I. ANKLE SPRAINS. The approach to ankle sprains should distinguish between the acute and chronic ankle sprains. The most common ankle sprain consists of an inversion injury of the foot with some degree of plantar flexion. Overall, the period of recovery is relatively short and uneventful. A more significant injury with a completely different period of recovery is the injury while the foot is in eversion, the so-called high-ankle sprain (ankle syndesmosis sprain). It accounts for 1% to 15% of the total ankle sprains.1 Therefore, the first issue when approaching a patient with an ankle sprain should be directed to identifying the mechanism of injury. Given the possibility of fractures, it is often recommended to obtain the history and do a brief examination using only palpation, and, if suspicion for a fracture is present, obtain X-rays prior to extensive physical examination techniques.
A. Acute presentation
- Inversion injuries. With inversion ligamentous injuries, there is tearing of the lateral ligaments from front to back. Thus, the anterior talofibular ligament (ATFL) is the most commonly injured ligament followed by the calcaneofibular ligament and, in very rare instances, the posterior talofibular ligament.
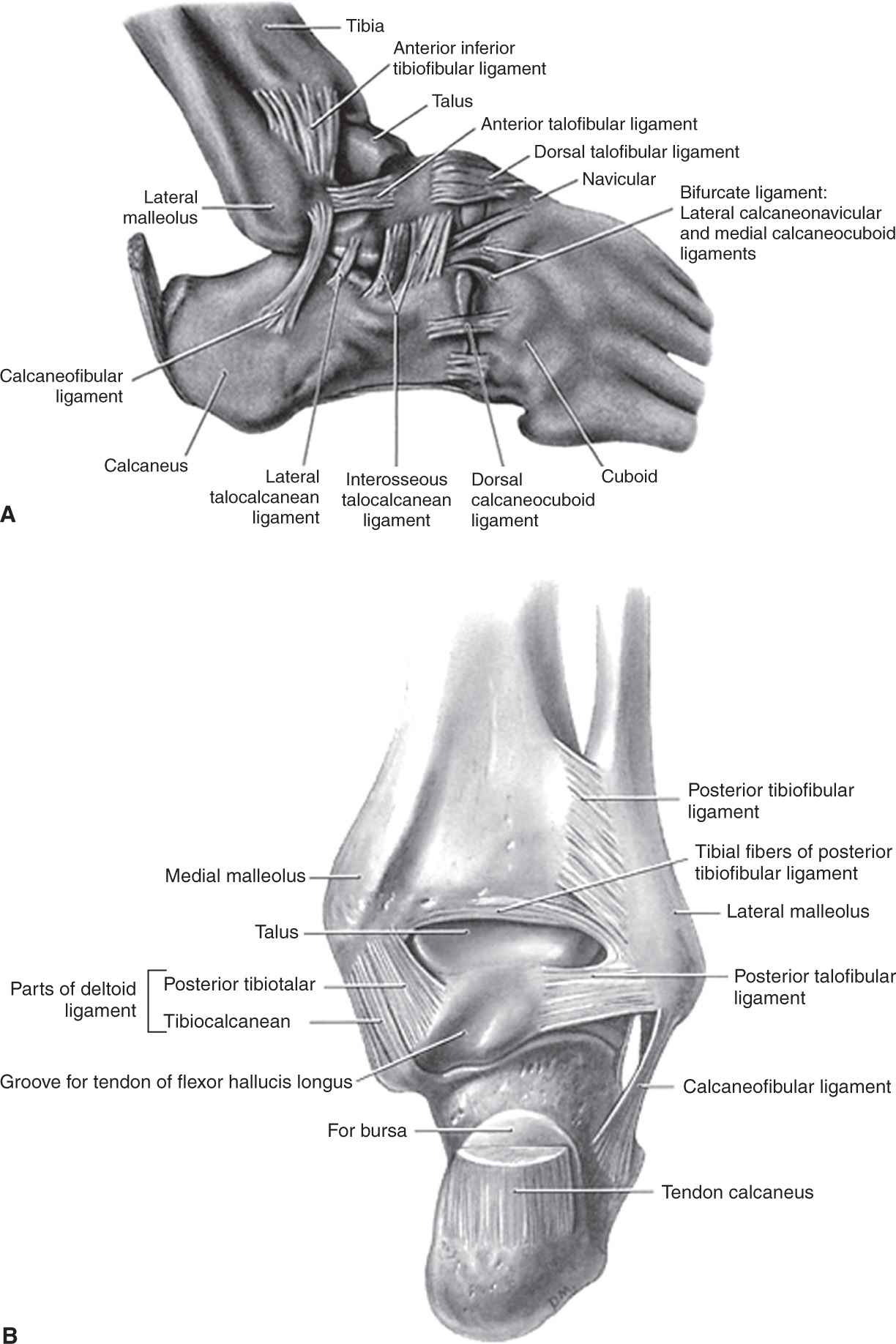
Fig. 27-1 shows the anatomic location of the ligaments. Fractures can occur with simple inversion injuries. The most common sites are the distal fibula and the base of the fifth metatarsal. More rarely, the lateral process of the talus and the anterior process of the calcaneus may fracture as well.
Figure 27-1. Anatomic description of the most significant ligaments and bones of the ankle and midfoot area.
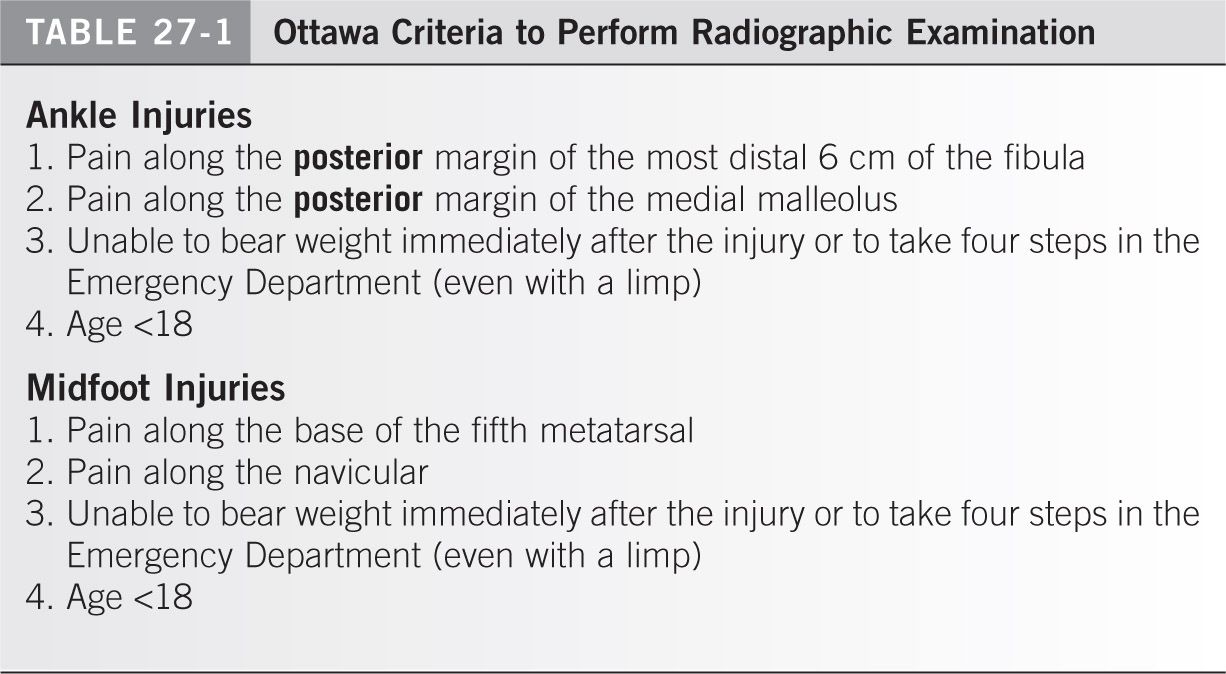
a. Examination. Palpation of the bones around the ankle is the key to examining ankle injuries. Special attention should be drawn to the distal fibula, distal tibia, and the base of the fifth metatarsal as per the Ottawa criteria (Table 27-1). In more severe fractures, also palpate the proximal fibula as this can be broken (Maissoneuve fracture). All ankle ligaments should be palpated looking for tenderness. In the acute setting, pain is quite limiting; therefore, it is very difficult to stress the ankle joint or obtain ankle stress radiographs to document the degree of instability. In the absence of fracture, soft-tissue swelling and pain will dictate the treatment.
b. Radiographic imaging. The need for X-rays can be guided by consideration of the Ottawa ankle rules (Table 27-1). It is important to note that the rules do not apply to a pediatric population with open growth plates (to be safe, it is recommended to X-ray those under age 18). Although not specifically listed, we recommend strong consideration to obtain X-rays on people over the age of 50, especially women over the age of 50 due to lower bone mass and subsequent higher fracture rates. X-rays should include anteroposterior (AP), lateral, and mortise views of the ankle.
c. Treatment. If there is no medial tenderness, the ankle joint should be considered a stable joint. The traditional principles of rest, minimal immobilization, compression, elevation, and icing should be applied followed by a functional return to activities while protected with any of the commercially available ankle braces until the pain allows proper muscle contraction of the dynamic stabilizers of the ankle (peroneal and deep compartment muscles of the lower leg). In rare occasions, owing to pain with weight bearing, the patient will have to be protected with crutches for a period.
If there is medial or anterior capsule tenderness, the possibility of developing long-term ankle instability may be higher, and closer examination of the ankle mortise for talar dome injuries is warranted. If suspected, a period of immobilization in a walking cast or boot could be as long as 6 to 8 weeks until the medial and anterior tenderness disappear. At that time, it can be treated as a stable injury depending on the remaining discomfort within the ankle joint.
2. Eversion injuries
a. Examination. The examination will show some tenderness along the most anterior and distal aspects of the syndesmosis of the ankle. Some tenderness along the lateral ligament complex may be present although to a much lesser degree than with true inversion ankle sprain. Any degree of external rotation, which stresses the ankle mortise, will increase or reproduce the pain. The external rotation can be applied directly by the examiner holding the lower leg with one hand and torquing on the foot with the opposite hand while keeping the ankle in a neutral position, so the talus is locked in the ankle mortise. If a fracture has been ruled out, a “squeeze test” (using both hands to push the mid-fibula and tibia together, noting pain distal to the area of compression) can be performed to assess syndesmotic injuries. If the patient can tolerate weight bearing, a more sensitive test for a syndesmosis injury consists of standing on the injured leg and applying an external rotation force to the ankle with an internal turn of the pelvis with the knee fully extended. If the patient can stand and perform some degree of external rotation, the suspicion for an unstable mortise should be low. If there is any tenderness in the proximal lower leg, full length tibia and fibula radiographs should be obtained to rule out a proximal fibula fracture (Maissonneuve fracture) or an unstable syndesmosis. The best projection to assess ankle syndesmosis instability is the mortise view of the ankle. This projection is taken as an AP view with 30° of internal rotation (when both malleolus are equidistant from the X-ray beam). A noncompetent syndesmosis is defined as the one that presents on an AP view of the ankle more than 6 mm of clear space between the tibia and the fibula measured at 10 mm proximal from the joint line2 (Fig. 27-2). When it comes to X-ray measurements, the clear space in between the tibia and the fibula has been shown to be more reliable and less subjective to rotation than the overlap in between the tibia and fibula (<5 mm). If the syndesmosis appears intact on a static radiograph, but suspicion for syndesmotic instability remains high, consider stressing the ankle (ideally under fluoroscopic dynamic examination) while applying external rotation to the foot for final assessment. The patient may need to be either sedated or injected with local anesthetic along the syndesmosis prior to its evaluation. A total of 5 to 15 cc of lidocaine 1% with epinephrine should suffice to anesthetize the syndesmosis. The injection is performed using a 25G or 22G needle along the anterior aspect of the syndesmosis, starting immediately proximal to the joint line level and always “walking” along the lateral cortex of the tibia from distal to proximal. Special attention has to be paid to not angle the needle too posteriorly, never posterior to the plane of the fibula, to avoid damage into vital structures of the posterior compartment of the leg.
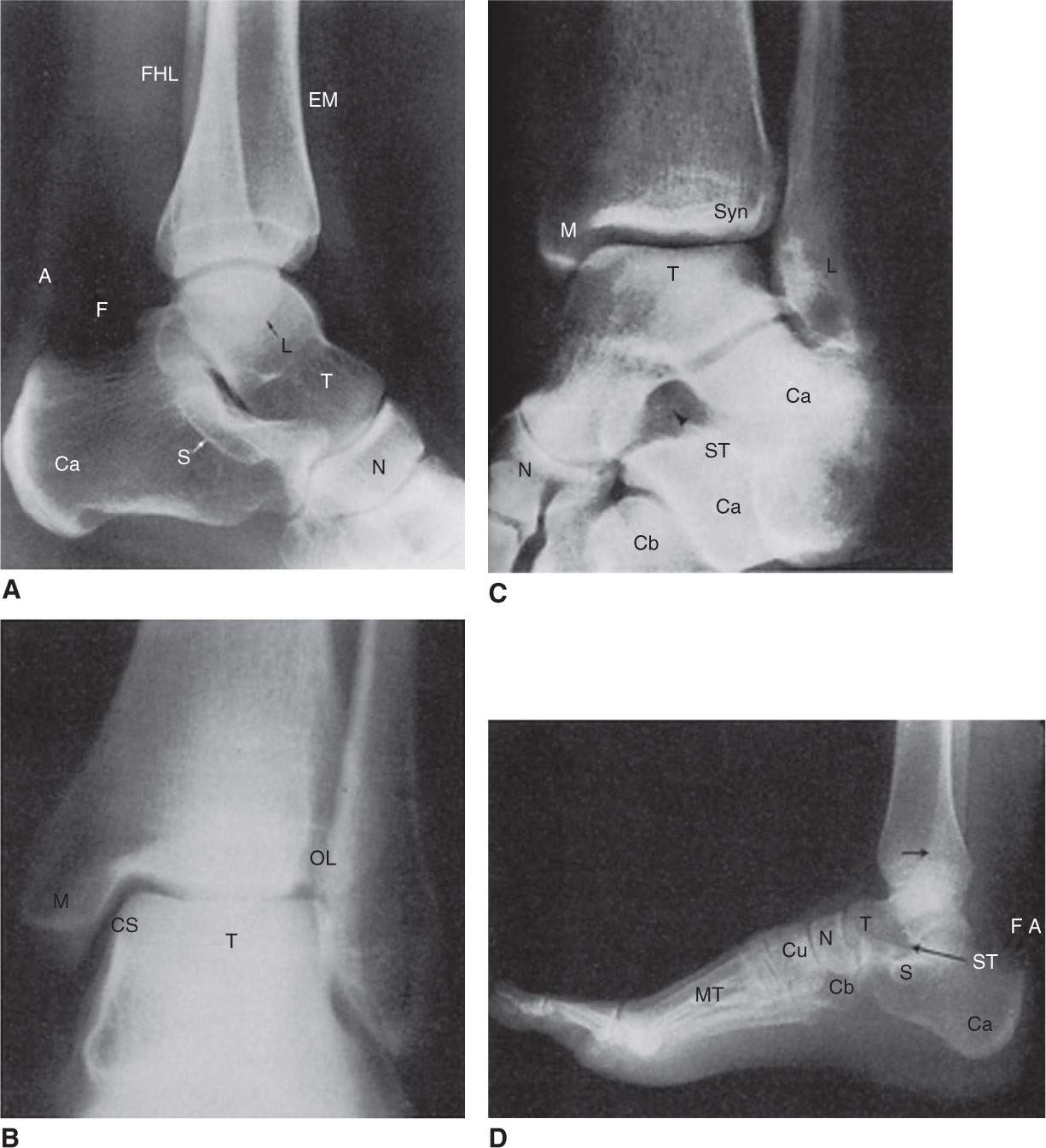
Figure 27-2. Radiographic appearance of the most common bony landmarks of the ankle and foot. A: Medial view of ankle region. B: Anterior view of ankle. C: Mortise view of ankle region. D: Lateral view of foot. M, medial malleolus; L, lateral malleolus; T, talus; Ca, calcaneus; S, susten-taculum tali; N, navicular; Cu, cuneiforms; Cb, cuboid; Mt, metatarsal; ST, sinus tarsi; A, Achilles tendon; F, fat; arrowhead, superimposed tibia, and fibula; Syn, Syndesmosis; FHL, flexor hallucis longus; EM, extensor muscles; CS, tibiofibular clear space; OL, tibiofibular overlap.
b. Treatment. If the syndesmosis is stable and in the absence of fractures, the patient should be immobilized in a walking cast or boot for 6 to 8 weeks followed by a functional return to activities. If the syndesmosis is unstable or in the presence of a proximal fibula fracture, the patient will require fixation of the syndesmosis followed by immobilization for 6 to 8 weeks. The fixation method is variable, with recently gaining some popularity devices without the need for removal or second surgeries (unlike more traditional fixation with screws). A residual wide syndesmosis because of a misdiagnosis or improper treatment is a devastating sequelae that will lead to posttraumatic osteoarthritis of the ankle joint within 1 to 2 years.
B. Subacute–chronic presentation
- Inversion injuries. The patient presents with some residual discomfort in areas where there may still be some healing taking place or where an injury has been missed. The physician has to rule out any residual instability, reported to be present in 20% to 40% of ankle sprains, or a chondral injury of the talus, present in 6.5% of ankle sprains.3 If the patient continues to report instability after a period of physical therapy, one may consider stress views of the ankle. Although they are not absolutely necessary to confirm the diagnosis, they help to document the degree of instability. The patient may require having the ankle anesthesized to allow a reliable radiographic evaluation. A total of 5 cc of lidocaine 2% with epinephrine should be enough to anesthetize the ankle joint. The injection is performed with a 25G or 22G needle along the most medial border of the ankle joint immediately distal to the medial shoulder of the tibial plafond and medial to the anterior tibialis tendon. The needle has to be angled at 45° from the coronal plane (see Chapter 30). The ankle can also be approached through the lateral aspect over the “soft spot,” which is defined as the junction of the tibia and fibula at the level of the joint line. However, the chances of damaging the dorsal cutaneous branch from the superficial peroneal nerve are not low. The best chance to identify the nerve branch is with gentle palpation of the skin, looking for a cord-like structure, when the ankle and fourth toe are forced into plantar flexion.
The stress views are obtained with a lateral radiograph while the foot is pulled forward (an anterior drawer test) in slight plantar flexion. The most commonly injured ligament, the ATFL, is stressed during this maneuver. A 10-mm difference of anterior displacement between the stress view and the resting view or a 3-mm difference of anterior displacement compared with the stressed opposite side is indicative of ankle instability. Treatment options for chronic instability include a formal physiotherapy program and, if that fails, the next reasonable step is a surgical repair/reconstruction of the lateral ligament complex of the ankle. In the absence of an obvious chondral injury of the talus on plain X-rays, a magnetic resonance imaging (MRI) scan is necessary to rule it out. A symptomatic chondral injury most likely will require some surgical treatment (i.e., arthroscopic debridement ± subchondral drilling) to improve the symptoms.
2. Eversion injuries. The most common reason to present with residual pain after a syndesmosis sprain will be some degree of remaining instability. A careful and detailed evaluation of the patient has to be performed as surgical fixation of the syndesmosis will be the most likely treatment recommendation.
II. ANKLE FRACTURES
A. Classification. Ankle fractures are intraarticular injuries, and accurate reduction as well as maintenance of the reduction is required for a satisfactory long-term result. To achieve reduction by closed manipulation, it is necessary to know the direction of the forces producing the fractures. It must be emphasized that fractures about the ankle usually are not isolated injuries and more likely than not will have associated ligamentous injuries. Ankle fractures may be classified by the Lauge-Hansen scheme (Fig. 27-3). This classification is useful because of the method used for its description. The first term makes reference to the position of the foot at the time of injury and the second term to the direction of the force applied to produce the fracture. That information is extremely valuable in planning closed reduction maneuvers.
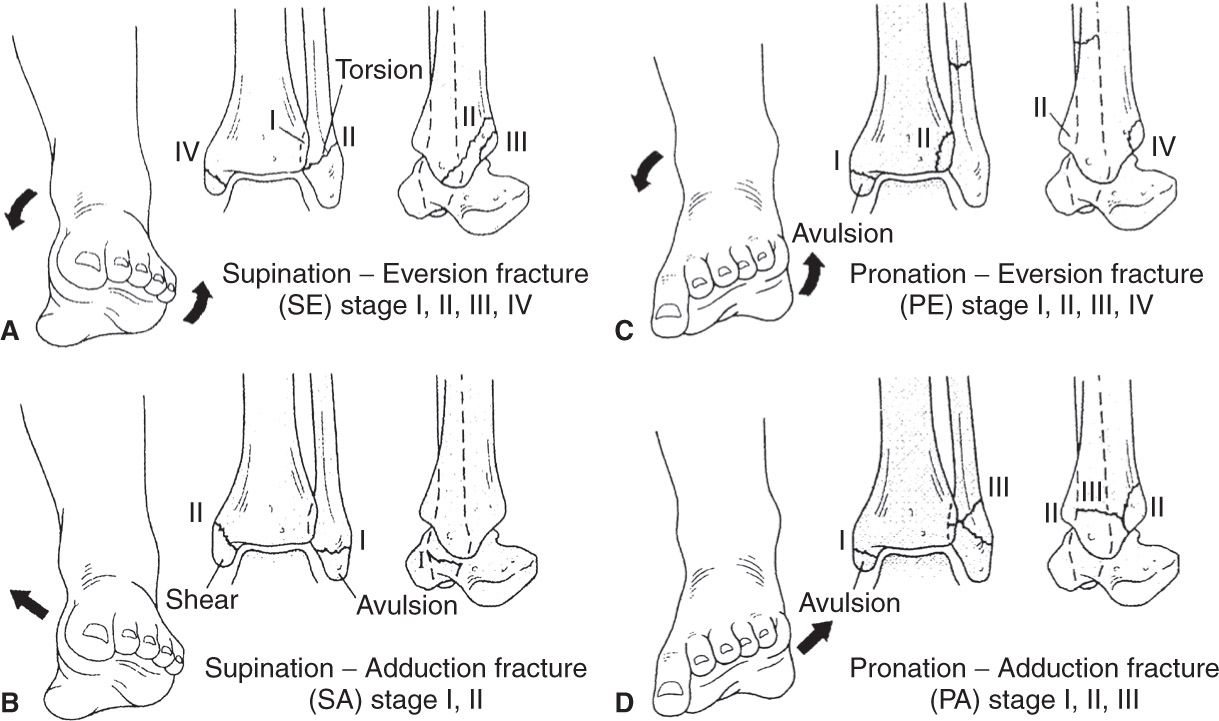
Figure 27-3. The Lauge-Hansen classification of ankle fractures. A:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree