma, so called because it has a bony base (osteo-), a cartilage cap (-chondro-) and is a benign tumour (-oma). About 1% of children will develop a noticeable osteochondroma. The diagnosis is made on clinical examination and X-ray. Most are asymptomatic, but sometimes they can cause discomfort when muscle or tendon rubs over the surface of one. An osteochondroma will usually grow up to skeletal maturity and then stop, although occasionally it may continue to grow into adulthood. It is thought to arise from the perichondrial ring that surrounds the childhood growth plate, because the histological appearance of the cartilage cap is quite similar to the columnar architecture of the growth plate.
2. It is important to check for other osteochondromas. If they occur, the condition may be hereditary multiple exostoses (HME), an autosomal-dominant inherited condition affecting about 1 in 50 000 people in which many osteochondromas are found. In this condition there is often short stature, deformity of forearms and legs, and occasionally malignant change in an osteochondroma to form a chondrosarcoma in adulthood (less than 5% of HME).
3. Treatment mostly depends upon symptoms. Many painful osteochondromas will settle with observation, but sometimes excision is warranted. In HME, removal of osteochondromas is quite common, and correction of long-bone deformity may also be required.
Case 26 answers
1. This X-ray shows a cemented total hip replacement. The implant is loose at both the acetabular and femoral sides of the joint because there is a clear surrounding lucency at the bone–cement interface. Proof of this would be gained by performing a hip arthrogram in which radio-opaque contrast is injected into the artificial hip joint under aseptic conditions and X-ray control. Contrast leaking into the bone–cement interface indicates loosening. Loosening can be either septic or aseptic. An aspiration sample taken at the same time as the arthrogram can be sent for microbiology, but a negative result does not exclude infection entirely. Loosening at 15 years after primary surgery, however, is much more likely to represent an aseptic process.
2. All non-biological implants will eventually fail under load. The natural history of aseptic loosening at the bone–cement interface is one of progressive symptoms, with progressive cortical and medullary osteolysis through bone phagocytosis. Eventually the femur may fracture, or the acetabular component may spin or even perforate into the pelvis.
3. Treatment depends upon the patient’s general condition, but if an improvement in mobility is anticipated in a resilient patient then revision total hip replacement could be undertaken. Outcome overall is often satisfactory, but this is a much more extensive procedure than the primary operation with a higher general complication rate, and a lower implant survival rate.
Case 27 answers
1. The likely diagnosis is infection within the total knee replacement. The clinical picture of pain, redness, swelling and heat is one of acute inflammation, possibly with a pointing abscess.
2. Temperature and inflammatory markers (white cell count, ESR, CRP) may be raised. A knee arthrogram could be performed. Here radio-opaque contrast is injected into the artificial knee joint under aseptic conditions and X-ray control. Contrast leaking into the bone–cement interface indicates loosening. An aspiration sample taken at the same time as the arthrogram can be sent for microbiology, but a negative result does not exclude infection entirely.
3. If there is a clinical abscess, surgery to drain and debride the knee replacement is indicated. Septic loosening of the prosthesis means that a simple ‘washout’ will not suffice, and revision of the prosthesis should be undertaken. Early debridement of a possibly infected joint replacement is preferable to late debridement, and hence careful clinical observation in the immediate postoperative phase is vital. This may be performed as a single-stage procedure, in which the implants are replaced with new ones during the same operative procedure. Alternatively a two-stage procedure can be undertaken in which the new prosthesis is implanted several weeks after removal of the infected components. In the intervening period a ‘cement spacer’ is often interposed between the femur and tibia, and appropriate antibiotics are given. The advantage of a two-stage revision is that the re-infection rate is low, but patient morbidity may be higher.
Case 28 answers
1. The nursing chart is a record of postoperative patient observations; here a selection is recorded. Both pulse and blood pressure are rising, supporting evidence for an increasing level of pain. Leg sensation and power are recorded because of spine surgery adjacent to nerve roots supplying the lower limbs. Any life- or limb-threatening deterioration should be detected early by this chart.
2. The doctor should be informed when pain is not controlled by prescribed medications, and certainly when a deterioration in neurology is first detected (by 16.00 hours).
3. The likely diagnosis is a compressive lesion affecting the nerve roots. This is usually due to an acute haematoma. An emergency MRI scan should be undertaken to confirm the diagnosis, followed by immediate surgical evacuation of the haematoma.
Case 29 answers
1. The picture described is of a myelopathy that is affecting the lower limbs, but also certain parts of the upper limbs. If the upper limbs were normal there could be a problem in the thoracic cord, but with the upper limb involvement the lesion must be in the cervical spine. The lack of pain is typical and is partly responsible for the fact that myelopathy does not present until the condition is well advanced.
2. The jaw reflex is normal, so placing the lesion below brain level. The biceps and brachioradialis reflexes are normal, but the abnormal triceps reflexes means that there is cord pathology at a level between the sixth and seventh cervical vertebrae (C6/7). The knee reflexes are brisk as one would expect, but the ankle reflexes and plantar responses are inhibited by the presence of a diabetic peripheral neuropathy.
3. The MRI scan shows a minor abnormality at C5/6, but a more significant stenosis at C6/7 due to a combination of disc and osteophyte narrowing the spinal canal and compressing the spinal cord. The level of this pathology would exactly explain the neurological picture.
4. Cervical myelopathy carries a variable prognosis and sometimes remains static for long periods of time. However, when there is evidence of a quadriparesis and a rapidly deteriorating myelopathy, there is an inevitable progression to severe disability with loss of all useful function in the hands and legs. No conservative treatment is helpful, but operative decompression can halt the progression of the condition. Modest improvement of function is possible, but complete recovery is unlikely except in early and mild cases.
Case 30 answers
1. The high ESR and general malaise suggest more serious pathology including neoplasia and infection. An ESR greater than 100 mm/h raises the possibility of myeloma in middle-aged patients. The plasma proteinaemia and monoclonal gammopathy are in keeping with the diagnosis of multiple myeloma.
2. The C6 radiculopathy and myelopathy suggest a condition at the C5/6 level with compromise of the sixth cervical nerve and spinal cord itself. This could mean a reduced biceps reflex, but increased triceps and lower-limb reflexes.
3. As well as the blood tests mentioned above, Bence Jones protein may be found in the urine. Plain radiographs of the neck show loss of density of the C5 vertebra with collapse of the vertebral body. MRI shows collapse of the vertebral body and axial slices show a major soft-tissue abnormality extending on the left side of the midline, impinging upon the spinal cord and encompassing the sixth cervical nerve. A needle biopsy under X-ray guidance should be carried out and the tissue samples examined histologically and by tissue culture for the possibility of infection.
In this patient, the diagnosis of multiple myeloma was confirmed.
4. The neurological problems – radiculopathy and myelopathy – were treated by anterior vertebrectomy of the diseased sixth cervical vertebra with anterior cervical fusion using bone-graft and plate fixation. Decompression rapidly improved the pain and neurological deficit, but was clearly not the answer to the neoplastic process. Therefore, radiotherapy to the cervical spine was indicated together with the appropriate chemotherapy to control the myeloma.
Case 31 answers
1. The most likely problematic level is at C4/5 because the clinical features suggest a C5 nerve deficit (weak biceps and diminished sensation in the C5 dermatome see Chapter 1). MRI or CT of the cervical spine is indicated.
2. Treatment should be conservative because the natural history of multi-level cervical spondylosis is variable and unlikely to require surgery. Physiotherapy with traction and manipulation can help, as can other techniques, such as acupuncture and transcutaneous nerve stimulation. The changes seen on this scan would be equivalent to those on scans of asymptomatic subjects, so caution should be exercised to avoid over-treatment of the changes that may simply reflect benign degenerative changes associated with ageing.
3. If symptoms persisted and were troublesome enough, a local decompression and fusion could be considered.
Case 32 answers
1. The differential lies between acute septic arthritis of the hip and acute osteomyelitis of the femur. Both may present in a similar manner and the posture of the child is characteristic. In a larger child it may be possible to demonstrate discrete swelling and tenderness overlying the femur in osteomyelitis, but such distinction may be difficult in the younger child. The history of preceding upper respiratory tract infection raises the possibility of transient synovitis or ‘irritable hip’, but this would be unlikely to result in such high levels of the inflammatory markers.
2. An ultrasound scan is simple, safe and non-invasive, but should be interpreted with care. An effusion in the hip joint does not exclude a proximal femoral osteomyelitis, because there may be a sympathetic effusion in the adjacent joint. However, absence of an effusion would point towards osteomyelitis as the cause, and detection of a sub-periosteal pus collection would confirm the diagnosis. Aspiration of any effusion under ultrasound control may help distinguish between infected and sympathetic collections. Isotope bone scanning may be used on occasion to localize the site of infection, but it may not be readily available as an emergency and there are concerns about radiation. MRI will clearly distinguish between a primary septic arthritis and acute osteomyelitis, but this may not be available as an emergency investigation.
3. If septic arthritis is suspected, blood cultures should be taken. The joint should be aspirated or opened, to obtain infected material for culture and also to decompress the joint. Appropriate antibiotic therapy should then be started and given intravenously initially. If acute osteomyelitis is suspected, intravenous antibiotics prescribed on a ‘best guess’ basis should be started and the progress closely monitored by the child’s temperature and serial estimation of inflammatory markers. Ultrasound evidence of a sub-periosteal collection that fails to resolve may be an indication for surgical drainage of pus. In both scenarios, supportive measures such as pain control, nutritional support and close watch on fluid balance are important.
Case 33 answers
1. An Asian person with a generalized illness and spinal trouble demands early investigation for a possible diagnosis of tuberculosis (TB) of the spine.
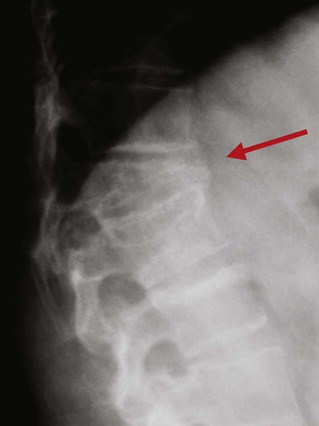
2. Plain radiographs of the spine show loss of definition of the disc space and may show erosion of the end-plates (see figure).
3. Treatment: rest in an orthosis and anti-tuberculous chemotherapy may suffice, even in the presence of an epidural abscess, but if there is no clinical improvement surgical drainage and instrumented spinal fusion may be required. This patient improved on chemotherapy alone. Therapy with two or three anti-tuberculous drugs continues for at least 6 months. It is important to monitor treatment progress by weekly measurement of inflammatory markers. Serial radiographs and MRI scans can also be helpful in assessing resolution of the infection. The natural history of a tuberculous spondylodiscitis is to heal by a process of ankylosis with bony bridges forming to immobilize the affected motion segment.
Case 34 answers
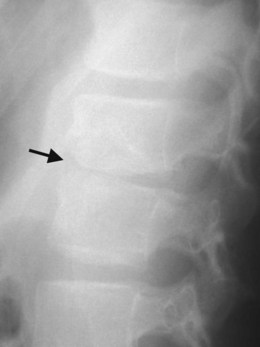
1. There is a spondylolisthesis of the fifth lumbar vertebra on the sacrum. Spondylolisthesis is classified according to the degree of slip of the AP diameter of the vertebral body upon the vertebra below. Grade I is a 0–25% slip, grade II 25–50%, grade III 50–75%, grade IV 75–100%, and grade V (‘spondyloptosis’) is where the vertebra has slipped right off the vertebra below.
2. Bilateral pars interarticularis defect. The slip often develops gradually and there may be adaptation of the tissues with few deleterious effects. Although the spondylolisthesis can present in childhood with back pain, a spinal deformity, tight hamstrings and even neurological deficit (numbness, weakness and sphincter disturbance), it is just as likely to be picked up in adulthood in the course of investigation for chronic back pain and it can turn up as an incidental finding during investigation of other conditions.
3. Treatment of spondylolisthesis depends upon the cause, the degree and the severity of symptoms. Most forms of spondylolisthesis can be managed conservatively with only a small proportion needing spinal fusion. By the time a patient reaches the age of 30 years the spondylolisthesis usually stabilizes spontaneously and any back pain is just as likely to have a completely separate cause. The young patient with severe symptoms and an unstable slip is different and there is good evidence that a spinal fusion with bone grafting in situ will suffice. Pain is relieved and the relief of hamstring muscle spasm improves the posture and sagittal balance. This girl underwent surgery.
Case 35 answers
1. The patient has sustained a fracture of the mid-shaft of the clavicle. This is a very common injury and the treatment of choice is non-operative. Patients are provided with a sling and analgesia. Regular follow-up is required to ensure the fracture progresses to union, which normally occurs in adults within 2–3 months of injury.
2. The radiographs at 12 weeks indicate there has been no progression to union. Non-union is a well recognized complication of clavicular fractures in adults and occurs in 10% of cases. It is more common in fractures with more than 1 cm of displacement between the bone fragments or in those with comminution.
3. The most appropriate treatment is plating, occasionally with bone grafting. This is successful in obtaining union in more than 90% of cases. The radiograph below shows the bony union progressing after plating.
Case 36 answers
1. The patient has sustained an anterior dislocation of the shoulder. The humeral head has come to lie in a sub-coracoid position. Anterior dislocations account for 95% of shoulder dislocations. The other directions encountered in clinical practice are posterior and the very rare ‘luxatio erecta’ when the humeral head dislocates in an inferior direction.
2. Anterior dislocations may be complicated by traction nerve injuries, most commonly involving the axillary nerve. However, in older patients brachial plexus palsies are not unusual. Rotator cuff tears are also frequent in patients over the age of 40 years who sustain a shoulder dislocation. These are difficult to diagnose at the time of the dislocation. They should be suspected in patients who fail to mobilize the shoulder in the weeks following injury.
3. A closed reduction under sedation is the most appropriate treatment for the acute case. A period of immobilization in a sling for a period of 4–6 weeks is usually recommended for younger patients to minimize the risk of recurrent dislocation. In patients over the age of 40 years the risk of recurrent dislocation is small and early mobilization can safely be attempted once the initial pain and swelling have settled.
Case 37 answers
1. The patient has sustained a fracture dislocation of the shoulder.
2. The humeral head is visible in a dislocated position. Note that the head is separated from the humeral shaft and the greater tuberosity. The lesser tuberosity is not visible as a separate fragment and is probably still attached to the humeral head.
3. This is a high-energy injury and there is a significant risk of an associated axillary nerve neuropraxia or even a brachial plexus injury. There is also a risk of fractures elsewhere. Clinical examination should, therefore, be conducted with these possibilities in mind. The neurological status was actually normal. However, there was a painful deformed wrist and radiography confirmed a comminuted intra-articular distal radial fracture.
4. Options for treatment: non-operative treatment is not feasible in this situation. A closed reduction of the dislocated head is impossible because it is separated from the humeral shaft. The choices are either open reduction and internal fixation or replacing the humeral head with a shoulder hemi-arthroplasty. Internal fixation is feasible if the bone is of good quality and the humeral head has an adequate soft-tissue attachment to provide a blood supply. Surgical exploration was carried out. This revealed that the bone was very osteoporotic and the lesser tuberosity was also detached from the humeral head. The humeral head, therefore, had no soft-tissue attachments and in this situation (a four-part fracture dislocation) shoulder joint replacement (see figure) was a better option. This was performed and the patient made a satisfactory postoperative recovery. The distal radial fracture was considered unstable because it was very comminuted and it was treated with external fixation. She should have her falls and osteoporosis risk factures assessed and managed appropriately.
Case 38 answers
1. Fractures of the humerus are associated with injury to the radial nerve in 10–15% of cases. If the patient lacks active dorsiflexion of wrist then a radial nerve palsy is likely to be present.
2. Physical examination is rendered difficult in the presence of a humeral shaft fracture. The radial nerve supplies all the muscles involved in extension of the arm, forearm and wrist. It supplies triceps, brachioradialis, supinator, extensor carpi radialis brevis and longus, extensor carpi ulnaris, extensor digitorum communis, extensor pollicis longus and abductor pollicis longus. In patients with humeral shaft fractures it is usually possible to test the wrist, finger and thumb extensors. If a radial nerve palsy is found, an area of numbness involving the dorsal aspect of the first web space is also present.
3. The treatment of choice for an isolated closed humeral shaft fracture is non-operative. A plaster U-slab is applied. This can be changed to a functional brace at 3–4 weeks. Union will occur in more than 95% of cases between 8 and 12 weeks.
4. Operative treatment is indicated in patients whose fractures fail to heal or show signs of progression to union with the 8–12-week time-frame. Some fractures cannot be maintained in a satisfactory position in a cast and this is also an indication for internal fixation. However, modest degrees of mal-union are well tolerated in the humerus and up to 20° of angulation or rotation can be tolerated without functional limitation. Fixation is also generally indicated in patients with multiple long bone fractures, open humeral fractures and humeral fractures with a vascular injury. An isolated radial nerve palsy in itself is not an indication for fixation.
5. Plating is the preferred method of fixation for humeral shaft fractures. The other main alternative is intra-medullary nailing. This has been associated with a higher complication rate in clinical practice than plating. Intra-medullary nails are inserted at the shoulder or the elbow. If inserted at the shoulder they are often associated with pain due to penetration of the rotator cuff. The elbow entry point is at a relatively weak bony point and iatrogenic fracture may occur. Non-union has also been more common with intra-medullary nailing. The humerus is subject to a lot of torsional force during normal use. Plates are good at resisting this type of force. Nails, by comparison, are less suited to resisting torsional motion. This excess motion at the fracture site contributes to a higher risk of non-union. Nails may be preferable for segmental fractures where the bone is fractured at two locations. Nails are also more suitable for treatment of pathological fractures.
Case 39 answers
1. This is a humeral supra-condylar fracture and is a common elbow injury in children.
2. The brachial artery and median nerve have been contused by the injury or the fracture haematoma has caused some local pressure on these two structures.
3. X-ray the limb and apply temporary splintage. Provide intravenous or intranasal analgesia. The child should be admitted to the ward prepared for theatre and have their pulse and sensation checked regularly. Loss of the pulse and an ischaemic hand is a surgical emergency.
4. The fracture is reduced under general anaesthesia and pinned using percutaneous wires. The fracture will heal rapidly and the wires can be removed at 3 weeks as an outpatient procedure without the need for general anaesthesia.
Case 40 answers
1. The patient has sustained a fracture dislocation of the elbow. There is a dislocation with an associated fracture of the coronoid process of the ulna and a radial head fracture. This combination of injuries is often referred to as the ‘unhappy triad’ of the elbow, signifying that it is a well recognized injury pattern commonly associated with a poor outcome. It is often the result of high-energy trauma, and a careful clinical evaluation should be part of the initial work-up to detect any associated neurovascular problems or signs of fractures elsewhere in the upper limb.
2. This injury is not amenable to non-operative treatment. The presence of the coronoid process fracture and the radial head fracture greatly increases the instability of the elbow and an adequate closed reduction cannot be maintained. These injuries require internal fixation of the coronoid process to restore ulno-humeral stability. The fracture is exposed through a posterior approach. The proximal ulnar shaft and coronoid fracture is reduced and fixed with a plate. The options for the radial head fracture are either reduction and fixation with screws, if there are no more than three main fragments, or, if there is more comminution than this, a radial head replacement is preferred.
3. The most common complication following an injury of this severity is elbow stiffness. Heterotopic ossification of the elbow is not unusual after injuries of this type and the extensive surgery required. If this occurs, the stiffness may be severe and disabling. The functional range of motion required for normal elbow activities is 30–120°. If the range of motion is less than this then normal activities of daily living may be interfered with. Elbow stiffness can be minimized if the internal fixation has secured a good-quality stable reduction that allows early motion and avoids the need for prolonged immobilization. Physiotherapy to supervise rehabilitation is helpful. If stiffness occurs and causes significant disability, further surgery to carry out a soft-tissue release can be performed, usually 4–6 months after the initial injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree