Anomalous Pulmonary Venous Connections
Kent E. Ward
Partial anomalous pulmonary venous connection (PAPVC) occurs when one or more, but not all, pulmonary veins connect anomalously to the right atrium, either directly or through a systemic venous tributary. PAPVC, which often is found in association with an atrial septal defect (ASD), demonstrates hemodynamic findings of an acyanotic cardiac lesion with increased pulmonary blood flow similar to that observed in an ASD alone.
When all pulmonary veins connect anomalously to the systemic venous circulation, total anomalous pulmonary venous connection (TAPVC) is defined. TAPVC is associated with total mixing of pulmonary and systemic venous blood at the level of the right atrium and, as such, is defined as a cyanotic form of cardiac disease that may demonstrate increased or decreased pulmonary blood flow. Increased pulmonary blood flow is usual. Decreased pulmonary blood flow may occur when severe obstruction in the anomalous pulmonary venous channel is present. In addition, TAPVC always is associated with an interatrial communication, usually a patent foramen ovale.
EMBRYOLOGY
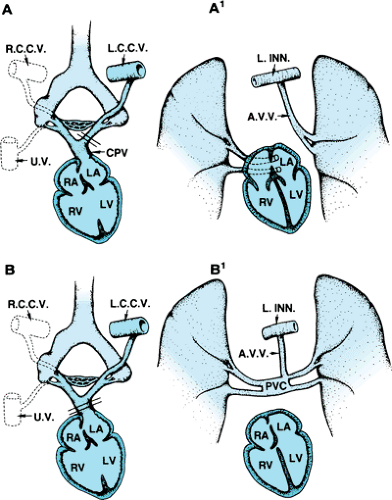
A review of the embryologic development of the systemic and pulmonary venous systems is necessary to understand fully the abnormalities observed in this spectrum of cardiac defects. In the developing embryo, the primitive foregut gives rise to the lungs, larynx, and tracheobronchial tree. The primordial lung buds share a common vascular plexus (splanchnic plexus) with other derivatives of the foregut and, early on, drain through the paired common cardinal and umbilicovitelline veins. As development proceeds, this splanchnic plexus differentiates into the primitive pulmonary vascular bed, thus becoming committed to draining pulmonary venous blood. This pulmonary vascular bed, however, remains in communication with the cardinal and umbilicovitelline system of veins until later in development. At 27 to 29 days of gestation, a small endothelial outgrowth arises from the posterior superior wall of the primordial left atrium. This outgrowth, called the common pulmonary vein, merges with the splanchnic plexus and begins to drain blood from this region. If development proceeds normally, the pulmonary portion of the splanchnic plexus loses connections with the cardinal and umbilicovitelline venous systems. Tributaries to the common pulmonary vein coalesce to form two pulmonary veins that drain each lung. If the right or left portion of the common pulmonary vein becomes atretic or loses connection with the pulmonary plexus, persistence of the primitive pulmonary venous–systemic venous connection on that side leads to PAPVC. If the common pulmonary vein–left atrium connection is disrupted totally, TAPVC occurs (Fig. 277.1).
PARTIAL ANOMALOUS PULMONARY VENOUS CONNECTION
PAPVC is a relatively common occurrence and is found in 0.6% of all autopsy studies. The relatively high incidence of this defect observed in autopsy specimens supports the contention that many cases of PAPVC do not produce symptoms and thus are not diagnosed during life. In order of decreasing frequency, the most common types of PAPVC encountered are right pulmonary veins to right superior vena cava, right pulmonary veins to right atrium, right pulmonary veins to inferior vena cava, and left pulmonary veins to the left innominate vein. Connection from the right lung anomalously occurs approximately twice as often as does that from the left lung.
Clinically apparent PAPVC usually is found in association with other cardiac defects, most commonly an ASD of the secundum or sinus venosus type. PAPVC from the right lung to the inferior vena cava occurs in the scimitar syndrome, a complex of anomalies that includes pulmonary hypoplasia or sequestration, diaphragmatic abnormalities, and anomalous systemic arterial supply to the right lung. Both scimitar syndrome and isolated PAPVC have been diagnosed prenatally using fetal echocardiography and Doppler color flow imaging as early as 20 weeks of gestation.
Hemodynamics and Clinical Features
The basic hemodynamic alteration that occurs in PAPVC is that of a pretricuspid left-to-right shunt in which fully oxygenated blood is recirculated through the lungs via the right atrium, right ventricle, and pulmonary artery. The increased pulmonary blood flow leads to enlargement of the right atrium, enlargement and hypertrophy of the right ventricle, and dilatation of
the pulmonary artery. The left heart chambers are not affected, and systemic cardiac output is normal. Most patients with PAPVC, with or without an interatrial communication, do not exhibit symptoms in early life. These patients often are referred with a cardiac murmur or an abnormal chest roentgenogram. When symptoms are elicited at this age, the most common complaint is mild intolerance for exercise. Progressive symptoms, if they appear, usually begin when the patient is in the mid-thirties or early forties. They consist of dyspnea, recurrent bronchitis, hemoptysis, chest pain, and palpitations associated with supraventricular arrhythmias. Physical examination in patients with isolated PAPVC may be normal if only a single lobe connects anomalously. When multiple lobes are involved or when an associated ASD is present, the findings are typical of an uncomplicated ASD. Occasionally, a low-frequency continuous murmur may be heard over the base, representing flow through an anomalous venous channel. The electrocardiogram usually demonstrates right ventricular hypertrophy, although it may be normal in patients without associated cardiac defects. Atrial arrhythmias are rare occurrences in the infant and child, but they may occur in the third and fourth decade of life and usually are associated with an ASD or mitral stenosis.
the pulmonary artery. The left heart chambers are not affected, and systemic cardiac output is normal. Most patients with PAPVC, with or without an interatrial communication, do not exhibit symptoms in early life. These patients often are referred with a cardiac murmur or an abnormal chest roentgenogram. When symptoms are elicited at this age, the most common complaint is mild intolerance for exercise. Progressive symptoms, if they appear, usually begin when the patient is in the mid-thirties or early forties. They consist of dyspnea, recurrent bronchitis, hemoptysis, chest pain, and palpitations associated with supraventricular arrhythmias. Physical examination in patients with isolated PAPVC may be normal if only a single lobe connects anomalously. When multiple lobes are involved or when an associated ASD is present, the findings are typical of an uncomplicated ASD. Occasionally, a low-frequency continuous murmur may be heard over the base, representing flow through an anomalous venous channel. The electrocardiogram usually demonstrates right ventricular hypertrophy, although it may be normal in patients without associated cardiac defects. Atrial arrhythmias are rare occurrences in the infant and child, but they may occur in the third and fourth decade of life and usually are associated with an ASD or mitral stenosis.
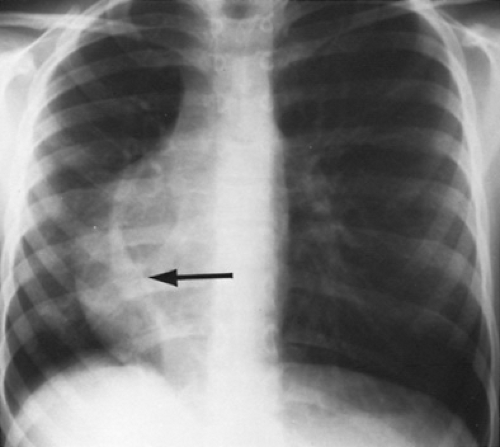
In the presence of an ASD, the chest roentgenogram often shows evidence of right atrial and right ventricular enlargement in addition to increased pulmonary vascularity. Specific radiographic findings related to the insertion or drainage of the anomalous pulmonary vein or veins are described well, the scimitar sign being a classic example (Fig. 277.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree