(1)
Department of Orthopedic Surgery Academic Medical Centre, University of Amsterdam, Amsterdam, The Netherlands
Abstract
This chapter deals with acute and chronic lateral ankle ligament lesions. The various considerations concerning anatomical reconstruction and tenodesis are described in detail. Nowadays anatomical reconstruction of the lateral ankle ligament is regarded as the surgical treatment of choice in patient with chronic ankle instability. In case of insufficient remnants, a free graft is used. These techniques are described in detail. The place for arthroscopic stabilization is given and the operative technique is described in detail. Finally, this chapter deals with subtalar instability.
Anatomical reconstruction of the lateral ankle ligaments is the surgical treatment of choice in patient with chronic ankle instability (De Vries et al. 2011). In case of insufficient remnants, a free graft can be used.
The anterior talofibular ligament is the most important stabilizer of the ankle joint. It is the first ligament to rupture during an inversion trauma. Therefore, the anterior drawer test is the most important test for detection of acute and chronic ankle instability.
The anterior drawer is not a straightforward translation of the talus in relation to the tibia, but it is a rotatory movement (Van Dijk 1994). This rotation is caused by the intact deltoid ligament which prevents the talus to move forward on the medial side.
Unlike an anatomical reconstruction, tenodesis does not restore the normal anatomy of the lateral ankle ligaments. Tenodesis procedures may result in a restricted range of ankle and subtalar motion, a higher number of reoperations, impairment of athletic performance, and a higher percentage of unsatisfactory functional results.
9.1 Anatomy
The ankle joint is the most congruent joint of the human body (Fig. 9.1). Stability is provided by the bony configuration of the ankle mortise, the talar dome, and the ankle ligaments. During ankle motions, both rotation and translation around and along the movement axes occur. Soft tissue stability is provided by the ligaments; these are the tibiofibular syndesmosis, the deltoid ligament on the medial side and on the lateral side, the anterior talofibular ligament, the calcaneofibular ligament, and the posterior talofibular ligament (Fig. 9.2) (Wiersma and Griffioen 1992). The anterior talofibular ligament is an intra-articular reinforcement of the joint capsule. This ligament is the main stabilizer on the lateral aspect of the ankle and the most vulnerable to injuries (Van den Bekerom et al. 2008) (Fig. 9.3). The orientation of the anterior talofibular ligament is in a plane parallel to the axis of movement (flexion-extension), provided the ankle is in a neutral position. The anterior talofibular ligament is a true collateral ligament when the foot is placed in plantar flexion. Most ankle ligament injuries occur by internal rotation in equinus position with the foot in plantar flexion, when the narrowest part of the talus is placed in the ankle mortise and the ankle is lax. This is one important reason for the high incidence of injuries of the anterior talofibular ligament (Broström 1966; Rasmussen and Kromann-Andersen 1983; Fallat et al. 1998) (Fig. 9.4).

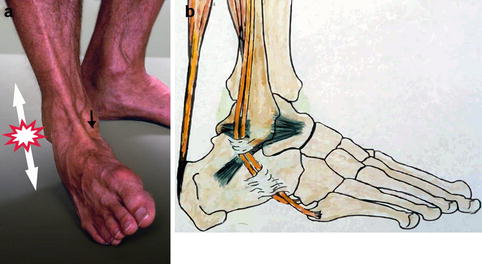
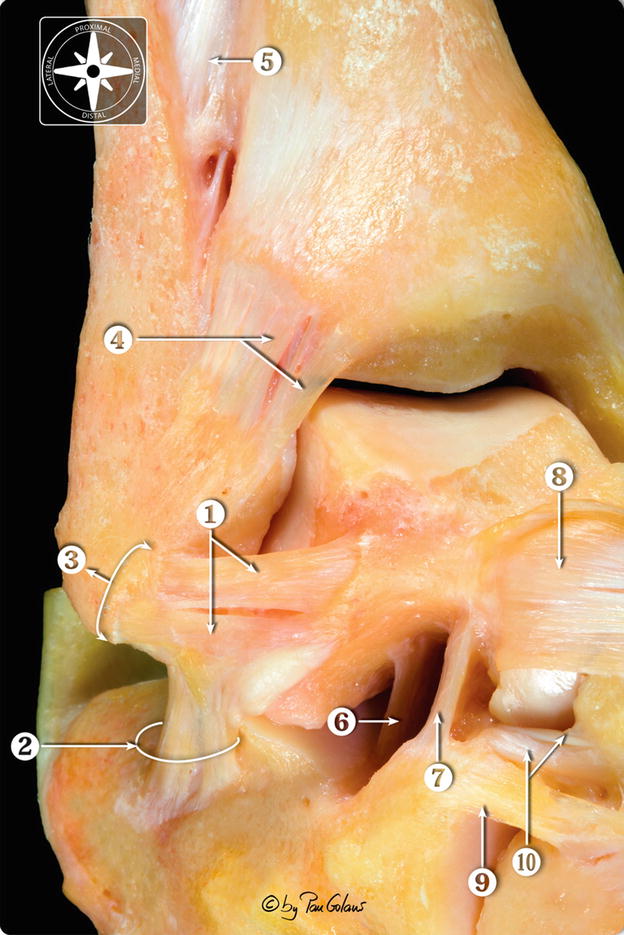
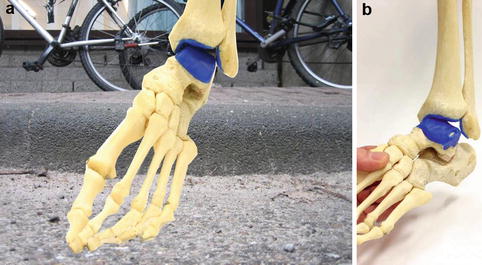

Fig. 9.1
Frontal section of the ankle joint, the most congruent joint of the human body (With kind permission of © Pau Golanó 2013)
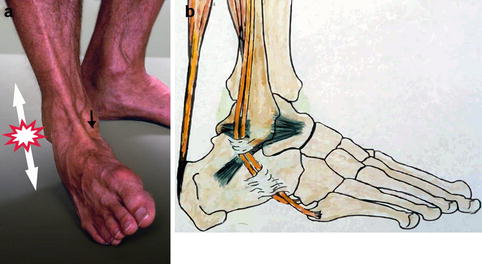
Fig. 9.2
(a) Supination result in distraction forces (white arrows) on the lateral side and compression (black arrow) on the medial side. (b) Schematic drawing of the three lateral ankle ligaments: ATFL (anterior talofibular ligament), CFL (calcaneofibular ligament), and PTFL (posterior talofibular ligament)
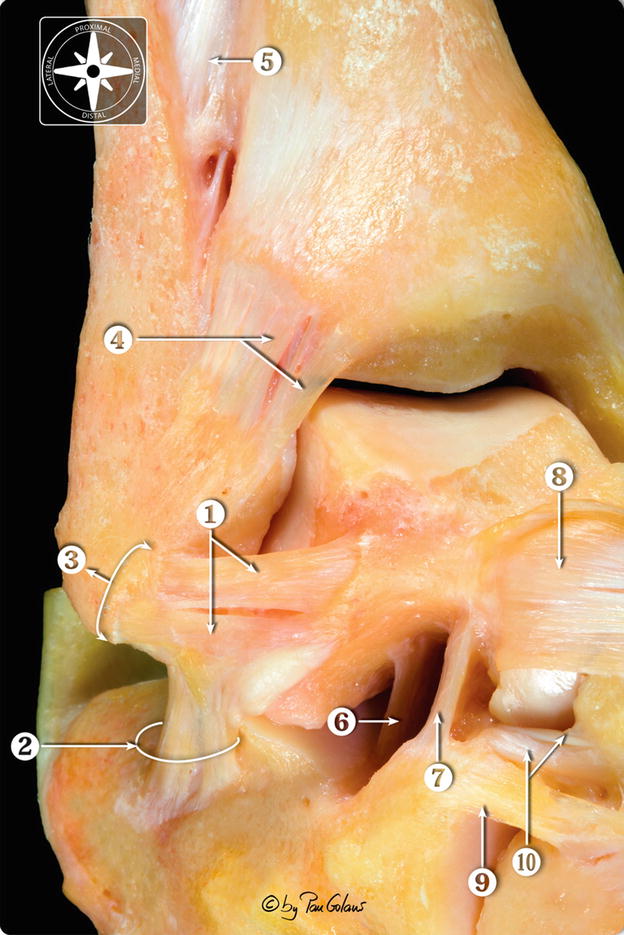
Fig. 9.3
Anterolateral view of the osteoarticular dissection of the foot and ankle. 1 Anterior talofibular ligament (two bundles). 2 Calcaneofibular ligament and the lateral talocalcaneal ligament. 3 Common insertion (usually) of the anterior talofibular ligament and lateral talocalcaneal ligament. 4 Anterior tibiofibular ligament and distal fascicle. 5 Interosseous membrane. 6 Interosseous talocalcaneal ligament. 7 Cervical ligament. 8 Dorsal talonavicular ligament. 9 Dorsolateral calcaneocuboid ligament. 10 Bifurcate ligament (With kind permission of © Pau Golanó 2013)
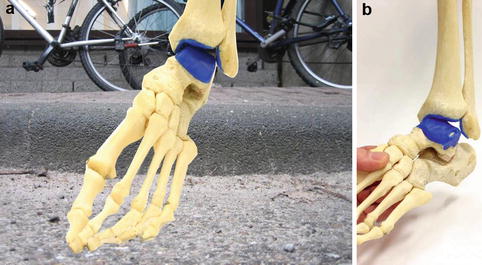
Fig. 9.4
(a and b) Supination of the right foot. Supination results in distraction forces on the lateral side and compression on the medial side. In most cases, this will result in a rupture of one or two of the lateral ankle ligaments and compression between the anterior part of the medial malleolus and the tip of the medial malleolus with the opposite medial talar facet resulting in local cartilage damage of the anteromedial rim and medial talar facet
The extra-articular calcaneofibular ligament inserts on the anterior part of the tip of the fibula. In most cases, a bundle of fibers runs directly from the calcaneofibular ligament to the anterior talofibular ligament. In some cases, the calcaneofibular ligament attaches predominantly to the anterior talofibular ligament (Wiersma and Griffioen 1992; Van Dijk 1994). The calcaneofibular ligament runs obliquely downward and backward to attach to the lateral surface of the calcaneus. The calcaneofibular ligament is intimately associated with the posteromedial part of the peroneal tendon sheath. It bridges the talocrural and the subtalar joint (Fig. 9.5). The posterior talofibular ligament is a short and thick ligament. The posterior talofibular ligament is tight with the ankle in extension and lax in plantar flexion. Injuries to this ligament are infrequent, and the ligament is not used as a part of a reconstructive procedure.
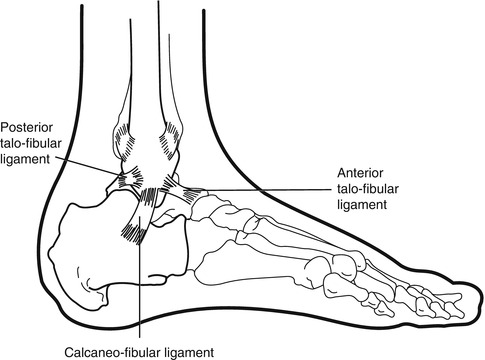
Fig. 9.5
The lateral ankle ligaments
The distal tibiofibular syndesmosis provides the stability of the ankle mortise. A combination of forced external rotation, dorsiflexion, and axial loading of the ankle has demonstrated to cause a rupture of the anterior tibiofibular ligament (Broström 1966; Rasmussen and Kromann-Andersen 1983). This is accompanied by a (partial) rupture of the deltoid ligament. The main stabilizer on the medial side is the deep portion of the deltoid ligament, a fan-shaped, thick, and strong ligament.
Anatomical variations in shape, size, orientation, and capsular relations of the lateral ankle ligaments are common. The anterior talofibular ligament is divided into two separate bundles in one-third of all patients (Van Dijk 1994). These anatomical variations have to be considered when surgical reconstruction is performed (Kannus and Renström 1991).
9.2 Acute Ligament Injuries
Acute ankle ligament injuries are the single most common type of injuries seen by general practitioners and emergency departments. They involve about 25 % of all injuries of the musculoskeletal system with over 20, 000 patients in the USA each day (Klenerman 1998; Van Dijk 1994). In about 10–15 % of all inversion traumas, a rupture of the lateral ankle ligaments is present (Hamilton 1994).
In most cases, the lateral ligament injury occurs with the foot rotating inward in plantar flexion when the tibia is simultaneously rotating outward, giving rise to anterolateral rotational movement. The medial malleolus acts as a fulcrum when the ankle moves into increased inversion, losing its stabilizing function and increasing the strain on the lateral side (Fig. 9.4).
Ankle ligament injuries are often classified as grade I (mild), grade II (moderate), and grade III (severe) (Konradsen et al. 1991). Grade I injuries include stretching of the ligament without macroscopic rupture. There is a minor swelling and tenderness and not an increased laxity. The loss of function is minimal and the recovery is usually quick. In grade II injuries, there is a partial macroscopic rupture of the ligaments, with moderate swelling, tenderness, and pain. There is a mild to moderate increment of laxity, some loss of motion, and moderate functional disability.
Grade III injuries always include a complete rupture of the ligaments and the joint capsule, with severe bruising, swelling, and pain. There is a major loss of function, reduction of motion, and increased laxity due to the ligament rupture. The value of this classification is doubtful, since a partial rupture or isolated capsular lesion (grade I) is present in less than 1 % of cases. The outcome of several studies has shown that there is no difference between the prognoses of a single (grade II)- and multiple-ligament ruptures (grade III) (Van Dijk 1994, 2005; Van Dijk et al. 1996a). Therefore, after a supination trauma, it is important to distinguish a simple sprain from a ligament rupture.
It has been shown that a rupture of the anterior talofibular ligament occurs as an isolated injury in 50–75 % of cases. A partial rupture of this anterior talofibular ligament or an isolated capsular lesion is present in only 1 % of patients after a supination injury (Broström 1966; Prins 1978). With an increasing force, the calcaneofibular ligament is also ruptured. A rupture of both the anterior talofibular ligament and the calcaneofibular ligament occurs in 15–25 %. Isolated rupture of the calcaneofibular ligament happens in approximately 1 %, and injury to the posterior talofibular ligament is rare (Broström 1966; Karlsson and Andreasson 1992; Karlsson and Lansinger 1992).
Isolated ligament injuries of the deltoid ligament are infrequent. The frequency has been estimated to approximately 2.5 % of all ankle ligament injuries (Fallat et al. 1998). The injury mechanism is an excessive eversion, i.e., an outward rotation of the foot during simultaneous inward rotation of the tibia. This type of injury usually takes several weeks to heal and more often gives rise to chronic anteromedial pain rather than recurrent medial instability. Pain and swelling are present for a longer period of time than for a corresponding injury on the lateral side.
Injury of the ankle syndesmosis is often seen in soccer players after external rotation of the foot, in dancers after forced dorsiflexion of the foot, or in alpine skiers after combined external rotation, axial compression, and forced dorsiflexion (Fritschy 1989; Boytim et al. 1991; Taylor et al. 1992). When this injury is suspected, a complete radiographic examination of the lower leg should be performed to rule out a fracture of the proximal fibula. Disruption of the ankle syndesmosis is painful and often heals slowly, but residual disability with recurrent instability episodes is not frequent (Hopkinson et al. 1990; Xenos et al. 1995). A rupture of the anterior tibiofibular ligament alone does usually neither cause symptoms nor degenerative changes at long-term follow-up. It is concluded that this rupture of the anterior tibiofibular ligament does occur in 1–5 % of the patients after severe inversion trauma of the ankle (Hopkinson et al. 1990; Kiter and Bozkurt 2005). Physical examination cannot discriminate between an isolated lateral ankle ligament rupture and a lateral ankle ligament rupture accompanied by a (partial) syndesmotic ligament rupture. Treatment of the lateral ankle ligament rupture is sufficient for the natural healing of the concomitant syndesmotic ligament rupture (Taylor et al. 1992; Hopkinson et al. 1990; Xenos et al. 1995).
A supination trauma is associated with a distraction force on the lateral side and compression force on the medial side of the joint (Van Dijk et al. 1996a) (Fig. 9.2). Damage to the cartilage rim covering the anterior distal tibia, the anterior part of the medial malleolus, and the medial talar facet is known to occur in the majority of patients who sustain a supination trauma (Figs. 9.6 and 9.7). Depending on the degree of damage, a repair reaction with cartilage proliferation, scar tissue formation, calcification, and eventually development of osteophytes will follow. Additional damage due to recurrent instability or forced ankle movement, especially forced dorsiflexion, will enhance this process. Presence of osteophytes is not always associated with complaints. Asymptomatic ankle osteophytes have been reported in over 50 % of athletes. Arthroscopic removal of symptomatic osteophytes produces good or excellent results in over 90 % of cases (Tol et al. 2001; Van Dijk et al. 1997). Grading of the degenerative changes of the ankle joint in patients with chronic ankle instability is important for the judgment of the prognosis of ankle joint function in the longer term (Van Dijk et al. 1997).
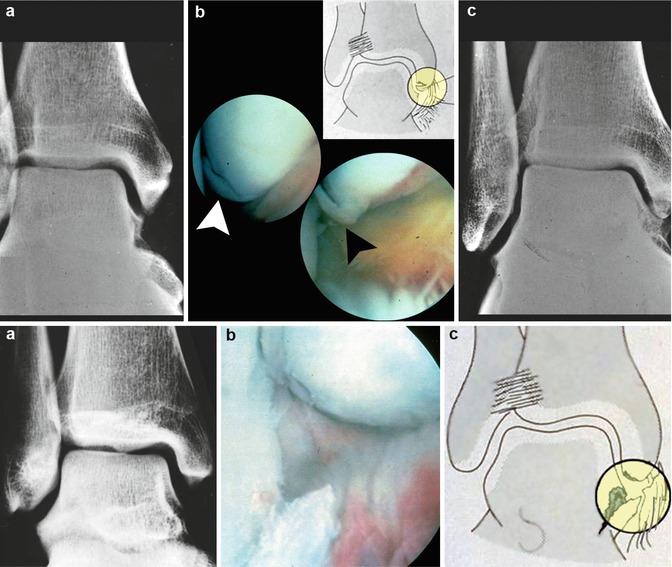
Figs. 9.6 and 9.7
Two patients out of a consecutive series of 30 patients underwent diagnostic arthroscopy five days after an acute supination trauma that resulted in a rupture of the lateral ligaments. In this group of 30 patients, a majority sustained damage to the cartilage of the tip of the medial malleolus and the anterior border of the medial malleolus and the opposite medial talar facet. Figure 9.6 shows a 32-year-old female patient 5 days after acute supination trauma which resulted in rupture of the lateral ligaments. The arthroscope is in the anterolateral portal looking over the medial edge of the talus towards the tip of the medial malleolus. The cartilage has been shifted off the subchondral bone of the tip of the medial malleolus like an eggshell (b). White and black arrowhead point at the cartilage lesion. The AP X-ray does not show a bony deformity (a). The X-ray 9 years later however shows osteophytic transformation of the tip of the medial malleolus and the medial talar facet (c). Figure 9.7 shows a 24-year-old female 6 days after an acute supination trauma of the left ankle. The arthroscopic view 6 days after the initial trauma shows the compression injury of the cartilage on the tip of the medial malleolus and a cartilage flap of the medial talar facet, in which the subchondral bone is exposed (b and c). The X-ray shows no abnormality (a)
9.2.1 Diagnosis of Acute Ligament Injuries
After a supination trauma, it is important to distinguish a simple distortion from an acute ankle ligament rupture since adequate treatment is associated with a better prognosis (Van Dijk et al. 1996a). Because of the poor reliability of physical examination after inversion trauma of the ankle, stress radiography, arthrography, MRI, and ultrasonography are often performed simultaneously (Friedrich et al. 1993). However, these methods are expensive and their reliability is debated. The reliability of physical examination can be enhanced when the investigation is repeated a few days after the trauma. The accuracy of physical examination has been determined in a series of 160 patients, who underwent arthrography, comparing physical examination within 48 h of the injury and 5 days after the injury. The specificity and sensitivity of delayed physical examination for the presence or absence of a lateral ankle ligament rupture were 84 and 96 %, respectively. The most important features of physical examination are swelling, hematoma discoloration, pain on palpation, and the anterior drawer test (Figs. 9.8 and 9.9). Physical examination is unreliable in the acute situation, since the anterior drawer test cannot be performed due to pain. A few days after the trauma, the swelling and pain have diminished and it becomes clear that the cause of swelling is edema or hematoma (Fig. 9.10). The pain on palpation has become more localized and the anterior drawer test can now be performed. If there is no pain on palpation over the anterior talofibular ligament, there is no acute lateral ligament rupture. Pain on palpation over the anterior talofibular ligament itself cannot distinguish between a rupture and a distortion. Pain on palpation in combination with a hematoma discoloration has a 90 % chance of acute lateral ligament rupture. A positive anterior drawer test has a sensitivity of 73 % and a specificity of 97 % (Figs. 9.9, 9.11, and 9.12). A positive anterior drawer test in combination with pain on palpation over the anterior talofibular ligament and hematoma discoloration has a sensitivity of 100 % and a specificity of 77 %. Delayed physical examination provides a diagnostic modality with a high sensitivity and specificity (Van Dijk 1994; Boytim et al. 1991; Taylor et al. 1992; Van Dijk et al. 1996b). It has been reported by the ISAKOS consensus meeting to be the method of choice (Van Dijk 2005).

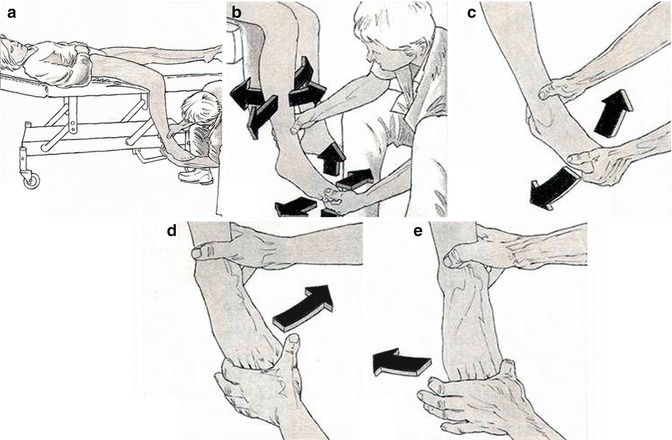

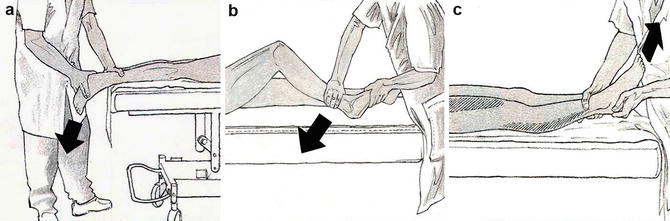
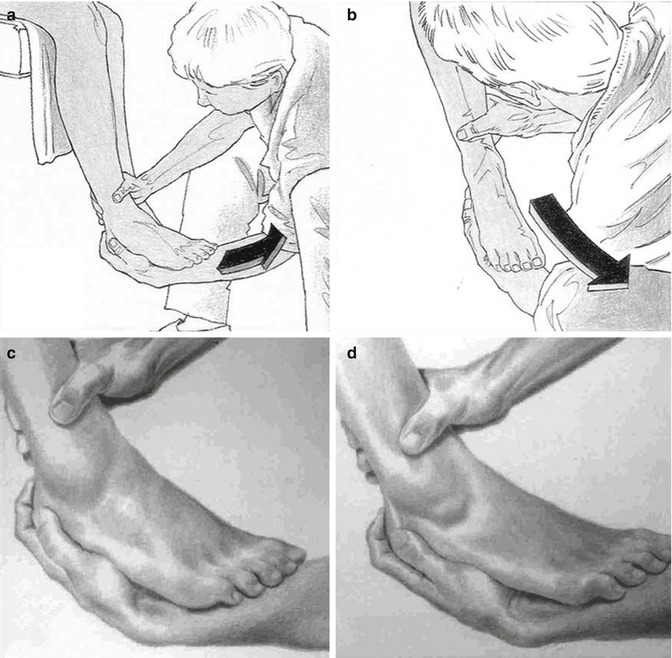

Fig. 9.8
Picture of patient a few hours after supination trauma which resulted in a rupture of the anterior talar fibular ligament (shown by arthrography). There is massive swelling on the lateral side. The location of tenderness on palpation is marked (red). There is a small area of tenderness on palpation on the medial side as well
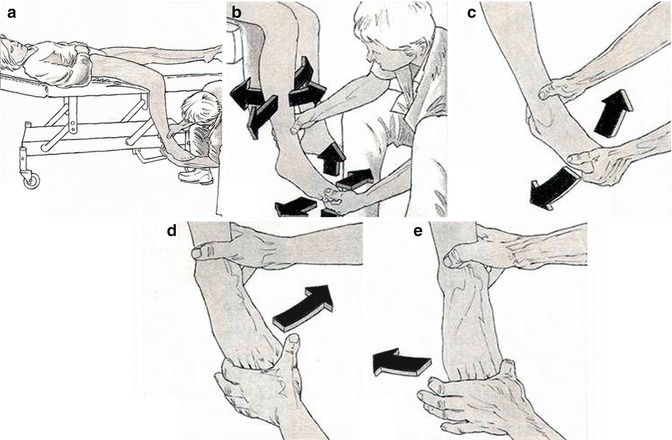
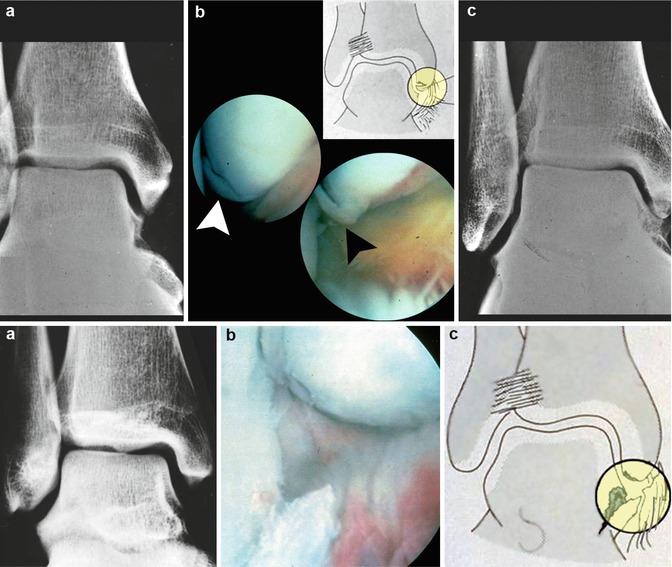
Fig. 9.9
Correct positioning of patient for performing anterior drawer test. (a) The patient is in the supine position. The upper leg supported by the table, the knee joint is flexed. The ankle joint is held in 10°–15° of plantar flexion. (b) When the patient is very apprehensive, relaxation is stimulated by grasping patients free hanging forefoot/toes loosening the ankle and foot by gentle manipulation in all directions. This includes exo- and endorotation of the hip and flexion and extension of the knee. (c) Gentle flexion and extension of the toes and ankle joint. (d) Gentle inversion and eversion (e) to check if the patient has relaxed all muscles that can control the anterior drawer

Fig. 9.10
The same patient from Fig. 9.8, 5 days after trauma. Hematoma discoloration on the lateral side. The pain on palpation is now localized on the insertion on the ATFL on the fibula and on the anterior joint capsule
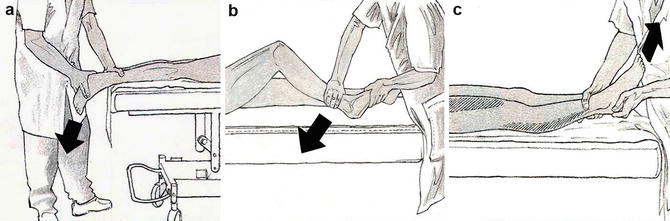
Fig. 9.11
Three methods of anterior drawer testing. These methods are not advised since the anterior drawer cannot be easily and directly visualized. In these three positions the patient cannot easily relax the lower leg muscles and thus withstand the anterior drawer. (a) The patient is in a prone position with the foot and ankle extending beyond the end of the table. With one hand the examiner presses the heel forward steadily. If the ATFL is ruptured, the talus moves further forward in the ankle mortise then on the uninjured side. (b) The patient is supine with hip and knee joint flexed. The heel rests against a support (table). The examiner holds the front part of the foot in a prone position with one hand, the other hand placed over the distal part of the lower leg. The leg is then rapidly and unexpectedly pushed backward. (c) The patient is supine with hip and knee joint extended. A backward force is applied to the lower leg, while the heel of the patient is supported. A forward pull on the heel/foot while holding the lower leg back is preferred by others
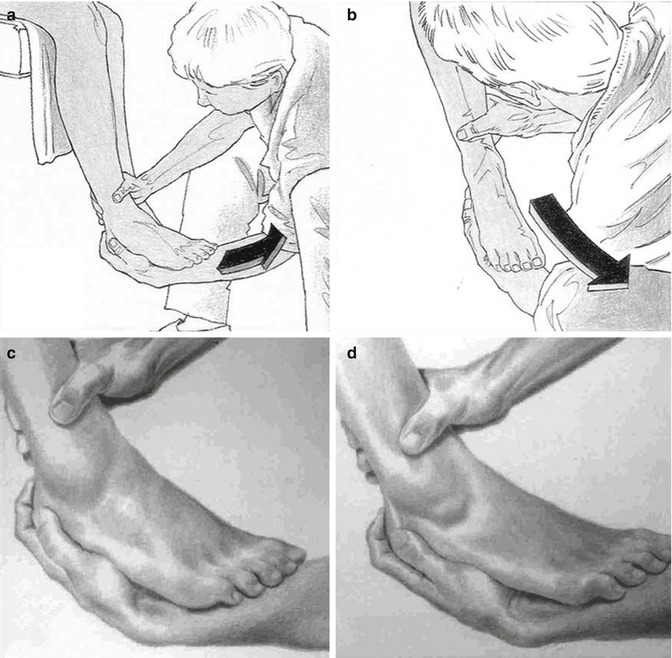
Fig. 9.12
(a) Anterior drawer test. Same test situation as shown in Fig. 9.6, but the patient instead of lying supine is sitting at the end of the table or at the side of a table. The knee is flexed to 90°. In this case the right ankle is tested. (b) Anterior drawer test. The talus (and with it the foot) rotates out of the ankle mortise anteriorly. The center of rotation is the intact deltoid ligament. The foot curves inward in the direction of the arrow. The examiner should “guide the foot” in this direction, while performing the test. (c, d) Anterior drawer test. The lower leg hangs downward (knee flexed). The heel is grasped and pulled forward. When a rupture of the ATFL is present, an indentation can be noticed just in front of the tip of the medial malleolus. The forward movement of the talus results in a negative pressure which draws the skin inward at the site of the ligament rupture. In case of a rupture of the ATFL, the talus typically moves forward, 1 cm in relation to the lower leg
9.2.2 Treatment of Acute Ligament Injuries
Repeated studies and recent systematic reviews have shown that simple sprains can safely be treated conservatively using functional treatment with a short period of rest, cooling (ice), compression, and elevation to reduce the edema (the RICE principle) during the first 1–3 days. Early weight bearing is encouraged. Active range of motion training is started after the acute phase treatment is completed, followed by neuromuscular coordination training using balance boards and peroneal strengthening exercises (Hamilton 1994; Kerkhoffs et al. 2003, 2005).
The ankle must be protected from new injuries during the healing phase by using an external support to control the range of motion. Both ankle tape and ankle braces, e.g., the air-stirrup, are easy to apply, versatile, and effective in stimulating the proprioceptive system. The results of functional treatment are satisfactory in the majority of cases, and most athletes are able to return to sporting activities within a few weeks (Kerkhoffs et al. 2003). It has been shown that costs are significantly lower and ankle function is significantly better following early functional brace treatment than after immobilization in a plaster cast (Karlsson and Andreasson 1992; Karlsson et al. 1991a; Kerkhoffs et al. 2002, 2001).
There is still a controversy as to whether ligament ruptures should be treated nonsurgically either by active functional treatment and early mobilization or by primary surgical. There are only a few prospective, randomized, and controlled studies in literature (Munk et al. 1995; Povacz et al. 1998). A recent meta-analysis concluded that surgical treatment leads to superior results in the short- and mid-term follow-up, in terms of giving-way and residual pain. Also, a large randomized prospective trial of surgical and functional treatment of lateral ankle ligament ruptures with 6–11 years of follow-up revealed that operative treatment leads to less residual pain and giving-way than functional treatment (Pijnenburg et al. 2000). Most studies show that the medium- and long-term results are satisfactory in the majority of these patients regardless of the primary choice of treatment, i.e., surgical repair, cast immobilization alone for 3–6 weeks, or functional treatment based on the principle of early immobilization (Kemler et al. 2011). In a prospective, randomized trial, comparing early mobilization with plaster cast immobilization, it was shown that these treatment modalities prevented late residual symptoms and persistent ankle instability equally well, but patients treated with early mobilization had significantly less pain at 3 weeks and were more likely to be back at work after 1 week (Karlsson et al. 1991a). Taken together, at least 80–90 % of patients with lateral ankle ligament ruptures will regain satisfactory functional stability after nonsurgical treatment.
Still, an unsolved problem is how the approximately 30–40 % of patients who will develop chronic instability in spite of adequate primary treatment and may need surgical reconstruction at a later stage can be identified. Neither the degree of ligament injury nor the degree of radiographic laxity as measured by stress radiographs is reliable predictors (Karlsson 1989). Therefore, this question still remains unanswered.
9.3 Ankle Joint Instability
Functional instability is the most common residual disability after an acute, lateral ligament rupture. It is a description of the subjective symptoms of the patient, with repeated giving-way, combined with pain. Laxity or mechanical instability refers to an objective measurement with standardized stress radiographs or clinical measurement of anterior drawer sign (Karlsson et al. 1991a).
Functional instability is a complex syndrome, in which mechanical, neurological, muscular, and constitutional factors interact. The etiological factors are not exactly known and in several cases there is a combination of factors (De Vries et al. 2010). Elongation of the ruptured ligaments, i.e., increased laxity, proprioceptive deficit, peroneal muscle weakness, and subtalar instability, are all documented etiological factors of functional instability, either alone or in combination. In some studies a correlation between functional instability and increased laxity using standardized stress radiographs has been shown (Karlsson 1989, 1991b). Although these radiographic stress tests may be useful, the reliability of these tests is rather low and there is no definite correlation between functional instability and increased laxity (Konradsen et al. 1991; Karlsson and Andreasson 1992; Karlsson et al. 1992; Kerkhoffs et al. 2003, 2005).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








