The ankle is formed by the articular surfaces of the dome of the talus and the distal ends of the fibula and tibia. Motion occurs around the transverse axis through the malleoli.
The ankle is more than a hinge joint that permits motion in only one plane. The primary movements include dorsiflexion (raising the forefoot above the level of the heel) and plantar flexion (lowering the forefoot below the level of the heel).
Average dorsiflexion is 30° and plantar flexion 50°. The working position or neutral position is a right angle (90° angle between foot and calf).
Plantar flexion is important when pushing off in running and jumping activities. It permits standing on the toe in ballet and gymnastics. A contracture with the foot in plantar flexion (an extreme example would be talipes equinus) would interfere with walking and standing. This is why the foot should be immobilized in its 90° working position when applying a cast or taping for various injuries. Dorsiflexion is important for the rolling-off motion.
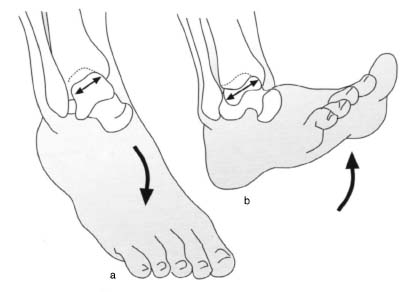
Ankle motion is guided by the mortise formed by the tibia and fibula, which permits a certain degree of lateral motion in extreme plantar flexion. In this position there is a certain amount of play between the mortise and the talus, whose anterior aspect is wider than its posterior aspect (Fig. 6.1).
Fig. 6.1 Motion of the talus within the mortise in plantar and dorsiflexion.
Despite this, the talus is in close contact with the articular surface of the mortise, regardless of the position of the foot. This should be taken into account when treating ankle injuries. This close contact surface must be restored for biomechanical reasons; over time, slight incongruities will result in posttraumatic arthritis with degenerative changes.
If the joint remains in extreme plantar flexion for an extended period of time, the syndesmosis and the capsular ligaments contract, narrowing the mortise and contributing to the equinus contracture mentioned above.
In contrast, extreme dorsiflexion expands the mortise formed by the tibia and fibula, placing tension on the ligaments of the tibiofibular syndesmosis. This dorsiflexion stabilizes the joint in the weight-bearing phase.
A tight syndesmosis connects the distal tibia and fibula, giving the mortise a certain degree of elasticity.
Broad ligaments such as the anterior and posterior tibiofibular ligaments lie along the ankle’s anterior and posterior surfaces and are stressed in extreme dorsiflexion. These ligaments extend horizontally and anteriorly from the lateral malleolus and posteriorly to the talus.
Another major ligament, the calcaneofibular ligament extends vertically from the lateral malleolus to the calcaneus and provides lateral stability.
Insufficiency of a ligament resulting from a tear or sprain produces instability in the ankle. This instability can result in joint incongruity. Extended periods of abnormal weight-bearing can produce degenerative symptoms similar to arthritis.
The capsule of the ankle extends from the cartilage-covered surfaces anteriorly as far as the neck of the talus. Here it fuses with the sheaths of the extensor tendons, preventing impingement of these structures in dorsiflexion.
The weakest point of the joint capsule is its posteromedial aspect. This is often the site of dislocation of the talus.
Thirteen tendons traverse the ankle. The Achilles tendon and the anterior tibial tendons are the structures frequently injured. The peroneal tendons can dislocate from their groove posterior to the lateral malleolus. The tendon of the tibialis posterior passes posterior to the medial malleolus. This tendon is often incarcerated between the talus and malleolus in ankle injuries.
Nerves that transverse the ankle include the saphenous nerve anteromedially, the superficial peroneal nerve in the anterolateral region, and the sural nerve in the posterior region.
The ankle is crucial to walking and standing and is essential for athletic activities. In sports, injuries to the ankle such as ligament injuries and fractures occur frequently.
6.2 Clinical Examination
The stability of the ankle depends on the integrity and interaction of bony structures, ligaments, muscles, and tendons.
Patient History
As in other areas of orthopedics, obtaining a history is the initial step in examining the ankle.
In addition to age-related degenerative changes and occupational stresses, sports in general and stresses specific to particular athletic activities are important. Involvement in sports known for a high incidence of ankle injuries should be identified. This is import for making a diagnosis and for counseling the patient about athletic activities. Sports that involve an increased risk of ankle injury include those that require acceleration and deceleration motions such as volleyball, track and field, basketball, badminton, squash, and gymnastics. Knowledge of the mechanism of injury aids in determining which structures are most susceptible to injury.
The most frequent injuries to the capsular ligaments of the ankle occur as a result of pronation and supination trauma. Depending on the mechanism of injury and the magnitude of the stresses involved, the injury may involve isolated damage to the capsular ligaments or may extend to avulsion injuries of the bone.
Malleolar fractures are usually the result of indirect trauma, and some fracture types always occur in combination with certain ligament injuries or avulsion fractures. There are many classification systems. One system classifies according to the height of fibular involvement – the Danis and Weber system. In this system, knowledge of the mechanism of injury and the height of fibular involvement can provide information about ligament injuries. The general rule is, the higher the fibular fracture, the greater the injury to the tibiofibular ligaments and the greater the danger of insufficiency of the mortise.
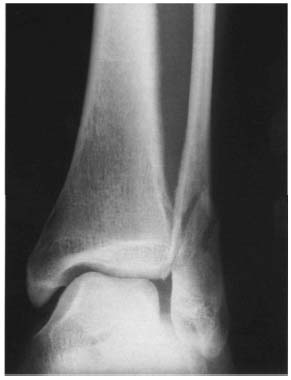
A transverse fracture of the lateral malleolus distal or at the level of the tibial plafond is caused by supination trauma and is classified as a type A injury. The tibiofibular ligaments remain intact (Fig. 6.2). An oblique or spiral fracture of the ankle extending proximally and posteriorly is generally encountered as the result of a pronation eversion injury. At the very least, the ligament injury will include a partial tear of the anterior syndesmosis. This is a type B injury (Fig. 6.27).
A fracture of the fibular shaft proximal to the syndesmosis will always be associated with a tear or avulsion fracture of the ligaments including the interosseous membrane. This type C injury usually severely compromises the stability of the ankle (Fig. 6.3).
In addition to bone and ligament injuries, the possibility of chondral or osteochondral injuries to the articular surfaces must always be considered.
Injuries sustained while jumping or falling from a great height tend to involve complex compression fractures of the distal tibia, although torsional trauma will more likely produce fractures of the malleoli or ligament injury. Distal tibial fractures involving the articular surface are referred to as “pilon fractures.”
Many ankle fractures may be treated with closed methods. The choice of open or closed treatment is less important than the quality of the reduction obtained. A nonanatomical reduction will have a bad outcome, even if it was attained with open methods.
The most favorable time for surgical treatment of malleolar fractures is within the first 6–8 hours after injury. If this time frame is exceeded or if severe swelling is present (possibly including fracture blisters), surgical treatment should be delayed approximately 6–8 days.
The goal of treatment is to restore the anatomy and stability of the articular surface.
Observation
When inspecting the ankle, abnormalities in shape and changes in the contour of the various regions may be distinguished. Causes may include soft-tissue swelling, sequelae of fractures, sequelae of infections, or intra-articular effusion.
Fig. 6.2 Type A malleolar fracture according to Weber and Danis.
Fig. 6.3 Type C malleolar fracture according to Weber and Danis.
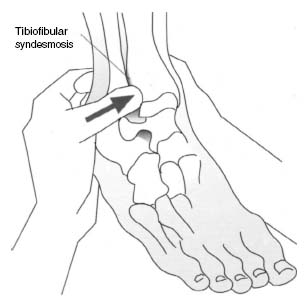
Fig. 6.4 Palpation of the tibiofibular syndesmosis.
If swelling is present, document whether it is diffuse or localized and unilateral or bilateral. Bilateral edema suggests a systemic cause.
Inspection will also reveal any open lesions such as scrapes or open fractures.
Palpation
To palpate the ankle, have the patient sit on the edge of the examining table with the legs dangling. Immobilize the patient’s foot and calf with one hand, grasping the calcaneus. Palpation of both bony structures and soft tissue should be documented.
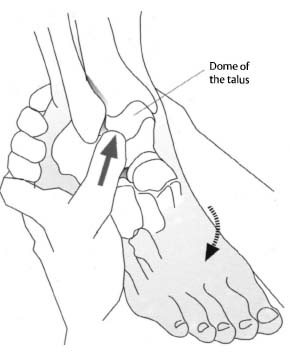
Thickening of the joint capsule medial and lateral to the extensor tendons can be evaluated by palpation. Examine local areas of tenderness such as above the distal syndesmosis (Fig. 6.4), the deltoid ligament, and the lateral fibular ligaments. In extreme plantar flexion, part of the talar dome is accessible to palpation on the medial side of the foot proximal to the navicular (Fig. 6.5). Tenderness to palpation may be caused by traction osteophytes, osteochondritis dissecans, or degenerative changes. Continue the examination proximally, palpating the medial malleolus (Fig. 6.6). The deltoid ligament will be palpable immediately beneath the malleolus (Fig. 6.7). This strong, broad ligamentous structure compensates for the short length of the medial malleolus compared with the lateral malleolus. Tenderness to palpation in this region suggests ligament injury.
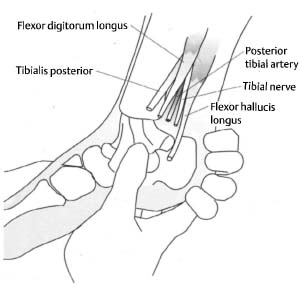
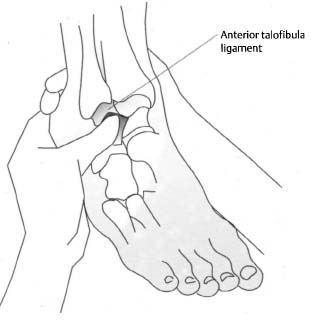
Localized tenderness to palpation immediately above the joint space and at maximum dorsiflexion of the foot with slight lateral migration of the fibula is the sign of an injury to the anterior talofibular ligament (Fig. 6.8). On the posterior aspect of the medial malleolus, several structures can be palpated in a small groove medial to the Achilles tendon. These include, from anterior to posterior, the tendons of the tibialis posterior and flexor digitorum longus muscles, the posterior tibial artery and nerve, and the flexor hallucis longus (Fig. 6.7). If tenosynovitis in this region is suspected, check for tenderness to palpation and for swelling along the tendons (Fig. 6.9). Another sign of tenosynovitis is pain that occurs when the foot is in plantar flexion and pronation (Fig. 6.10). In this position, tenderness to palpation and a palpable defect in the tibialis posterior tendon will be encountered in a tear (Fig. 6.11).
Fig. 6.5 Palpation of the talar dome in plantar flexion.
Fig. 6.6 Palpation of the medial malleolus.
Fig. 6.7 Palpation of the deltoid ligament.
Fig. 6.8 Palpation of the anterior talofibular ligament.
The thick cord of the Achilles tendon is located further posteriorly and medially.
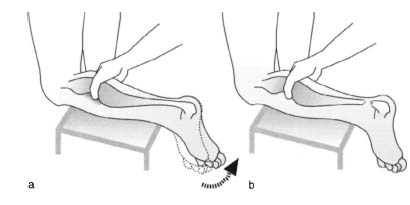
To evaluate the Achilles tendon, the patient is prone with the feet extending past the edge of the examining table. Evaluate strength and integrity by having the patient actively bring the feet into plantar flexion against your resistance. Observe and palpate the tensing of the tendons. If a tear is present, a loss of strength and a change in the contour of the tendon will be noticeable on the affected side (Figs. 6.12a, b).
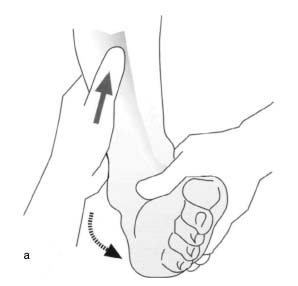
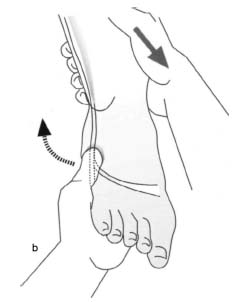
If the Achilles tendon is intact, compressing the calf will produce plantar flexion. Absence of plantar flexion in this test is a sign of a tear in the Achilles tendon (Figs. 6.13a, b).
The lateral malleolus is palpated at the distal tip of the fibula. The anterior talofibular ligament, calcaneofibular ligament, and the posterior talofibular ligament are important stabilizing structures that are palpable in this region. These structures are frequently injured in supination trauma.
Fig. 6.9 Palpation of the tendons of the tibialis posterior, flexor digitorum longus, flexor hallucis longus, and posterior tibial artery.
Fig. 6.10 Pain in passive plantar flexion and pronation of the foot with tenosynovitis of the tibialis posterior tendon.
Fig. 6.11 Palpation of the tibialis posterior tendon for tenderness in tenosynovitis or a palpable defect in a tear.
Figs. 6.12a, b Palpation of the Achilles tendon and evaluation of active strength in both ankles.
The anterior talofibular ligament is tensed in the foot in plantar flexion and supination.
The calcaneofibular ligament inserts on the calcaneus toward the plantar aspect of the foot. Usually, it is only affected in severe ankle trauma after injury to the anterior talofibular ligament.
Figs. 6.13a, b Evaluating the integrity of the Achilles tendon by compressing the calf.
The posterior talofibular ligament is the strongest of the lateral ankle ligaments. It stabilizes the ankle as the talus moves anteriorly and is usually only damaged in high-energy injuries.
The peroneal ligaments can be palpated at the lateral malleolus. These will be tender to palpation if tenosynovitis is present. Extreme passive inversion and plantar flexion will also cause pain in the peroneal tendons with tenosynovitis (Fig. 6.14).
In dislocation of the peroneal tendons, there will be a palpable snap anterior to the malleolus as the patient actively pronates the foot (Fig. 6.15).
Fig. 6.14 Passive strong plantar flexion and inversion intensifies pain in tenosynovitis of the peroneal tendons.
Fig. 6.15 Palpation of the peroneal tendons while the patient actively pronates the foot in peroneal tendon dislocation.
Fig. 6.16 Evaluating posterior extension in shortening of the Achilles tendon.
Assessing Range of Motion
As with every joint, range-of-motion testing for the ankle evaluates the active and passive ranges of motion.
Motion is measured around the main axis. This axis connects the medial and lateral malleoli through the talus. It permits lifting of the foot (dorsiflexion) and lowering of the foot (plantar flexion). The range of motion is measured and documented using the neutral-O method.
Assessing Active Range of Motion
To examine plantar flexion, instruct the patient to walk a short distance on tiptoe. Walking on the heels is used for evaluating dorsiflexion.
Assessing Passive Range of Motion
To evaluate the passive range of motion of the ankle, have the patient sit on the examining table with the legs dangling. In this position with the knees flexed 90°, the action of the gastrocnemius is minimized, permitting unimpeded evaluation of dorsiflexion even in the presence of a shortened Achilles tendon (Fig. 6.16).
Pressing the foot downward produces plantar flexion. Normally the range of motion according to the neutral-O method will be 30° dorsiflexion and 50° plantar flexion.
Specific Tests
These tests permit a rough estimation of the severity of an injury.
According to the direction of motion, a distinction is made between pronation and supination trauma of the ankle. Supination trauma, i.e., trauma in which the medial aspect of the foot bends upward beyond the patient’s control, is more common for anatomic reasons. Since the medial malleolus is shorter than the lateral malleolus, the talus tends to supinate rather than pronate. The lateral ligaments as isolated structures are not as strong as the deltoid ligament.
All specific tests can be performed under local anesthesia to neutralize reflexive muscle tensing by the patient if the pain is too great.
Specific Tests for Instability
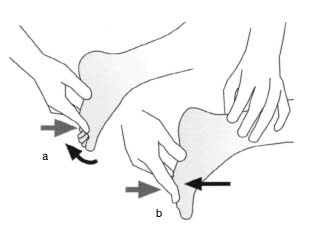
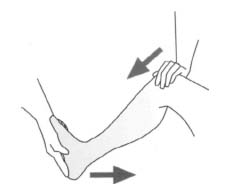
Anterior drawer (Figs. 6.17a, b). Anterior drawer is best evaluated with the patient supine. Immobilize the patient’s distal tibia with one hand while holding the back of the foot with the other. Now apply pressure against the back of the foot. Repeat the test for both sides. A positive test is the sign of injury to the anterior and posterior capsular ligaments of the ankle.
In an isolated tear of the talofibular ligament, the talus can be shifted anteriorly against the tibia. This ligament does not allow such mobility when intact. This test may also be documented in radiographic and ultrasound studies.
Figs. 6.17a, b Evaluating the anterior drawer of the talus.
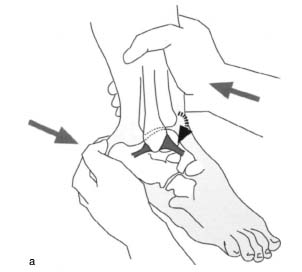
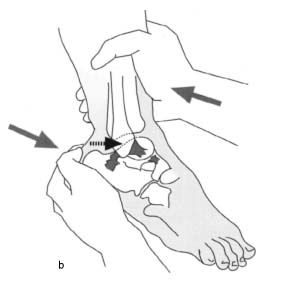
Figs. 6.18a, b Evaluating lateral and medial opening.
Lateral and medial opening (Figs. 6.18a, b). This may also be known as talar tilt. It is also best tested with the patient supine and relaxed. Again, examine both sides for comparison. Apply a varus and valgus stress to the ankle to evaluate the lateral and medial capsular ligaments.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree