Ankle Fractures: Open Reduction Internal Fixation
David J. Hak
Mark A. Lee
Indications/Contraindications
Ankle fractures are among the most common orthopedic injuries. Nondisplaced fractures can almost always be successfully treated nonoperatively with close follow-up. Most displaced bimalleolar fractures benefit from operative reduction and fixation if no surgical contraindications exist.
Certain displaced-ankle fractures can be treated with closed reduction, and if successful, carefully followed to union with nonoperative treatment. Isolated, distal, fibula fractures without mortise widening or talar shift can usually be successfully managed nonoperatively if the fibular displacement is less than 2 mm. These patients must be differentiated from individuals who also have an obvious or occult injury to the medial side of the ankle. While the decision for operative versus nonoperative treatment is frequently clear, for a group of patients, the treatment decision is more difficult; for these patients, reduction may be borderline acceptable or follow-up x-rays suggest some loss of reduction.
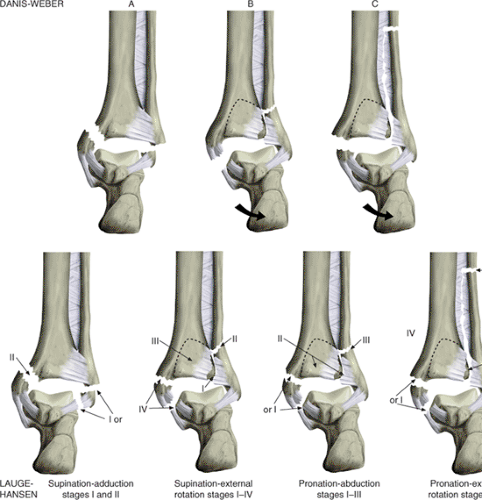
Two classification systems of ankle fractures are commonly used. Lauge-Hansen described a classification based on the foot position (supination or pronation) at the time of injury and the direction of the injury force (external rotation, adduction, or abduction) on the foot (Fig. 33.1). The Danis-Weber classification is based on the location of the fibula fracture with respect to the ankle joint. In Danis-Weber injuries, the fibula fracture is distal to the ankle joint and is usually the equivalent to Lauge-Hansen supination-adduction injuries. In Danis-Weber B injuries, the fibula fracture is at the level of the ankle joint and can be either a supination–external rotation or pronation-abduction injury. Type C Danis-Weber fractures are characterized by a fibula fracture proximal to the ankle joint and are usually the equivalent of the Lauge-Hansen pronation–external rotation injury.
Supination–external rotation injuries are thought to be the most common fracture pattern. In this injury, the supinated foot is subjected to an external rotation force that may cause a varying degree of soft-tissue and bony damage. The first structure to be injured is the anterior tibiofibular ligament (stage I). As the external rotation force continues, the
fibula is fractured (stage II). Further force results in rupture of the posterior tibiofibular ligament or a fracture of the posterior malleolus (stage III). Finally, the deltoid ligament is ruptured or the medial malleolus is fractured (stage IV). Because of their clinical significance, stage II injuries must be differentiated from stage IV supination–external rotation injuries. Stage II injuries can be managed nonoperatively because the deltoid ligament is intact, stabilizing the talus in the mortise. However, in stage IV injuries, the ankle is unstable, and surgical management is usually recommended (1).
fibula is fractured (stage II). Further force results in rupture of the posterior tibiofibular ligament or a fracture of the posterior malleolus (stage III). Finally, the deltoid ligament is ruptured or the medial malleolus is fractured (stage IV). Because of their clinical significance, stage II injuries must be differentiated from stage IV supination–external rotation injuries. Stage II injuries can be managed nonoperatively because the deltoid ligament is intact, stabilizing the talus in the mortise. However, in stage IV injuries, the ankle is unstable, and surgical management is usually recommended (1).
Traditionally, medial ecchymosis and tenderness when the ankle is palpated have been used as clinical indicators for occult injury to the medial deltoid ligament. Recent studies have shown that these traditional signs are not sensitive for predicting deltoid ligament incompetence (1,2). Stress radiographs should routinely be obtained in patients with isolated fibula fractures that are classified as supination–external rotation injuries (Danis-Weber type B) so the physician can identify occult injury to the deltoid ligament. Several different methods for obtaining stress radiographs have been described and include the use of gravity, valgus stress, or external rotation (2,3).
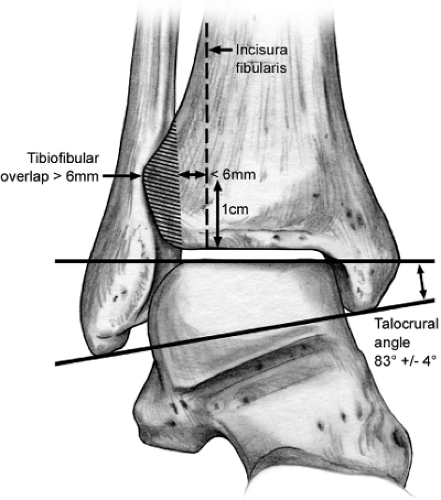
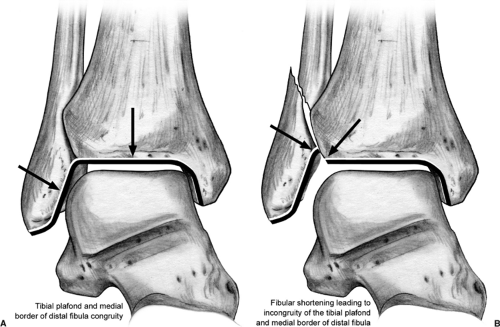
We prefer a careful evaluation of high-quality plain x-rays in the absence of plaster, which may obscure important findings. Occasionally, contralateral radiographs are useful to evaluate unusual abnormalities. The physician must understand the normal radiographic landmarks and relationship of the fibula with the distal tibia. Equal medial, lateral, and superior joint space should be seen surrounding the talus on the mortise view. The position of the distal fibula with respect to the incisura should be carefully evaluated. This is measured 1 cm proximal to the tibial plafond. Specific measurements may vary depending on the ankle rotation and angle of the x-ray beam. The distance between the medial border of the fibula and the incisura should be less than 6 mm on both the anteroposterior (AP) and mortise view. On the AP view, the fibula should overlap the tibia by 6 mm, or 42 % of the fibular width, and there should be at least 1 mm of overlap between the fibula and tibia on the mortise view. Finally, the length of the fibula is assessed by evaluating the talocrural angle, which on average should measure 83 ±4 degrees and can be compared with the contralateral ankle (Fig. 33.2). In addition, fibular shortening will lead to incongruity in a line drawn along the tibial plafond and the medial border of the distal fibula (Fig. 33.3).
One of the major goals of ankle fracture management, whether operative or nonoperative, is to maintain anatomic reduction of the tibiotalar joint. Lateral displacement of the talus will reduce ankle joint contact, resulting in joint-contact stress alterations that may predispose the patient to posttraumatic osteoarthritis (4,5,6).
Closed reduction and splinting are the first step in fracture management. The majority of rotational ankle fractures will require little more than longitudinal traction and internal rotation reduction to be achieved. A well-padded, posterior, plaster splint with the ankle at neutral dorsiflexion will provide comfort and immobilization and allow for soft-tissue swelling. In general, immediate circumferential casting should be avoided, even if this is eventually chosen as the definitive treatment method, as ongoing swelling can lead to dangerous constriction and exacerbation of the soft-tissue injury. Edema control with judicious elevation is a well-accepted approach to early management if compromised vascular inflow is not an issue. Cryotherapy may reduce swelling and may have analgesic benefit. More recently, intermittent compression devices have been utilized to help control swelling both preoperatively and postoperatively (7,8).
Occasionally, when managing fractures with significant soft-tissue injuries or those with large, posterior, malleolar fractures that cause persistent talar subluxation, the surgeon may find that temporary external fixation is required. External fixation provides fracture and soft-tissue stability, allows for free access and easy evaluation of the soft tissues, and optimizes patient mobilization.
Many ankle fractures requiring open reduction and internal fixation can be addressed with immediate surgery. However if soft-tissue swelling is a concern, the operation is delayed and the limb is immobilized and elevated. Examination of the skin should be performed preoperatively
to insure that the soft tissues can safely permit operative treatment. This requires removal of the splint or cast prior to the induction of anesthesia. The “wrinkle sign” is often used to assess the readiness of soft tissues for surgical intervention. The ankle is dorsiflexed to the neutral position and the anterior ankle skin is observed for the presence of wrinkles. Absence of wrinkles suggests excessive soft-tissue swelling and edema.
to insure that the soft tissues can safely permit operative treatment. This requires removal of the splint or cast prior to the induction of anesthesia. The “wrinkle sign” is often used to assess the readiness of soft tissues for surgical intervention. The ankle is dorsiflexed to the neutral position and the anterior ankle skin is observed for the presence of wrinkles. Absence of wrinkles suggests excessive soft-tissue swelling and edema.
Preoperative Planning
While open reduction and internal fixation (ORIF) of most ankle fractures is straightforward, care should be exercised to avoid unexpected findings. A careful review of high-quality plain radiographs (without obscuring plaster) should be performed. A preoperative plan or surgical tactic, while often neglected for this “simple” fracture, may provide mental preparation and avoid unnecessary mistakes. Forging ahead, assuming the case is a simple straightforward ankle fracture, can lead to suboptimal outcomes when unusual fracture variations are encountered.
Surgery
Patient Positioning
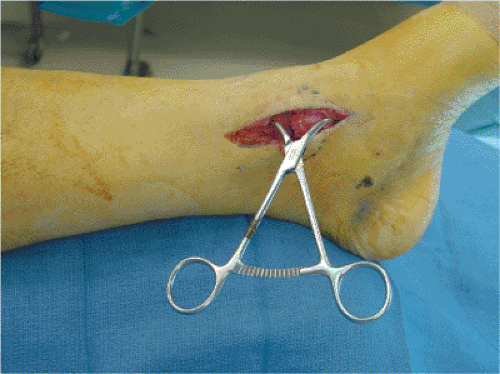
Patients are generally positioned supine, and a general or spinal anesthetic is administered. Prophylactic intravenous antibiotics are administered prior to surgery. A first-generation cephalosporin is used unless there is an allergic contraindication, in which case an alternative antibiotic is chosen. A towel roll is placed beneath the ipsilateral buttock to provide easier access to the fibula (Fig. 33.4). As is routine, a pneumatic tourniquet is applied to the upper thigh. The leg is sterilely prepped. A sterile sheet is then placed beneath the leg to prevent inadvertent contamination of surgical gowns during the draping process. A stockinette is applied to the leg, and the leg is draped free. The toes are sealed with a plastic adhesive drape and the stockinette is removed to the midcalf.
Prone positioning may occasionally be indicated for trimalleolar ankle fractures with a large, displaced, posterior, malleolar fragment that will be fixed through a posterolateral approach. Reduction and fixation of the medial malleolus in the prone position may be easiest performed after the knee is flexed.
Technique
Bony landmarks are palpated and marked. The location of the fracture can also be marked based on palpation and radiographic review. We generally perform surgery under tourniquet control to minimize blood loss, to maximize visualization, and to speed the surgical procedure. After confirming that preoperative prophylactic antibiotics have been administered, we exsanguinate the extremity with an elastic (Esmarch) bandage and inflate the tourniquet to the appropriate level.
In bimalleolar fractures, the surgeon’s preference dictates whether the medial malleolus or the fibula is fixed first. In cases of osteopenia, we prefer to fix the medial malleolus first because it may aid the subsequent reduction of the fibula. Care must be exercised when using reduction clamps on osteopenic bone. Excessive pressure with reduction clamps may easily cause iatrogenic comminution of the fibula. In addition, the ankle joint can usually be visualized through the medial malleolar fracture site in most circumstances. This allows inspection of the articular surface and removal of any intra-articular debris. While joint inspection and irrigation can be performed either before or after fixation of the fibula, we often do this prior to rigid fixation of the fibula.
Medial Malleolar Fixation
Our preferred medial incision is straight and aligned with the long axis of the tibia. This incision should also be placed slightly anterior to the midcoronal axis to allow inspection of the anterior aspect of the ankle joint. Other surgeons prefer a slightly angled incision, but too much, distal, anterior angulation may make difficult the access to the screw insertion site. The saphenous vein and its accompanying saphenous nerve branches should be preserved whenever possible (Fig. 33.5).
Adequate exposure is required to ensure an anatomic reduction. This can best be confirmed by visualizing the anterior aspect of the fracture. Because of the orientation of the fracture plane, anterior or posterior malreduction may not always be appreciated when looking at the lateral surface.
Distal retraction of the medial malleolus allows irrigation and thorough inspection of the articular surface of the tibia and talus (Fig. 33.6). Any osteocartilaginous debris should be removed. Articular damage to either the tibia or talus should be noted in the operative report.
Approximately 2 mm of periosteum is excised along the edges of the fracture. A 2.5-mm drill is used to perforate the medial tibial cortex to allow anchorage of a bone tenaculum. A small, pointed, bone tenaculum can be placed on the medial malleolar-fracture fragment from anterior to posterior and used to guide the reduction. A second small or large, pointed, bone tenaculum is then used to achieve compression of the reduction. One tine is placed in the tibial metaphyseal drill hole and the other is placed around the distal aspect of the
medial malleolus. (Fig. 33.7).
medial malleolus. (Fig. 33.7).
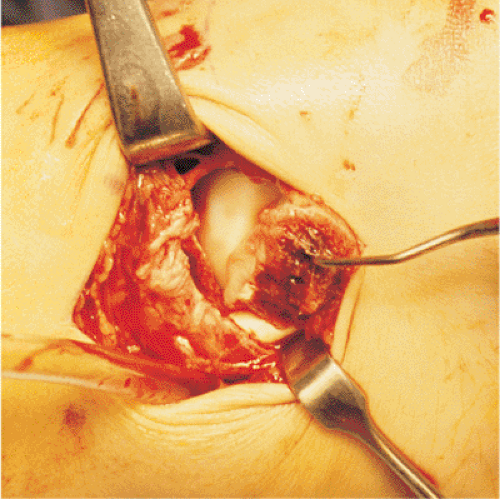 Figure 33.6. Retraction of the medial malleolar fragment distally allows inspection and irrigation of the ankle joint. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree