Arthroscopic Ankle Arthrodesis
Keywords
• Ankle • Arthrodesis • Arthroscopy • Fusion • Arthritis
Despite the increasing popularity of total ankle replacement (TAR), ankle arthrodesis remains the gold standard for the treatment of end-stage ankle arthritis.1,2 Historically, open techniques have been used for ankle arthrodesis. Many variations and techniques, including transfibular, anterior, and medial approaches and miniarthrotomy, have been described.3–17 Inherent disadvantages to these open techniques include postoperative pain, delayed union or nonunion, wound complications, shortening, prolonged healing times, and prolonged hospital stays.18–20
Arthroscopic ankle arthrodesis provides the foot and ankle surgeon with an alternative to the traditional open techniques. Arthroscopic ankle arthrodesis has demonstrated faster union rates, decreased complications, reduced postoperative pain, and shorter hospital stays.3,20–29 Although once considered technically difficult, advancements in techniques and instrumentation have reduced the learning curve once encountered with the arthroscopic technique.
Schneider30 first reported arthroscopic ankle arthrodesis in 1983, and described faster time to union, earlier mobilization, and reduced patient morbidity. Recent studies have demonstrated similar results, with faster union rates comparable with those using current open techniques, fewer complications, and shorter hospital stays.3,21–23,29 This article discusses the indications, technique, and complications associated with arthroscopic ankle arthrodesis.
Indications/contraindications
Arthroscopic ankle arthrodesis may be indicated in patients with end-stage arthritis caused by rheumatoid arthritis, posttraumatic arthritis, arthrogryphosis, septic arthritis, inflammatory arthritis, avascular necrosis of the talus, idiopathic osteoarthritis, and chronic ankle instability. Posttraumatic arthritis is the most frequently encountered cause.21
The primary indication for ankle arthrodesis is persistent pain in the arthritic ankle joint that has not responded to conservative treatments, including analgesics, nonsteroidal antiinflammatory drugs, corticosteroid injections, and orthoses or bracing for several months.3,22,28 Although not currently approved by the US Food and Drug Administration for the ankle joint, hyaluronase injections may also be used before proceeding with arthrodesis or replacement.
Limitations of arthroscopic ankle arthrodesis are typically related to deformity or malalignment about the ankle joint. Various studies have indicated that malalignment greater than 10° to 15° makes reduction of the ankle joint and deformity difficult.23,31 Ferkel and Hewitt27 indicated that patients with significant ankle deformity, either significant varus or valgus, are better suited for an open technique and those who require arthrodesis in situ are better suited for the arthroscopic technique. Tang and colleagues32 stated that arthroscopy is not advised when a large ankle deformity is present. A study by Gougoulias and colleagues26 showed that patients with marked deformity of greater than 10° to 15° of varus or valgus can be treated effectively using arthroscopy, depending on surgeon experience.
In addition to significant malalignment, Collman and colleagues22 noted that contraindications of arthroscopic ankle arthrodesis include excessive bone loss, neuropathic joints, active infections, and poor bone stock. Avascular necrosis of the talus may also be a contraindication.
Surgical technique
The ankle is insufflated with approximately 20 mL of normal sterile saline using an 18-gauge needle. Standard anteromedial and anterolateral portals are used. A 2.7-mm 30° arthroscope is then introduced into the ankle joint. The author prefers to use large joint power shavers and burrs while using a 2.7-mm arthroscope rather than the 4.0-mm arthroscope. A noninvasive ankle distractor is applied to the ankle to allow for complete visualization from anterior to posterior, as well as both the medial and lateral gutters (Fig. 1).

Fig. 1 Noninvasive ankle distractor is used for joint visualization.
(From Lee MS, Millward DM. Arthroscopic ankle arthrodesis. Clin Podiatr Med Surg 2009;26:274; with permission.)
A 3.85-mm full-radius incisor blade is used to aggressively debride the anterior joint of any hypertrophic synovium, fibrosis, or loose bodies. In some cases, aggressive resection of anterior tibiotalar osteophytes is required for proper joint visualization. A curette is inserted to aggressively remove any remaining articular cartilage (Fig. 2). A grasping forceps or resector may be used to remove the cartilage fragments that typically collect in the posterior aspect of the joint (Fig. 3). A 4.0-mm full-radius burr or 4.85-mm acromion burr is then used to resect the subchondral plate (Fig. 4). A curved osteotome is then used to fish scale the subchondral plates of both the tibia and talus (Fig. 5). Ideally, healthy bleeding bone is visualized throughout the tibiotalar articulation (Fig. 6). The joint is then irrigated, and all loose bodies or fragments are evacuated.
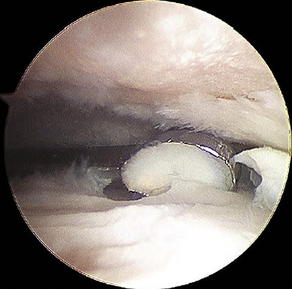
Fig. 2 Curettage of the remaining articular surface.
(From Lee MS, Millward DM. Arthroscopic ankle arthrodesis. Clin Podiatr Med Surg 2009;26:275; with permission.)

Fig. 3 Removal of the cartilage fragments after aggressive curettage.
(From Lee MS, Millward DM. Arthroscopic ankle arthrodesis. Clin Podiatr Med Surg 2009;26:276; with permission.)
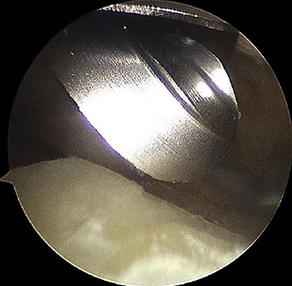
Fig. 4 Full-radius burr is used to resect the subchondral plate.
(From Lee MS, Millward DM. Arthroscopic ankle arthrodesis. Clin Podiatr Med Surg 2009;26:276; with permission.)

Fig. 5 Fish scaling the talus with a curved osteotome in preparation for arthrodesis.
(From Lee MS, Millward DM. Arthroscopic ankle arthrodesis. Clin Podiatr Med Surg 2009;26:277; with permission.)

Fig. 6 Joint surfaces after preparation for arthrodesis.
(From Lee MS, Millward DM. Arthroscopic ankle arthrodesis. Clin Podiatr Med Surg 2009;26:277; with permission.)
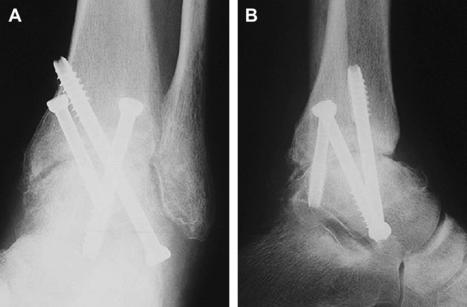
Fixation is achieved with 2 or 3 large-diameter cannulated screws. Typically, one screw is placed from the lateral talar process into the medial tibia, the second from the posterior tibia into the talar neck, and the third (if desired) from the lateral tibia into the posteromedial talus (Fig. 7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree